Around 90% of nonmelanoma skin cancers arise on the head and neck and about 10% of these occur in the area of the eyelids.1 Surgery continues to be the treatment of choice,2 but concerns about the risk of postoperative complications, local recurrence, or a poor cosmetic and functional outcome have led to the investigation of alternative options, such as cryotherapy, radiation therapy, chemotherapy, retinoids, topical immunomodulators, and photodynamic therapy (PDT). The choice of treatment will depend on the age of the patient, the site and size of the tumor, and the experience of the dermatologist.
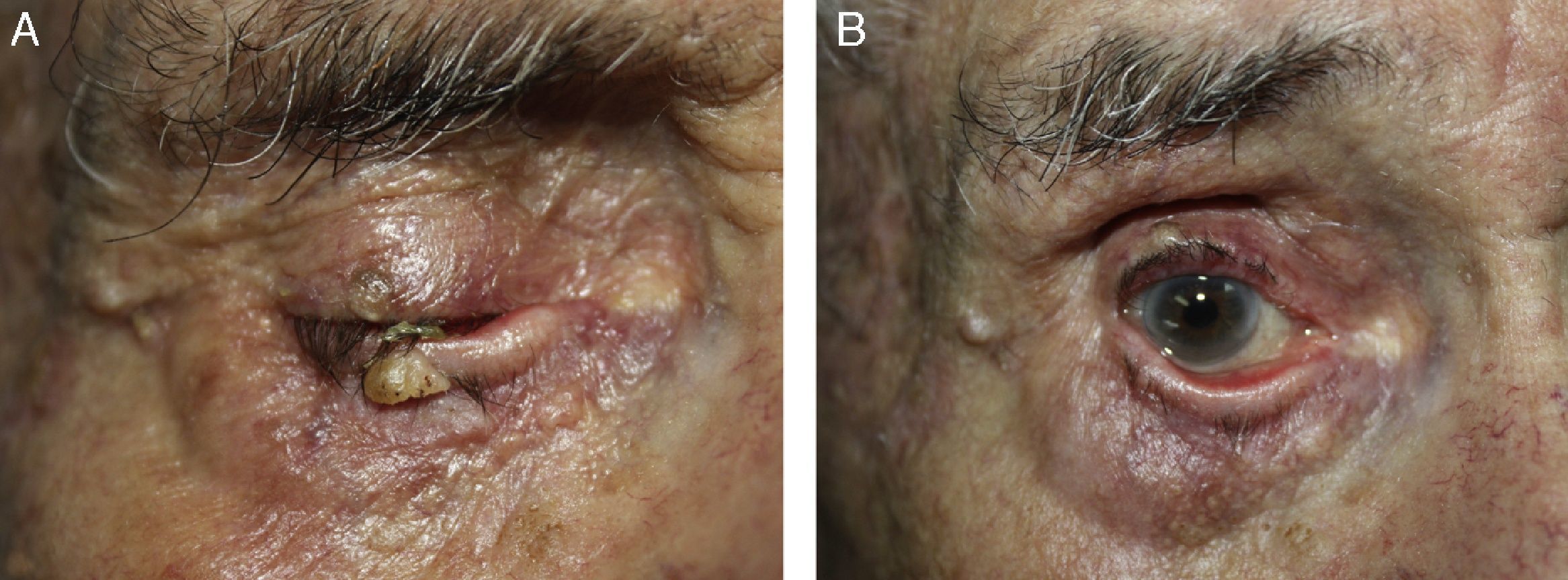
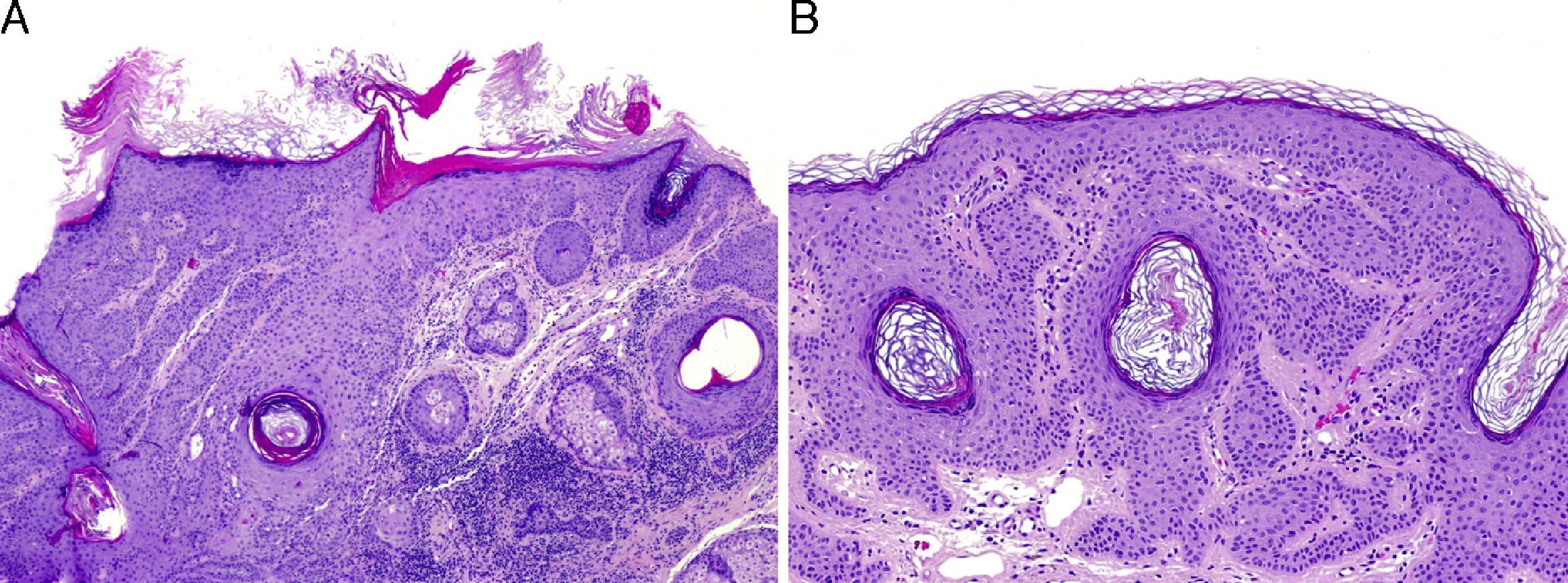
We present the case of an 82-year-old man who was seen for a desquamating, partially exophytic erythematous plaque of 1.5cm in diameter that had developed on the right lower eyelid and affected the free border (Fig. 1A). Biopsy showed the lesion to be an actinic keratosis (Fig. 2A). Photodynamic therapy (PDT) was chosen for treatment in accordance with the recommended protocol for the treatment of basal cell carcinoma.3,4 Topical methyl 5-aminolevulinate cream (Metvix) was applied to the lesion. The cream was removed after 3hours and uptake by the lesion was confirmed with the aid of a Wood lamp. A sterile, opaque black plastic shield was used to protect the eye; topical anesthetic eye drops (0.1% tetracaine hydrochloride plus 0.4% oxybuprocaine hydrochloride) should be instilled into the eye 5minutes before inserting the shield, and a viscoelastic substance such as Gonioftal gel (latex-free hydroxyethylcellulose) should be used to minimize contact with the surface of the eye. The lesion was infiltrated with local anesthetic (1% mepivacaine) and then illuminated using a light-emitting diode lamp with a wavelength of 634nm (Aktilite; PhotoCure, Galderma), administering 37J/cm2 over a period of 8minutes at a distance of 10cm. The patient's sensation of burning was reduced by the application of fine sprays of thermal water or liquid nitrogen from a distance. After completing the treatment session, we removed the shield by pulling down on the lower eyelid, thus minimizing the risk of corneal injury, and the patient was prescribed chloramphenicol eye drops for administration every 8hours for the first 3 days. A second treatment session was performed 2 weeks later. The therapy was well tolerated and in the treated area there was only mild erythema and edema, which resolved within a few days.
