Although the existence of photodistributed erythema multiforme has been recognized for years, few cases have been described to date. It is an uncommon, and probably underdiagnosed, skin disorder that can affect individuals of both sexes and all ages. It has been associated with drugs, reactivation of herpes simplex virus infection, and polymorphous light eruption. A diagnosis is made on the basis of history, physical examination, histology, and phototesting. The condition runs a benign, self-limiting course but patients may experience outbreaks for several years if the causative agent is not eliminated. It is treated symptomatically and patients are advised to avoid triggers and excessive sun exposure.
A pesar de que la fotodistribución del eritema multiforme se conoce desde hace muchos años, pocos casos de eritema multiforme fotodistribuido (EMF) han sido descritos hasta la fecha. El EMF es una dermatosis infrecuente, y probablemente infradiagnosticada, que puede afectar a sujetos de ambos sexos y de todas las edades. Se ha relacionado con fármacos, reactivaciones del virus herpes simple y erupción polimorfa lumínica. Su diagnóstico se basa en la anamnesis, la exploración física, la histopatología y el estudio fotobiológico. Su curso es benigno y autolimitado, pero pueden aparecer brotes durante varios años si no se suprime el agente causal. Se trata de forma sintomática, evitando los desencadenantes y adoptando medidas de fotoprotección.
Erythema multiforme (EM) is an acute mucocutaneous syndrome that runs a self-limiting, usually mild, course. It is considered a hypersensitivity reaction to different antigenic stimuli, the most common of which is herpes simplex virus (HSV).1–5 It is clinically characterized by a polymorphous eruption of crops of erythematous macules and papules that tend to be symmetric and located predominantly in acral regions. The most characteristic lesions, known as target or iris lesions, are round, erythematous, edematous papules with concentric color variations. The condition is known as erythema multiforme because patients have lesions at different stages of development.6
