The term primary cutaneous angioplasmocellular hyperplasia was proposed in 1995 to describe skin lesions characterized histologically by a vascular proliferation associated with a polyclonal inflammatory infiltrate of plasma cells; such lesions were first described on the trunk of young adults.1 We present a case of this rare condition.
A 40-year-old man with no past history of interest and who did not smoke or drink consulted for an asymptomatic lesion that had been present on his chest for 2 months. He did not recall a previous injury, insect bite, or pre-existing lesion. Physical examination revealed an erythematous-violaceous nodule measuring 2.5×2cm on the anterior aspect of the chest (Fig. 1). The nodule was firm, was not adherent to deeper planes and did not blanch on pressure. There was a central ulcer that was covered by fibrin. Nothing remarkable was found on examination of the rest of the skin and the patient was in a good general state of health.
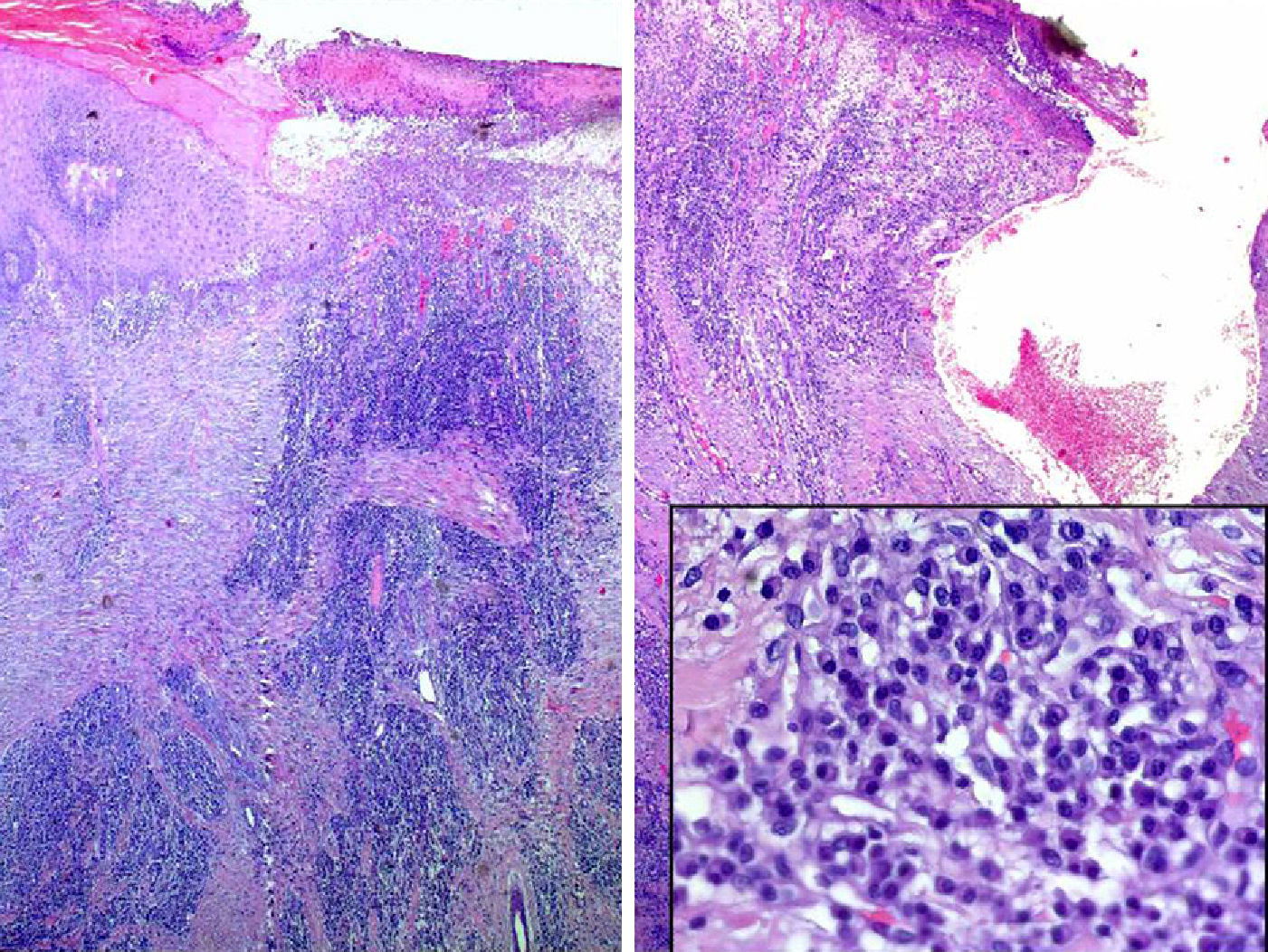
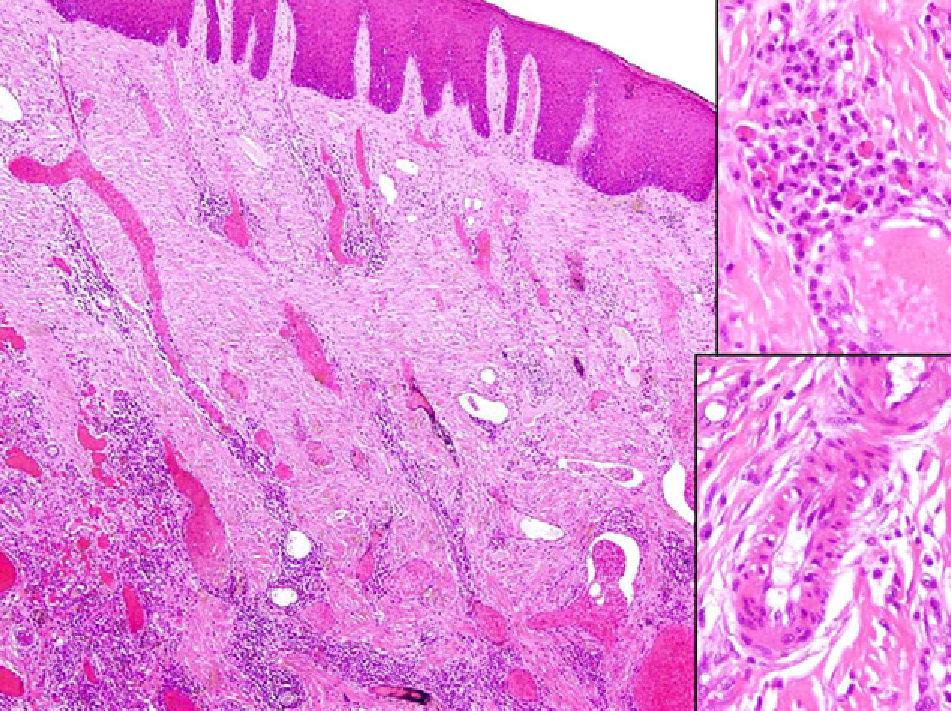
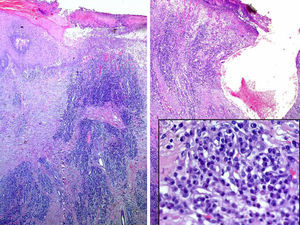
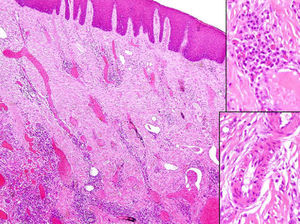
An incisional biopsy that included the border and center of the lesion revealed partial ulceration and epidermal hyperplasia with moderate acanthosis. A vascular proliferation constituted predominantly by thin-walled capillaries was observed in the reticular and papillary dermis (Fig. 2). A mainly perivascular inflammatory infiltrate formed principally of plasma cells with no atypia or mitoses was also observed; immunohistochemistry showed this to be a polyclonal infiltrate. Tissue culture and periodic acid-Schiff, Giemsa, and Warthin-Starry stains were negative. It was decided to excise the complete lesion. Histology confirmed the earlier biopsy findings and revealed the presence of Russell bodies. The vessels were dilated capillaries and venules. Some of the capillaries presented a prominent endothelium and focal endothelial vacuolization (Fig. 3). Additional tests, including complete blood count, biochemistry, coagulation studies, immunoglobulins, protein electrophoresis, antinuclear antibodies, and complement, were normal or negative. Serology was negative for syphilis and Lyme disease. Urinary protein electrophoresis and the chest x-ray presented no abnormal findings.
