A 14-year-old boy with no relevant past medical history presented with a lesion on the upper gum that had developed 6 weeks previously. The patient reported that the lesion had grown progressively, resulting in increasing discomfort and slight bleeding caused by friction.
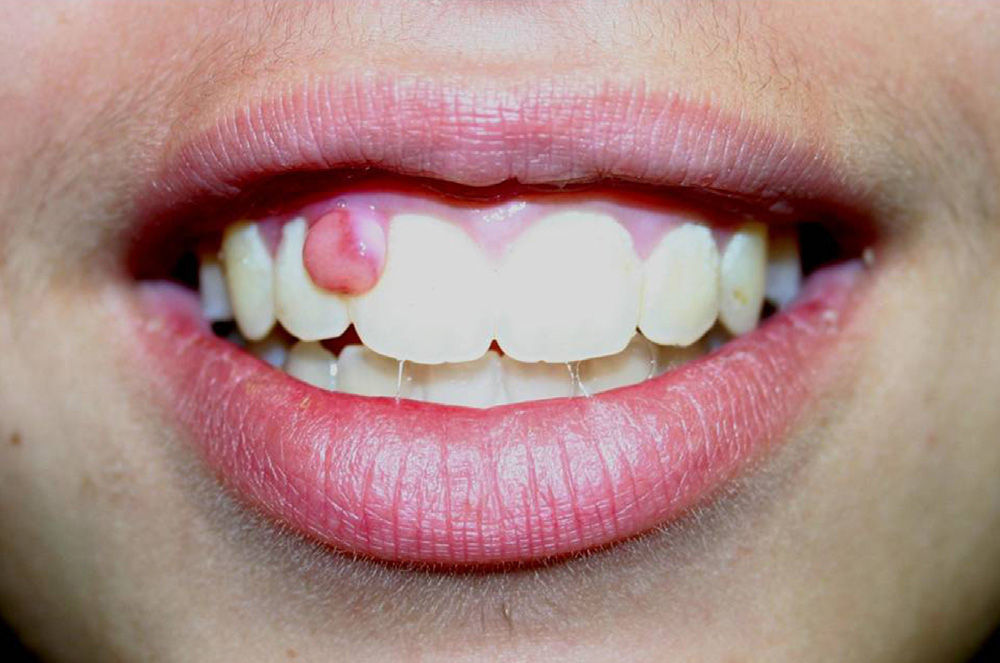
Physical ExaminationPhysical examination revealed a 5-mm polypoid lesion of normal mucosal color and firm rubbery consistency located between the medial and lateral incisors of the upper right gum (Fig. 1). No movement or alterations of the teeth were observed, nor were any other lesions detected in either the oral cavity or the cervical region. Curettage of the lesion was performed, followed by hemostasis with silver nitrate.
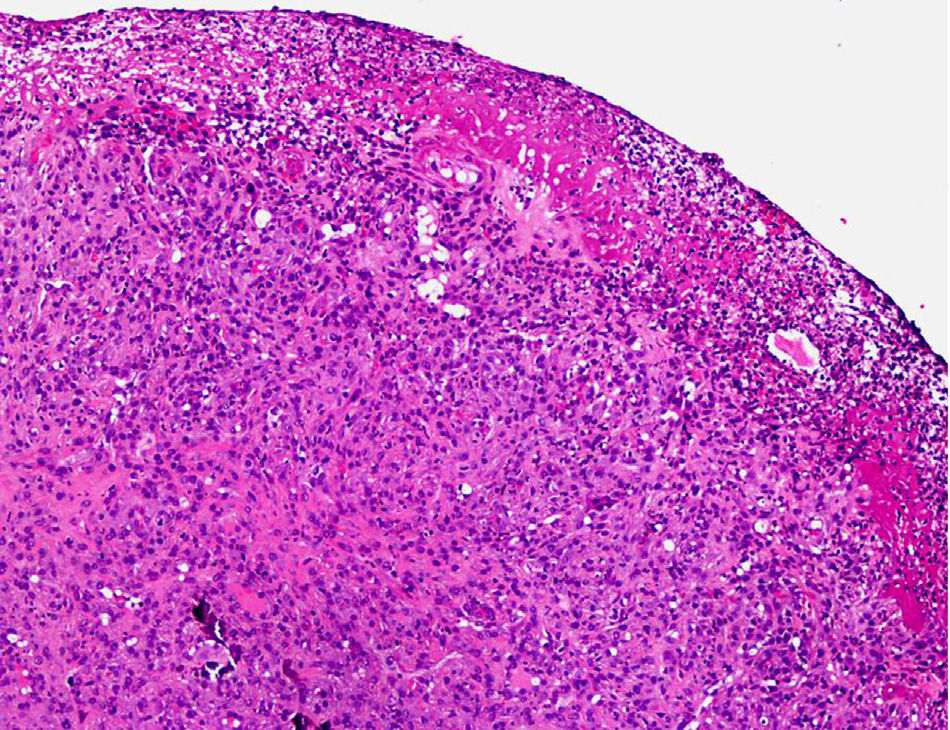
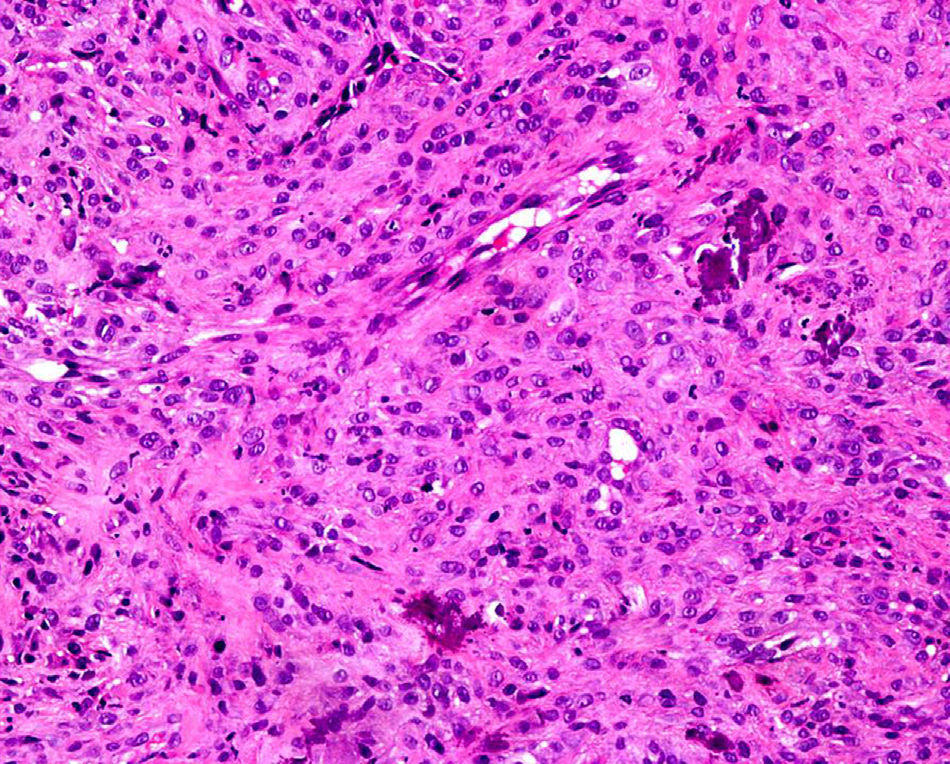
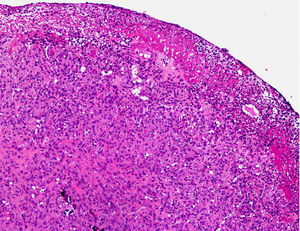
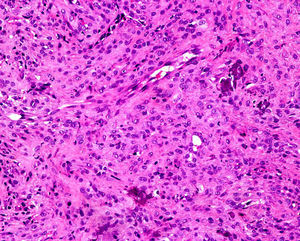
HistologyHistology showed fibrous tissue with prominent fusiform fibroblasts, among which lamellar bone trabeculae were dispersed (Figs. 2 and 3). Immunohistochemistry revealed that the cell population was positive for vimentin and had a mean Ki-67 value of 23%, but was negative for the markers CD31, CD34, von Willebrand factor, cytokeratin AE1/AE3, epithelial membrane antigen, smooth muscle actin, muscle-specific actin, desmin, CD68, and S-100 protein.
What Is Your Diagnosis?
DiagnosisPeripheral cemento-ossifying fibroma (PCOF).
Clinical Course and TreatmentTwo weeks after treatment the appearance of the gum had improved, with no recurrence or residual lesion.
CommentPCOF is a fibro-osseous, osteogenic, reactive hyperplasia. Its likely origin is the multipotent cells of the periodontal ligament, given its near-exclusive localization in the gums, the inverse relationship between age and incidence, and the presence of oxytalan fibers in the calcified matrix in some PCOF cases. While the pathogenesis of PCOF is unknown, this condition has been associated with trauma, the presence of ectopic remnants of the periodontal ligament, and the influence of female sex hormones and chronic irritants, including dental calculus, plaque, ill-fitting dentures, malpositioned teeth, and irregular dental restorations.1 Chronic irritation of the periosteum and periodontium result in the formation of reactive granulation tissue, which ultimately calcifies and undergoes fibrosis.2