EM is classified among the photoaggravated or photoaccentuated dermatoses.6,7 These are different from other photodermatoses in that they can also occur in the absence of exposure to UV radiation or visible light; indeed, only a few individuals experience eruptions triggered by light.8,9 In some cases, the lesions are confined to sun-exposed areas, with a clear division between these and unexposed areas. This explains why the use of the term photodistributed (or photosensitive) erythema multiforme (PEM) is justified.10,11 In our review of the literature, we identified 18 cases of PEM. The triggers identified were HSV reactivation,12–14 drug use,11,15–22 and polymorphous light eruption (PMLE).23,24 In this article, we review the epidemiologic, clinical, etiologic, diagnostic, and therapeutic aspects of PEM.
EpidemiologyThe prevalence of EM and PEM is unknown. EM is a relatively common condition, and while the existence of PEM has been recognized for many years,10,14 few cases have been described, possibly due to its low prevalence or to the fact that many cases go undiagnosed.
PEM affects individuals of both sexes and all ages. In the cases reported in the literature, the mean age at diagnosis was 41.7 years, with a range of 9 to 75 years. In the case of HSV-associated PEM, the mean age was considerably lower, at 15 years (range, 9-25 years) while in that of drug-induced PEM, it was higher (53.9 years; range, 36-75 years). PEM secondary to PMLE and idiopathic PEM were observed in middle-aged individuals. Overall, there was a slight male predominance (male to female ratio of 10:8). Approximately 39% of patients with PEM experience recurrences, particularly when there is associated HSV infection or no identifiable cause.
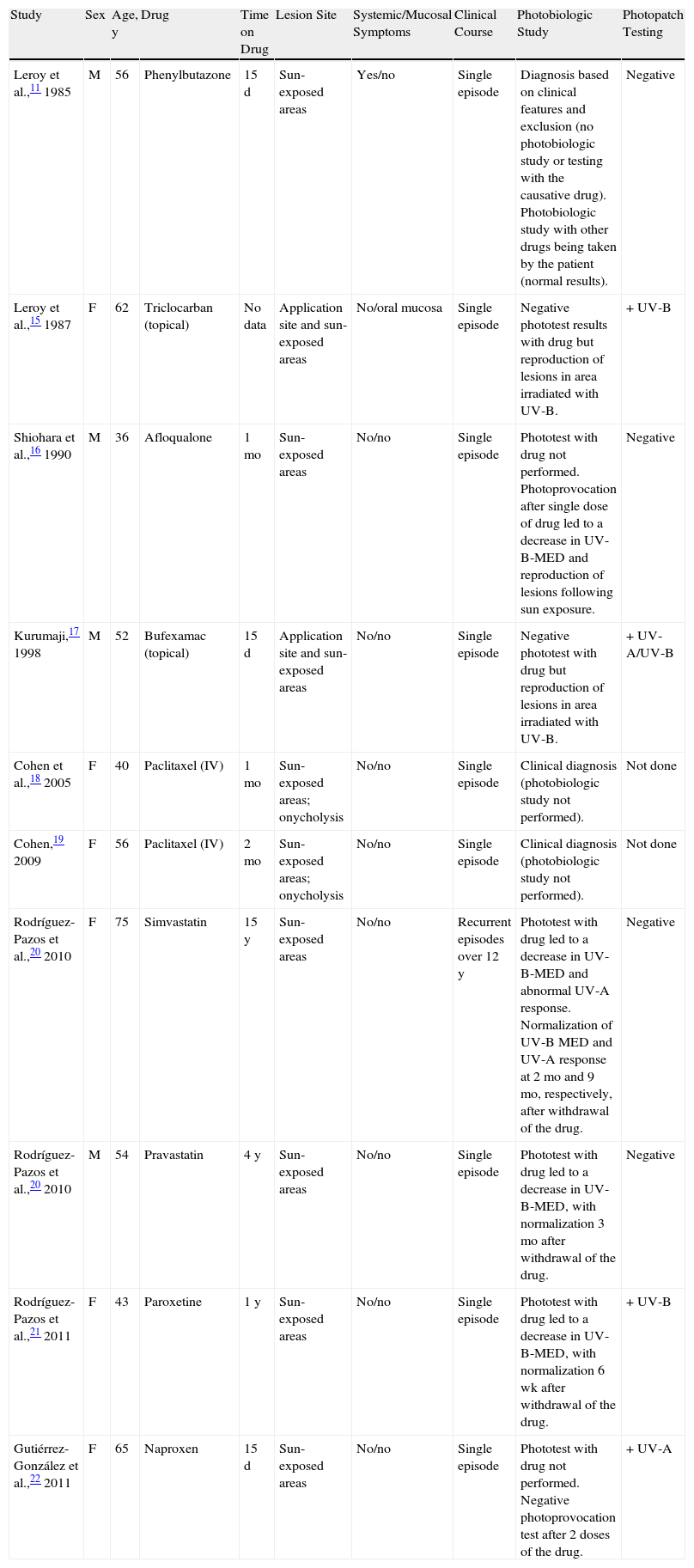
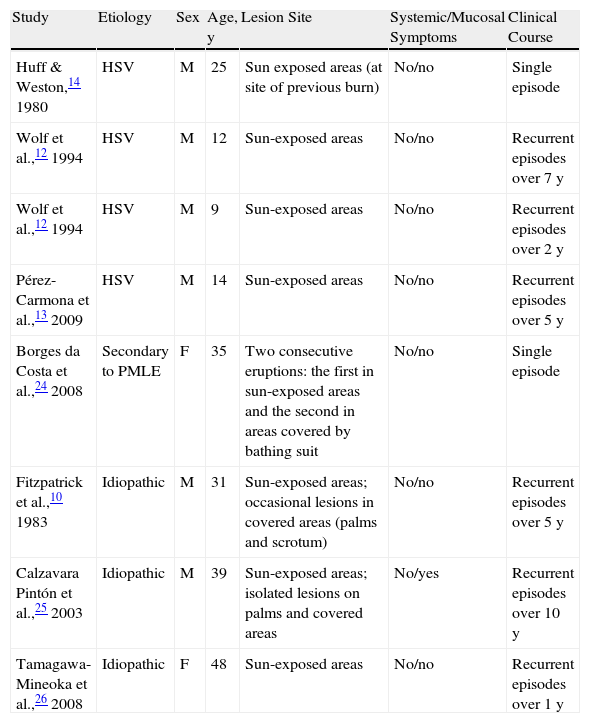
EtiologyPEM has been described in association with drugs, HSV infection, and other conditions, such as PMLE (Tables 1 and 2). Of the cases described to date, 55.5% were induced by drugs, 22.2% by HSV reactivation, and 5.5% by PMLE. The remaining cases were classified as idiopathic.
Cases of Drug-Induced Photodistributed Erythema Multiforme in the Literature.