A diagnosis of primary cutaneous angioplasmocellular hyperplasia was made on the basis of the clinical and histological characteristics of the lesion and the results of the additional tests.
The patient presented no recurrence or systemic involvement after 9 months of follow-up.
The majority of reports of primary cutaneous angioplasmocellular hyperplasia involve single patients,2,3 with the exception of the series published by Hsiao et al.4 The condition is characterized clinically by erythematous-violaceous or brownish papules or nodules measuring between a few millimeters and 2 to 3 cm in diameter and that occur most commonly on the head and trunk. The lesions are usually single, though a case in which the patient had 2 simultaneous lesions has been reported.4 Central ulceration and a peripheral erythematous halo are common findings. No trigger factor has been identified, although a relationship with previous injury or with varicella has been described in some cases.4 At the time of diagnosis, the lesions may have been present for weeks to years.1,3,4 Histologically these lesions are characterized by a central ulcer with peripheral epidermal hyperplasia with acanthosis and a variable degree of hypergranulosis. In the dermis there is a proliferation of dilated capillaries and venules and an inflammatory infiltrate formed predominantly of polyclonal plasma cells with no atypia or mitoses. Although the infiltrate tends to be perivascular in early lesions, it acquires an interstitial distribution in more advanced lesions. Though cell proportions are variable, plasma cells make up more than 60% of the infiltrate; lymphocytes, neutrophils, and eosinophils are present in small numbers. Foci of prominent endothelial cells with no atypia or mitoses and of endothelial vacuolization are common.