A, Histology showing the presence of hyperkeratosis alternating with parakeratosis and atypical keratinocytes occupying part of the thickness of the epidermis. B, Histology of the residual lesion. Observe the presence of epidermal acanthosis and corneal pseudocysts typical of seborrheic keratosis.
There was a marked reduction in the size of the lesion. Subsequent treatment with imiquimod 5% cream 3 times a week for 4 weeks produced no inflammation or improvement, and curettage biopsy was therefore performed for histological study, with electrocoagulation of the residual lesion (Fig. 1B). The biopsy revealed only seborrheic keratosis (Fig. 2B).
The incidence of actinic keratosis on the eyelids has increased in the last 2 decades. PDT has been shown to be effective in the treatment of basal cell carcinoma, actinic keratosis, and Bowen disease. A recently published case series described the effectiveness of PDT for patients with tumors on the eyelids.1 The authors of that report recommended initial curettage of the lesion, the use of topical methyl 5-aminolevulinate, and repetition of the treatment after a week. PDT offers better cosmetic and functional results and is associated with a lower morbidity and cost than surgery.5 One of the important limitations of this treatment is the risk of phototoxic eye damage and the need for follow-up due to the long-term risk of recurrence.
Another effective therapeutic option in selected cases is topical imiquimod 5% cream. Its application 5 times a week for 6 weeks has been shown to be effective in the treatment of periocular tumors.6 However, its use is controversial in tumors situated at less than 5mm from the free border of the eyelid because of the possibility of local adverse effects.
Our patient presented a satisfactory clinical course after PDT, with only a residual seborrheic keratosis that remained present after treatment. In conclusion, we must insist that tumors in the area of the eyelids are a therapeutic challenge for the dermatologist. Surgery continues to be the treatment of choice for tumors situated in areas difficult to treat, but PDT is an effective, noninvasive therapeutic alternative that is well tolerated by the patient and that offers good cosmetic and functional results, as we have shown with the case presented.
Please cite this article as: Toledo- Alberola F, et al. Terapia fotodinámica como respuesta al reto de tratar una queratosis actínica en el área palpebral. Actas Dermosifiliogr. 2012;103:938–9.