PCOF is rare, with a higher incidence in white women in their second or third decade of life, and accounts for 3.1% of biopsied oral tumors.1,2
It presents as a slow-growing, asymptomatic lesion in most cases, although large lesions resulting in facial asymmetry or the displacement of adjacent teeth have been described.1 Physical examination reveals a firm, erythematous, sessile or pedunculated tumor of normal mucosal color and of less than 2cm in diameter, located in the interdental papilla.1 In most cases these tumors develop in the upper maxilla.3
Diagnosis is based on clinical-radiologic-pathologic correlation.4 Histologically, PCOF is a nonencapsulated lesion composed of connective tissue, abundant large fibroblasts, and chronic inflammatory cells, and covered by intact or ulcerated stratified, nonkeratinizing, squamous epithelium. These tumors contain a laminar osteoid-like mineralized material, cement-like concretions, or a mixture of both. Radiography is the imaging test of choice, and reveals a radiolucent, radiopaque, or mixed-density mass that does not affect the underlying bone. Superficial bone erosion, central radiopaque foci, widening of the periodontal ligament, or dental displacement may also be observed.1,5
The differential diagnosis is established based on clinical-pathological correlation and includes other localized reactive gingival hyperplasias such as pyogenic granuloma, gingival fibroma, and peripheral giant cell granuloma; benign conditions such as fibrous dysplasia or osteomyelitis; and bone tumors, both benign (osteoid osteoma, osteoblastoma, cementoblastoma) and malignant (osteosarcoma).1,4,6 Juvenile ossifying fibroma, a variant of PCOF with a worse prognosis, was ruled out in our patient.
Treatment consists of excision of the lesion and deep curettage of the periosteum and periodontal ligament, with recurrence in 8% to 30% of cases depending on the series,2 probably due to inadequate curettage and the persistence of chronic irritants. Malignant transformation has not been described.4
Dermatologists should be familiar with this entity in order to ensure correct differential diagnosis and to avoid unnecessary tests and procedures.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Puente N, Castaño Á, Hernández-Núñez A. Lesión polipoide en la encía. Actas Dermosifiliogr. 2014;105:947–948.