| Study | Sex | Age, y | Drug | Time on Drug | Lesion Site | Systemic/Mucosal Symptoms | Clinical Course | Photobiologic Study | Photopatch Testing |
| Leroy et al.,11 1985 | M | 56 | Phenylbutazone | 15 d | Sun-exposed areas | Yes/no | Single episode | Diagnosis based on clinical features and exclusion (no photobiologic study or testing with the causative drug). Photobiologic study with other drugs being taken by the patient (normal results). | Negative |
| Leroy et al.,15 1987 | F | 62 | Triclocarban (topical) | No data | Application site and sun-exposed areas | No/oral mucosa | Single episode | Negative phototest results with drug but reproduction of lesions in area irradiated with UV-B. | +UV-B |
| Shiohara et al.,16 1990 | M | 36 | Afloqualone | 1 mo | Sun-exposed areas | No/no | Single episode | Phototest with drug not performed. Photoprovocation after single dose of drug led to a decrease in UV-B-MED and reproduction of lesions following sun exposure. | Negative |
| Kurumaji,17 1998 | M | 52 | Bufexamac (topical) | 15 d | Application site and sun-exposed areas | No/no | Single episode | Negative phototest with drug but reproduction of lesions in area irradiated with UV-B. | +UV-A/UV-B |
| Cohen et al.,18 2005 | F | 40 | Paclitaxel (IV) | 1 mo | Sun-exposed areas; onycholysis | No/no | Single episode | Clinical diagnosis (photobiologic study not performed). | Not done |
| Cohen,19 2009 | F | 56 | Paclitaxel (IV) | 2 mo | Sun-exposed areas; onycholysis | No/no | Single episode | Clinical diagnosis (photobiologic study not performed). | Not done |
| Rodríguez-Pazos et al.,20 2010 | F | 75 | Simvastatin | 15 y | Sun-exposed areas | No/no | Recurrent episodes over 12 y | Phototest with drug led to a decrease in UV-B-MED and abnormal UV-A response. Normalization of UV-B MED and UV-A response at 2 mo and 9 mo, respectively, after withdrawal of the drug. | Negative |
| Rodríguez-Pazos et al.,20 2010 | M | 54 | Pravastatin | 4 y | Sun-exposed areas | No/no | Single episode | Phototest with drug led to a decrease in UV-B-MED, with normalization 3 mo after withdrawal of the drug. | Negative |
| Rodríguez-Pazos et al.,21 2011 | F | 43 | Paroxetine | 1 y | Sun-exposed areas | No/no | Single episode | Phototest with drug led to a decrease in UV-B-MED, with normalization 6 wk after withdrawal of the drug. | +UV-B |
| Gutiérrez-González et al.,22 2011 | F | 65 | Naproxen | 15 d | Sun-exposed areas | No/no | Single episode | Phototest with drug not performed. Negative photoprovocation test after 2 doses of the drug. | +UV-A |
Abbreviations: F, female; IV, intravenous; M, male; MED, minimal erythemal dose.
Cases of Photodistributed Erythema Multiforme Not Related To Drugs in the Literature.
| Study | Etiology | Sex | Age, y | Lesion Site | Systemic/Mucosal Symptoms | Clinical Course |
| Huff & Weston,14 1980 | HSV | M | 25 | Sun exposed areas (at site of previous burn) | No/no | Single episode |
| Wolf et al.,12 1994 | HSV | M | 12 | Sun-exposed areas | No/no | Recurrent episodes over 7 y |
| Wolf et al.,12 1994 | HSV | M | 9 | Sun-exposed areas | No/no | Recurrent episodes over 2 y |
| Pérez-Carmona et al.,13 2009 | HSV | M | 14 | Sun-exposed areas | No/no | Recurrent episodes over 5 y |
| Borges da Costa et al.,24 2008 | Secondary to PMLE | F | 35 | Two consecutive eruptions: the first in sun-exposed areas and the second in areas covered by bathing suit | No/no | Single episode |
| Fitzpatrick et al.,10 1983 | Idiopathic | M | 31 | Sun-exposed areas; occasional lesions in covered areas (palms and scrotum) | No/no | Recurrent episodes over 5 y |
| Calzavara Pintón et al.,25 2003 | Idiopathic | M | 39 | Sun-exposed areas; isolated lesions on palms and covered areas | No/yes | Recurrent episodes over 10 y |
| Tamagawa-Mineoka et al.,26 2008 | Idiopathic | F | 48 | Sun-exposed areas | No/no | Recurrent episodes over 1 y |
Abbreviations: F, female; HSV, herpes simplex virus; M, male; PMLE, polymorphous light eruption.
Drugs are the most common cause of PEM. Of the 18 cases of PEM reported to date, 10 were induced by topical or systemic drugs (Table 1). The drugs implicated were phenylbutazone,11 trichlocarban,15 afloqualone,16 bufexamac,17 paclitaxel,18,19 simvastin,20 pravastatin,20 paroxetin,21 and naproxene.22
Drug-induced PEM is generally characterized by a single outbreak of lesions. However, when the condition is misdiagnosed and administration of the drug is continued, the disease can become chronic, with recurrent eruptions over many years triggered by sun exposure.20 The time from the start of treatment to the appearance of lesions is variable, with reports in the literature ranging from 15 days11,17 to 4 years.20 There is usually no personal or family history of photodermatoses or recurrent HSV infection. While there may be a history of herpes labialis, there does not appear to be an association between this condition and PEM.21
The clinical characteristics of drug-induced PEM are identical to those of PEM with other precipitating factors. The lesions are located in sun-exposed areas and may be accompanied by systemic symptoms11 and mucosal involvement.15 Lesions due to topical drugs are usually observed at the application site. One patient described by Leroy et al.15 developed EM-like contact dermatitis in the genital area following the use of a soap containing triclocarban in this area; 48hours later, the lesions spread to sun-exposed areas. Kurumaji et al.17 described a similar case in which a patient developed eczematous contact dermatitis in the groin area after the application of topical bufexamac. He then developed EM-like lesions around the affected area and in areas that had been exposed to the sun.
