Persistent labial edema is a nonspecific clinical manifestation that can occur in many different diseases, including Melkersson-Rosenthal syndrome or its monosymptomatic form, granulomatous cheilitis or Miescher syndrome.
We describe the case of a 76-year-old woman who was referred to our department for acquired edema in the lower left lip. Since its onset about 2 years previously, the lesion had been completely stable and asymptomatic. The patient's personal history included dyslipidemia, treated with atorvastatin, and left hemifacial spasm 8 years earlier. She had also received regular 6-month infiltrations of botulinum toxin in the orbicular muscle of the left eyelid for 4 years.
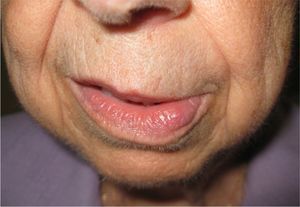
The examination revealed well-organized, nonpitting, nonpulsatile edema in the lower left lip, of soft, rubbery consistency; the mucous membranes and other oral structures were completely normal. No discoloration or local signs of superinfection were observed (Fig. 1). Additionally, the patient was unable to fully close her left eye and presented muscle twitching on the left hemiface. She reported no surgical operations, local radiotherapy, infiltrations of botulinum toxin or filler material in the area, or prosthetic dental work in contact with the affected area.
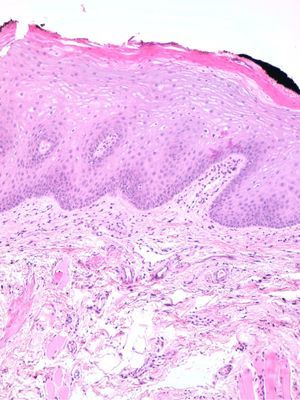
Because the lip swelling was accompanied by motor disturbances, the lesion was biopsied to perform a differential diagnosis with granulomatous cheilitis. Histology of the specimen showed lip edema with some ectasia of the lymphatic vessels in the specimen, but no granulomatous lesions or other inflammatory lesions (Fig. 2).
Hemifacial spasm is an involuntary abnormal movement of the face and is relatively common. The clinical entity is characterized by repeated tonic–clonic twitches of the muscles innervated by the facial nerve (cranial nerve VII). Hemifacial spasm is seen more often in women and in adulthood and usually appears as the sequela of idiopathic peripheral facial paralysis. However, cases secondary to large vascular abnormalities and tumors (e.g., neurinoma or meningioma) have also been reported. The condition typically presents insidiously and affects the orbicular muscles, in the form of eyelid twitching, and extends ipsilaterally to other muscles.1 Spasms are initially paroxysmal, but later increase in frequency and severity and then become sustained contractions.2 These tonic contractions would, in our opinion, hinder venous and lymph return from the affected areas, thus causing an increase in the diameter of the abundant lip vasculature.
The differential diagnosis should include conditions such as hereditary and acquired angioedema (in these cases, the lesions disappear within 24 to 48hours), various orofacial granulomatoses such as lymphomatoid granulomatosis, Crohn disease, and Melkerson-Rosenthal syndrome and its monosymptomatic form (granulomatous cheilitis or Miescher syndrome).3–5 The contractions can be associated with other accompanying manifestations (e.g., pulmonary or intestinal involvement, facial paralysis, or tongue fissures, respectively), and the biopsy tends to provide the diagnosis.
Likewise, it is necessary to rule out congenital or acquired lip malformations (lymphangioma, hemangioma, and neurofibromatosis), Ascher syndrome (possibly associated with blepharochalasis and thyroid goiter), and cheilitis glandularis, where the increased size of lips is due to secondary inflammation of heterotopic salivary glands in the lips.6 All these conditions have a well-established histologic diagnosis.
A final hypothesis to consider is the effect of regular botulinum toxin infiltration. Although cases of local edema secondary to botulinum toxin infiltrations have been described,7 in our patient this treatment was never administered in the circumoral region, and edema severity was unchanged long after injections, when the drug would have been expected to have a lower therapeutic effect.
In conclusion, although hemifacial spasm is not rare, there are no published reports in the literature that associate it with persistent labial edema. This phenomenon could be explained by the fact that the condition is asymptomatic and mundane. Therefore, the patient is unlikely to be referred to a specialist unless the clinical picture is noteworthy, hence the condition is underdiagnosed. Because both manifestations can appear together, they should be taken into account in the differential diagnosis of persistent lip swelling.
Please cite this article as: Bella-Navarro R, et al. Edema labial persistente secundario a espasmo hemifacial. Actas Dermosifiliogr. 2012;103:157–158.