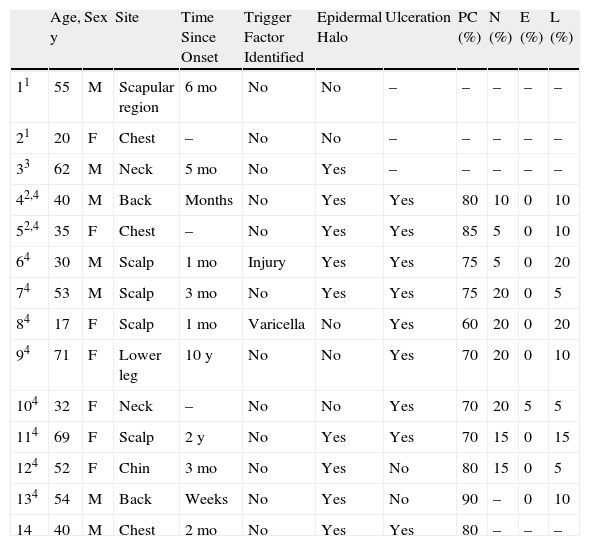
The clinical and histological characteristics of previously reported cases and of our patient are presented in Table 1. The presence of Russell bodies—homogeneous, intensely eosinophilic structures formed of immunoglobulins secreted by plasma cells—has not been described in any of the previously published cases, but they may be observed in lesions with a marked plasma cell component, whether reactive or neoplastic.5
Clinical and Histological Characteristics of Published Cases.
| Age, y | Sex | Site | Time Since Onset | Trigger Factor Identified | Epidermal Halo | Ulceration | PC (%) | N (%) | E (%) | L (%) | |
| 11 | 55 | M | Scapular region | 6mo | No | No | – | – | – | – | – |
| 21 | 20 | F | Chest | – | No | No | – | – | – | – | – |
| 33 | 62 | M | Neck | 5mo | No | Yes | – | – | – | – | – |
| 42,4 | 40 | M | Back | Months | No | Yes | Yes | 80 | 10 | 0 | 10 |
| 52,4 | 35 | F | Chest | – | No | Yes | Yes | 85 | 5 | 0 | 10 |
| 64 | 30 | M | Scalp | 1mo | Injury | Yes | Yes | 75 | 5 | 0 | 20 |
| 74 | 53 | M | Scalp | 3mo | No | Yes | Yes | 75 | 20 | 0 | 5 |
| 84 | 17 | F | Scalp | 1mo | Varicella | No | Yes | 60 | 20 | 0 | 20 |
| 94 | 71 | F | Lower leg | 10 y | No | No | Yes | 70 | 20 | 0 | 10 |
| 104 | 32 | F | Neck | – | No | No | Yes | 70 | 20 | 5 | 5 |
| 114 | 69 | F | Scalp | 2 y | No | Yes | Yes | 70 | 15 | 0 | 15 |
| 124 | 52 | F | Chin | 3mo | No | Yes | No | 80 | 15 | 0 | 5 |
| 134 | 54 | M | Back | Weeks | No | Yes | No | 90 | – | 0 | 10 |
| 14 | 40 | M | Chest | 2mo | No | Yes | Yes | 80 | – | – | – |
Abbreviations: E, eosinophils; F, female; L, lymphocytes; M, male; N, neutrophils; PC, plasma cells.
Plasma cells are not common in healthy skin, though they are much more prevalent in mucosas. Their numbers also increase in areas of infected or injured skin. Infections such as leprosy, chronic folliculitis, syphilis, leishmaniasis, and bacillary angiomatosis are associated with a more intense plasma cell infiltrate; serology and specific stains are useful to reach a diagnosis in such cases. Other conditions to be considered in the differential diagnosis include the pseudolymphomas and reactions to arthropod bites,1 which are clinically similar but histologically different, presenting a dense perivascular lymphocytic inflammatory infiltrate with lymphoid follicles and isolated plasma cells.
Neoplastic infiltrates of plasma cells are observed in extramedullary cutaneous plasmacytoma (primary or secondary to myeloma), but the cells are monoclonal4,6 and the vascular component is minimal.
Among the dermatoses with a predominantly vascular component, the most important disease that must be included in the differential diagnosis is pyogenic granuloma, which has a lobular histologic pattern that is not present in angioplasmocellular hyperplasia. The vessels in pyogenic granuloma are of smaller size and the infiltrates are formed mainly of lymphocytes, although they can contain plasma cells in ulcerated or long-standing lesions.1,3,4 In the histological differential diagnosis we should also considered angiolymphoid hyperplasia with eosinophilia,4 Kaposi sarcoma,7 epithelioid hemangioendothelioma,1 and cutaneous epithelioid angiomatous nodule.8
In summary, we have presented a new case of a patient with a lesion on the center of the chest with the clinical and histological characteristics described to date for primary cutaneous angioplasmocellular hyperplasia. Our patient's lesion was large and contained Russell bodies, a finding not previously described in this condition.
In agreement with other authors, we consider this to be a reactive hyperplasia, although no triggering stimulus can be found in the majority of cases.
Please cite this article as: Ramírez-Santos A, Pérez-Valcarcel J, Suárez-Amor OM, González-Vilas D. Hiperplasia angioplasmocelular cutánea primaria. Actas Dermosifiliogr.2012;103:739-741.