Herpes Simplex VirusRecurrent HSV infection is the second most common cause of PEM. Of the 18 cases of PEM described in the literature, 4 were triggered by HSV.12–14 The main association is with herpes labialis, but cases have also been described in patients with genital herpes and herpes in other areas. HSV-associated PEM tends to affect young men who do not have a personal or family history of photodermatosis and who report not having taken drugs. It is typically characterized by recurrent outbreaks that occur once or twice a year, normally in the sunniest months of the year and coinciding with sun exposure.12,13 Herpes lesions precede the skin eruption by approximately 7 to 10 days. The eruption affects sun-exposed areas and is generally not accompanied by systemic or mucosal involvement. In 1 case described in the literature, the lesions were limited to areas previously affected by sunburn.14
Polymorphous Light EruptionThree cases of EM and PEM secondary to PMLE have been reported to date.23,24 The patients, a man and 2 women aged between 28 and 38 years, had had recurrent PMLE for years but had more recently developed a second type of eruption that was clinically compatible with EM and occurred 1 to 2 weeks after the episode of PMLE. In 2 of the patients, the EM-like lesions were recurrent and affected both sun-exposed and covered areas.23 The third patient experienced 2 episodes of EM following 1 of the episodes of PMLE.24 The first affected sun-exposed areas and the second occurred a week later, with lesions observed in the area that had been covered by the woman's bathing suit. The patient had not been in the sun during the intervening week.
Idiopathic PEMSeveral cases of PEM have been reported in patients without herpes reactivation, drug use, or any other known trigger. These idiopathic cases tend to recur over several years. The lesions are commonly located mainly in sun-exposed areas, although they may also affect covered parts of the body as well as the palms of the hands and mucous membranes.25
In our review of the literature, we found 3 cases of recurrent PEM with no identifiable cause.10,25,26 In 1 case, however, elevated serum titers of immunoglobulin (Ig) G and IgM for HSV were identified, suggesting the possible presence of subclinical HSV reactivation that might have been the source of the antigenic stimulus.10 In another case, the patient developed PEM when she started to work as an aromatherapist.26 Consequently, and despite the negative photopatch results, the involvement of a topical photoallergen cannot be ruled out. In the third case, Akarsu et al.27 described a patient who developed 2 outbreaks of target lesions histologically compatible with EM in sun-exposed areas; the authors classified the lesions as EM-like PMLE based on the presence of pruritus, the location of lesions in sun-exposed areas only, and the absence of mucosal involvement. However, the patient also had lesions on her face and the dorsum of her hands and PMLE does not usually affect areas subject to chronic sun exposure.28 We therefore believe that this case could possibly be classified as idiopathic PEM.
PathogenesisThe pathogenesis of EM is not fully understood, but it appears to be a hypersensitivity reaction of the skin to a variety of stimuli. In PEM, UV radiation might contribute to the development of lesions by inducing the release of inflammatory mediators, such as quinines, prostaglandins, and histamine, which would increase vascular permeability, thereby facilitating the passage of skin antigens into the bloodstream and favoring the formation of circulating antibodies in sun-exposed areas.23 The source of the antigenic stimulus is not always known.
Short sequences of viral DNA have been detected in keratinocytes in patients with HSV-associated EM, leading to the hypothesis that these sequences might act as antigens and induce the release of interferon γ.29,30
In drug-induced PEM, either a photoproduct or the actual drug activated by UV radiation might act as an antigen, triggering the immune response, or as a phototoxic agent, favoring the rupture of cells and the release of nuclear antigens, which would then pass into the bloodstream, facilitated by the increased vascular permeability induced by sun radiation.10,20 It has also been speculated that alterations of porphyrin metabolism induced by several drugs might be involved in the development of lesions.18,19 In PEM secondary to the topical application of drugs, the absorption of the drug through the skin or mucosa could cause systemic contact dermatitis, which might manifest as EM-like lesions. Finally, the location of lesions in sun-exposed areas could be due to the photo Koebner phenomenon, with light acting as a traumatic stimulus.17
In such cases, once the acute episode has been treated and the offending drug withdrawn, the patient does not generally experience further episodes. Recurrence following exposure to other antigens and sunlight has been reported in just 2 cases.16,21 In 1 of these, Rodríguez-Pazos et al.21 described a patient who developed 2 consecutive episodes of PEM related to 2 different antigens: paroxetine and HSV reactivation. In the other case, Shiohara et al.16 described a patient who experienced PEM in association with afloqualone and exposure to Rhus verniciflua, to which he had been previously sensitized. It has been postulated that following the initial episodes of PEM, the skin might retain traces of photoactive substances, but not in sufficient quantities to cause the development of lesions. The presence of additional, nonspecific, antigenic stimuli, such as HSV reactivation or contact dermatitis due to R verniciflua might then have an add-on effect and trigger the development of skin photosensitivity.16
It has also been suggested that PMLE might be an immune response to as yet unknown endogenous or photoinduced antigens, and that associated cases of EM or PEM could be triggered by the same antigenic stimulus. Another theory is that the sun exposure that triggers PMLE could cause subclinical HSV reactivation and the subsequent development of EM.23 However, in all the cases described to date, PEM and EM occurred after PMLE. Furthermore, although 1 of the patients had a history of recurrent herpes labialis, he had had no episodes in the preceding year that might explain the EM lesions.23
Subclinical reactivation of HSV has also been implicated in the etiology of several cases of idiopathic PEM,10 and HSV DNA has been detected by polymerase chain reaction in 40% of recurrent, apparently idiopathic EM.31 Some of the cases responded to prophylactic antiviral treatment, strongly suggesting that they were triggered by subclinical HSV infection.31
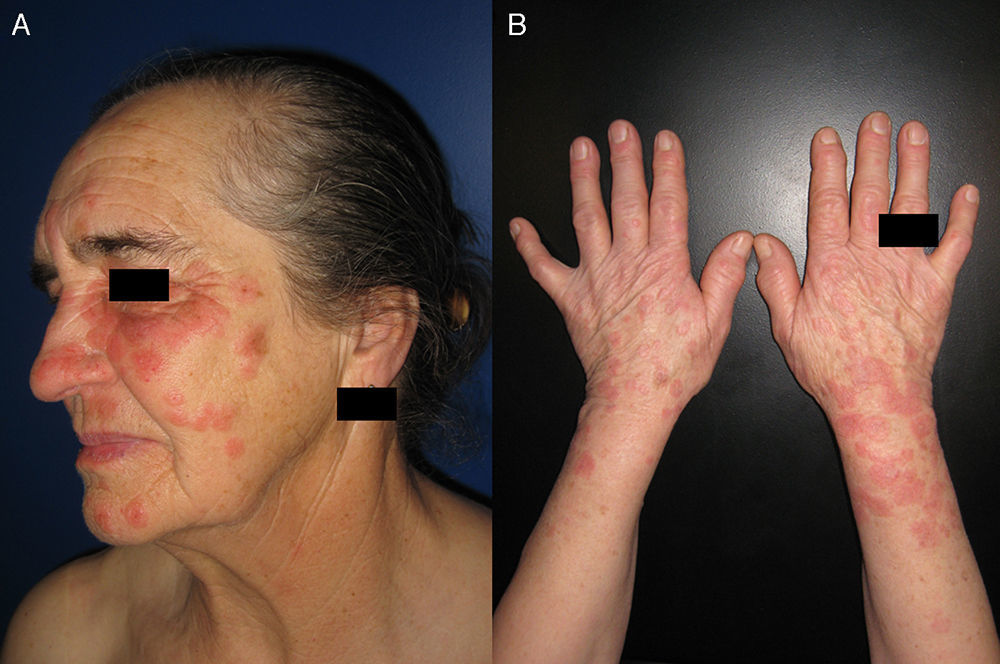
Clinical ManifestationsThe skin lesions that characterize PEM are identical to those seen in EM. They start out as erythematous macules and then develop into erythematous, edematous papules. They can grow and acquire a characteristic target-like appearance.1,32 These target lesions may be few in number, and may not even be apparent in the first few days after the onset of the rash.6 As these lesions are a key diagnostic clue, a thorough skin examination is essential.
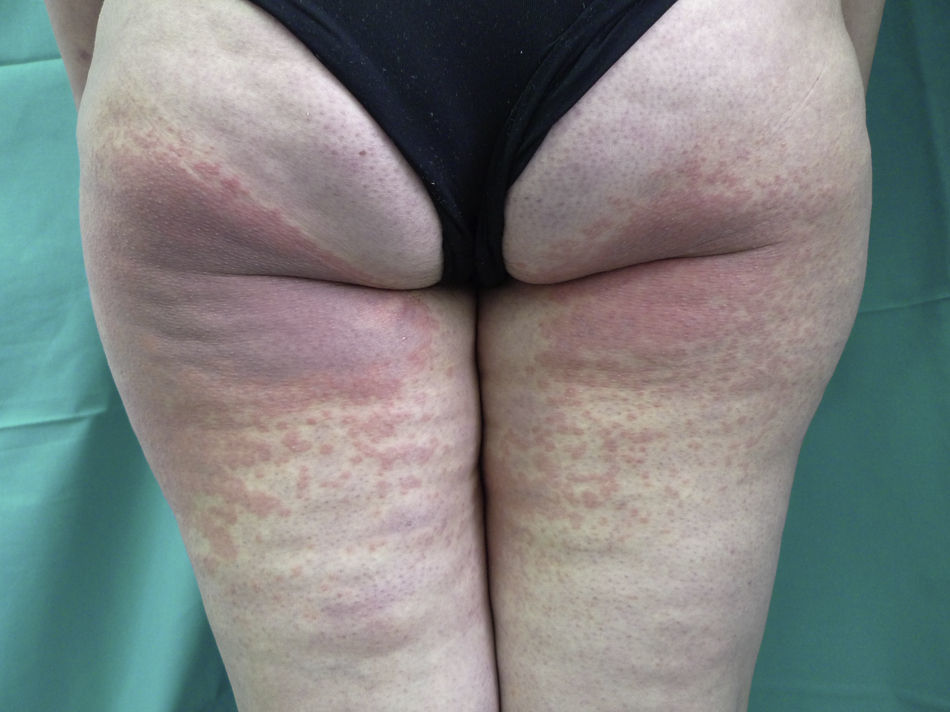
In PEM, the lesions are limited to sun-exposed areas. They typically affect the face, the neckline, the back of the arms and the forearms, but they can occur on any part of the body that has been exposed to the sun (Fig. 1). Certain physical findings can help to classify the condition as photodistributed: a) sparing of areas not exposed to the sun, such as under the chin or behind the ears, the nasolabial triangle, and the upper eyelids; b) a clear division between exposed areas (with lesions) and unexposed areas (without lesions) (Fig. 2); and c), typical absence of lesions on the palms of the hands and the mucous membranes. Nevertheless, in cases of idiopathic PEM, there have been reports of isolated lesions in covered areas (trunk and scrotum) and on the palms of the hands.10,25 Albeit rarely, some patients also develop fever, joint pain, and headache11 or lesions affecting the oral and/or genital mucosa.15,23,25 Onycholysis has been described in cases of paclitaxel-induced PEM.18,19 Patients with PEM can experience single or recurrent episodes that can occur at any time of the year, although they are more common in the sunnier months. Patients typically report previous sun exposure or the practice of outdoor activities.
When EM is suspected, the first step is to establish whether or not it is photodistributed and the second step is to identify the cause.
The diagnosis of EM is based on clinical history and physical examination and is greatly facilitated when the characteristic target lesions are detected. Laboratory tests do not generally reveal any distinctive alterations. Histology findings are characteristic but nonspecific and are particularly useful for excluding other diagnoses. Histologic features vary according to the type and site of the lesion biopsied and to the age of the lesion. A predominantly mononuclear inflammatory infiltrate is seen in early erythematous macules or papules.6,33 In lesions of longer duration and in the central area of target lesions, hydropic degeneration of the basal layer and necrosis of keratinocytes are observed. There may also be subepidermal blisters with keratinocytic necrosis in the adjacent area.6,33 The presence of a predominantly neutrophilic infiltrate or of leukocytoclastic vasculitis suggests a diagnosis other than EM.6
Once a diagnosis of EM has been established, the next step is to examine the lesions to determine whether or not they follow a photodistributed pattern.34 Clinical history, physical examination, and laboratory tests are useful for ruling out other photodermatoses. The following factors should all be considered: age at onset of the lesions, possible exposure to photosensitizing agents, exposure to light sources, time between exposure to the sun and development of the lesions, time since onset of the lesions, and a personal or family history of photodermatosis. The laboratory workup should include testing for antinuclear antibodies (ANAs) and anti-SSA (Ro) and anti-SSB (La) antibodies and measurement of plasma porphyrins.
The last step in the diagnostic workup is the identification of precipitating factors.
A diagnosis of drug-induced PEM must be confirmed by photobiologic testing, with at least 2 phototests performed at different times. Ideally, the first test should be conducted during the first visit (when the patient is still taking the suspect drug) and the second test after the drug has been withdrawn.35 Diagnosis is confirmed when response to UV radiation is altered in the first test and normal in the second one. It is easy to suspect PEM in patients who are taking just 1 recently introduced drug. In patients on several drugs that were prescribed simultaneously, however, it may be more difficult to identify the offending agent. In such cases, it is important to perform a sequential investigation until the drug responsible for the PEM is identified. The wavelength involved will vary according to the drug and it is therefore important to investigate response to both UV-B and UV-A radiation. The phototests should be performed on a part of the body that is usually covered by clothing, such as the buttocks or the lower back. If the patient has lesions at the time of testing, it is not necessary to wait for these to clear. The time it takes for phototest results to normalize after withdrawal of the drug responsible for PEM varies, and may be as long as a year.8 It is therefore important to repeat the tests regularly until the UV response is completely normal; at this point, it will be possible to establish a definitive diagnosis of systemic photosensitivity and at the same time exclude persistent light reactivity or chronic actinic dermatitis.8,36
Photopatch testing with a standard series of photoallergens and the suspect drug allows the dermatologist to exclude other diagnoses and determine whether or not the condition is immune mediated. The tests should be performed between 6 weeks and 6 months after resolution of the skin lesions, and at least a month after withdrawal of systemic corticosteroids or oral antihistamines. Phototest results must be normal before the photopatch tests are performed to prevent erythema from developing in the irradiated area. Photopatch testing can be performed using either the commercial drug or the pure substance. As a general rule, the commercial form of the drug can be applied directly or added to petrolatum or water at a concentration of 30%. Pure substances must be diluted at 10% in petrolatum, and if possible, also at 10% in water or alcohol.37,38 Each drug must be patch tested in triplicate. The 3 sets of patches are removed after 48hours. One of the sets is irradiated with 5J/cm2 of UV-A, while the other is irradiated with a sub-MED dose of UV-B (dose just below the dose that produces erythema, equivalent to 80% of the minimal erythemal dose, or MED). The third set serves as the control. It is important to perform the patch tests in controls, as a negative result will add credibility to a positive result in a patient.38
Photoprovocation can be useful for confirming diagnosis in both drug-induced and idiopathic cases. Based on data in the literature,10,17 some authors have postulated that it might only be possible to reproduce lesions during the initial eruption.12 However, there has been a report of lesions being provoked 4 weeks after the acute episode.25 Photoprovocation involves the performance of phototesting following the administration of the test drug at therapeutic doses over a period of 3 to 5 days. An alternative is phototesting performed 1, 3, and 5hours after the administration of a single dose of the suspect drug. The expected result would be a qualitative and/or quantitative pathologic response to the UV radiation. Informed consent must be obtained from the patient in all cases.
In our review of the literature, the diagnosis of drug-induced PEM was confirmed by photobiologic testing in 7 patients (Table 1). Three patients showed a decrease in UV-B-MED and/or a qualitatively pathologic response to UV-A while the patient was taking the drug and normalization of results after its discontinuation.20,21 In another case, the patient had already stopped treatment with the offending drug at the time of his visit.16 The phototest was therefore performed a posteriori, 3hours after the administration of a single dose of the drug. The result was a decrease in UV-B-MED. The time between discontinuation of the drug and normalization of the UV response varied among the patients. In 1 patient, the UV-B-MED returned to normal within 6 weeks,21 whereas in another, it took 12 weeks. In the third patient, UV-B-MED had normalized by week 8, but normal results were not seen on repeated UV-A-MED tests until month 9.20 Two of the 7 patients had a normal UV-B and UV-A response, but diagnosis was confirmed following the reproduction of EM lesions in the irradiated area.15,17 Photopatch tests with the suspect drug yielded positive results in 4 patients: 2 had a positive reaction in the area irradiated with a sub-MED dose of UV-B,15,21 1 had a positive reaction in the area irradiated with UV-A,22 and 1 had a positive reaction in the areas irradiated with UV-B and UV-A.17
HSV-induced PEM is diagnosed on the basis of a compatible clinical history and the exclusion of other possible causes of PEM. The skin eruption is usually preceded by HSV lesions and sun exposure. Elevated anti-HSV IgG titers are usually the only abnormal finding on blood tests. Photobiologic tests have been negative in all cases in which these tests were performed.12,13
Patients with PEM secondary to PMLE have a history consistent with PMLE that will probably have been present for several years. Laboratory and photobiologic test results are normal. A photobiologic study was reported for just 1 of the cases described in the literature; it was performed 2 months after the skin eruption and the patient showed a normal response to both UV-A and UV-B.24
Idiopathic PEM is diagnosed after all other known causes have been ruled out. Photoprovocation can reproduce lesions in some cases.10,26
TreatmentThe goal of treatment in EM is to reduce the duration of the skin lesions, alleviate symptoms, and prevent recurrence. To achieve this, it is necessary to eliminate the causative agent and treat the symptoms with antihistamines and topical and/or systemic corticosteroids. Sun protection measures are also important in the case of PEM.
In drug-induced PEM, avoidance of sun exposure and withdrawal of the offending drug tend to be sufficient to achieve resolution of lesions. Topical or systemic corticosteroids can also be used. There has also been a report of a successful outcome with dapsone and oral corticosteroids in 1 patient.16 A risk-benefit assessment should be performed before withdrawing the drug definitively, because, as was shown by Cohen et al.,19 treatment may be maintained if sun protection measures are taken. Patients do not generally experience recurrent episodes once treatment has been stopped. There have been just 2 reports of lesions returning following exposure to other antigens and sunlight.16,21
In HSV-induced PEM, symptomatic treatment with topical corticosteroids and antihistamines achieves resolution of lesions within days. Prophylactic treatment with acyclovir can prevent HSV reactivation and new episodes of PEM.12
As in drug-induced PEM, avoidance of sun exposure and the administration of antihistamines and oral and topical corticosteroids lead to the resolution of lesions. Short cycles of corticosteroids can be prescribed on detection of the first signs of PMLE, as these will interrupt the eruption within a matter of hours and prevent PEM from developing.23 Suppression of PMLE with prophylactic psoralen plus UV-A therapy also prevents the development of PEM.23
Idiopathic cases are logically more complicated to manage as the cause is not known. Patients tend to respond to oral corticosteroids, but lesions recur very soon after cessation of treatment. The prophylactic administration of hydroxychloroquine10,25 and long-term oral corticosteroids administered at low doses on alternate days in association with physical sun protection measures has been successful.25 Sulfapyridine and dapsone have not produced good results.10 Likewise, prophylactic narrow-band UV-B radiation25 and topical sunscreens used with or without oral antihistamines do not appear to be useful.
Differential DiagnosisThe differential diagnosis for PEM should include other photoaggravated dermatoses, certain idiopathic photodermatoses, and skin disorders that present with annular maculopapular lesions.
- 1.
EM-like PMLE. PMLE is a common idiopathic photodermatosis characterized by pruritic lesions in the form of erythematous papules, papulovesicles, vesicles, or plaques that develop in sun-covered areas hours or days after exposure to sunlight. Patients tend to report the development of lesions following exposure to the sun at the beginning of the summer. The episodes typically recur over successive years and the appearance of lesions is usually followed by what is known as the hardening phenomenon. Diagnosis is generally straightforward and is based on a compatible clinical history. Histology can help in doubtful cases. As already mentioned, PEM can be triggered by PMLE. Furthermore, it can sometimes be difficult to distinguish between the 2 entities. PMLE has many morphologic variants, some of which mimic EM. Furthermore, EM-like PLE and EM may be indistinguishable histologically. In such cases, investigation of viral DNA in skin biopsy specimens may be of use, as results are positive in between 32% and 72% of cases of EM and negative in PMLE.39 The absence of mucosal involvement in PMLE25 can also be a useful pointer. Finally, phototesting is negative in PMLE but not in drug-induced PEM.
- 2.
Juvenile spring eruption. This is a localized form of MPLE that tends to affect children aged between 5 and 12 years. It starts as erythematous papules that are located on the ears and can develop into vesicles or blisters. The detection of mucosal involvement and a history of HSV reactivation can help to establish a diagnosis of PEM rather than juvenile spring eruption.12
- 3.
Subacute cutaneous lupus erythematosus. This is a subtype of lupus erythematosus with distinctive clinical, histologic, and immunologic features. The most noteworthy of these are photosensitivity and the presence of anti-Ro (SSA) and anti-La (SSB) antibodies. Patients develop psoriasiform or annular lesions typically located in sun-exposed areas such as the neckline, the shoulders, the lateral aspect of the arms, and the dorsum of the hands, with sparing of the face.40 Small annular lesions can mimic the characteristic target lesions of EM.41 Subacute cutaneous lupus erythematosus can also be triggered by photosensitizing drugs, some of which have also been implicated in PEM.20,40
- 4.
Rowell syndrome. Patients with lupus erythematosus can develop lesions that are not only similar in appearance to those seen in EM but also follow an identical clinical course. Rowell syndrome was first described in patients with discoid lupus erythematosus, but it has also been seen in association with subacute cutaneous lupus erythematosus and systemic lupus erythematosus.41–43 Several authors do not consider Rowell syndrome to be a separate entity but rather a morphologic variant of subacute cutaneous lupus erythematosus with target lesions.41–43 The presence of ANAs, anti-LA (SSB) or anti-Ro (SSA) antibodies, rheumatoid factor, and perniotic lesions are typical findings in Rowell syndrome41 and can be useful in the differential diagnosis.
Other diseases with target lesions that should be included in the differential diagnosis are acute hemorrhagic edema of infancy, EM-like contact dermatitis, paraneoplastic pemphigus, IgA pemphigus, pruritic urticarial papules and plaques of pregnancy, syphilis, fixed drug eruption,44 ecthyma gangrenosum, erythema chronicum migrans, and granuloma annulare.45–49 In their very early stages and depending on their distribution, urticarial lesions,32 urticarial vasculitis,50 and rosacea may also resemble PEM lesions.
ConclusionsPEM is an uncommon, probably underdiagnosed, skin condition that can affect both sexes and patients of all ages. It has been associated with drugs, HSV reactivation, and PMLE. Diagnosis is based on clinical history, physical findings, histopathology, and photobiologic tests. The condition runs a self-limiting, benign course but can recur over successive several years if the cause is not eliminated. Treatment is symptomatic, with avoidance of triggers and the use of sun protection measures.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rodríguez-Pazos L, et al. Eritema multiforme fotodistribuido. Actas Dermosifiliogr. 2013;104:645–53.