In recent years, the widespread use of taxane-based chemotherapy regimens for the management of malignant tumors of various origins has evidenced the high frequency of cutaneous toxicity induced by this pharmacological group.1 In 2003, among its possible manifestations, Childress and Lokich2 defined periarticular thenar erythema and onycholysis (PATEO) syndrome as a rare subtype of hand-foot syndrome associated with nail changes in patients treated with paclitaxel and docetaxel. In contrast to typical palmar-plantar erythrodysesthesia, or classic hand-foot syndrome, skin involvement in this syndrome is characterized by an absence of involvement of the palms and soles and by the presence of alterations predominantly affecting the dorsum of the hands (particularly around the base of the thumb and fifth finger), the area of the Achilles tendon, and the perimaleolar skin.3
We present 3 patients on chemotherapy with taxanes who developed clinical manifestations similar to those described in this syndrome.
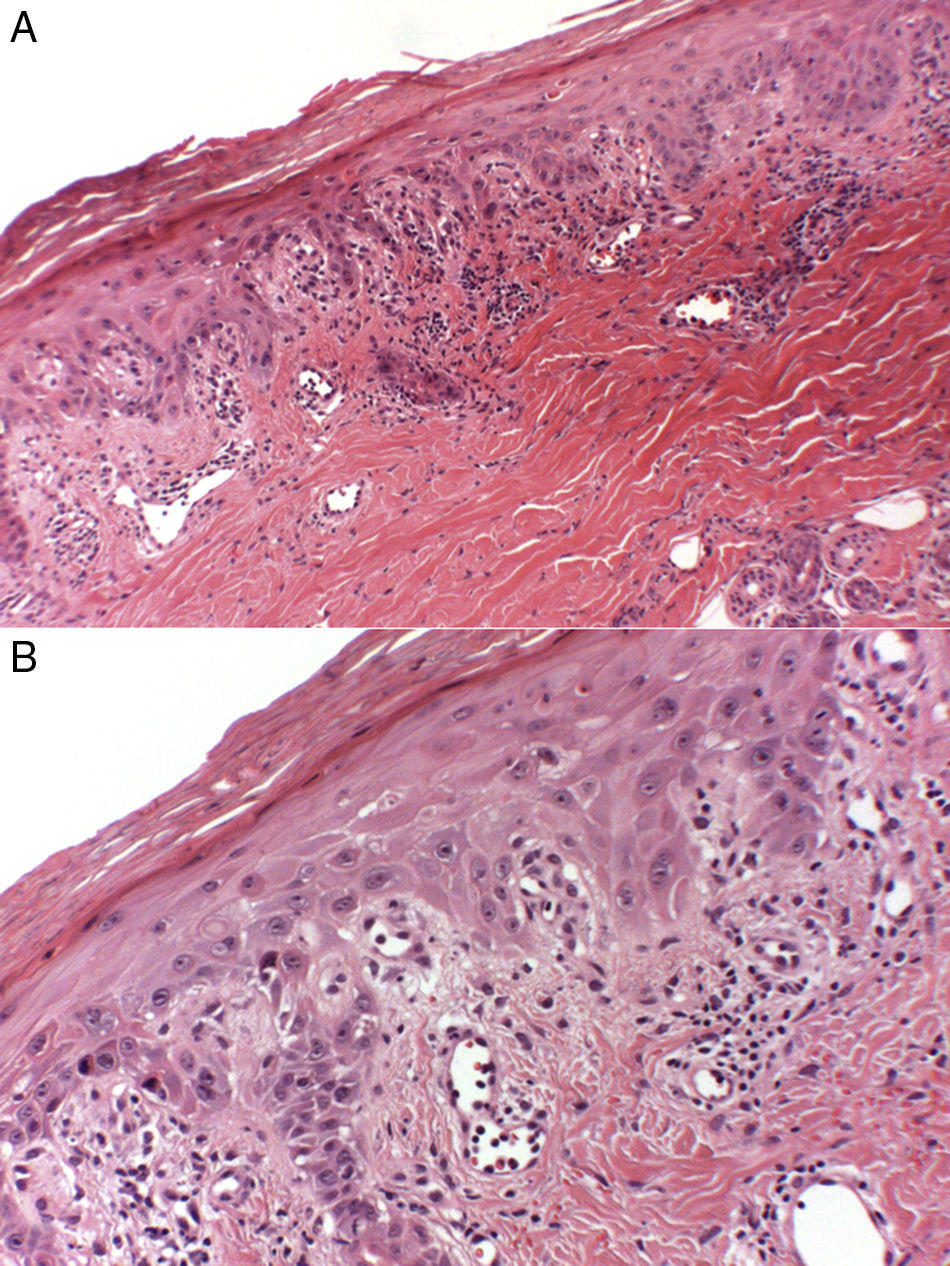
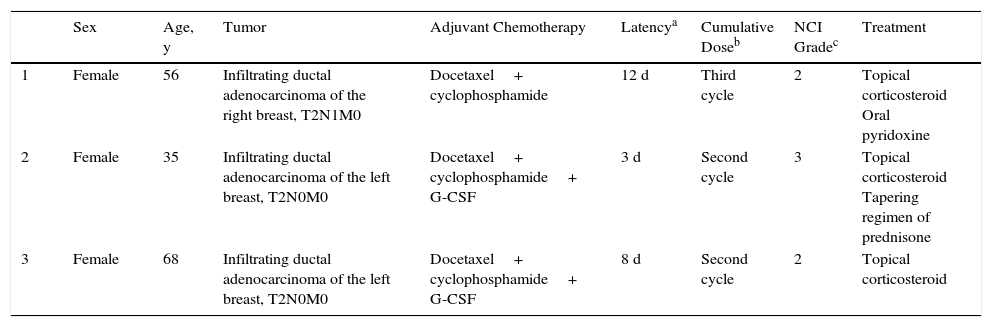
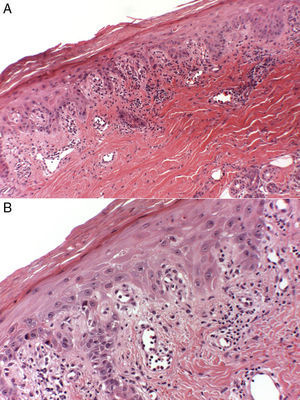
The 3 patients were women aged 35, 56, and 68 years, with infiltrating ductal adenocarcinoma of the breast on adjuvant treatment with docetaxel and cyclophosphamide (Table 1). They sought dermatologic evaluation for the appearance of painful erythematous-violaceous plaques with fine superficial desquamation on the dorsum of both hands (Fig. 1A). The lesions interfered with their activities of daily living. The lesions had arisen 3 to 12 days after the administration of chemotherapy, and showed a clearly progressive deterioration with each cycle, despite the use of topical corticosteroids. Associated nail involvement in the 3 cases varied from fine parallel Beau lines and subungual splinter hemorrhages to frank distal onycholysis of the nail plate (Fig. 1 B). Physical examination revealed no lesions on the rest of the skin, and the patients presented an otherwise good general state of health. Histology of a 4-mm punch biopsy from the dorsum of the hand of patient number 2 revealed a hyperkeratotic epidermis with parakeratosis, necrotic keratinocytes, focal vacuolar degeneration of the basal layer, and a band-like perivascular lymphocytic inflammatory infiltrate with occasional eosinophils (Fig. 2,A andB). These findings were consistent with a clinical suspicion of taxane-induced toxicity. Dose adjustment of the chemotherapy, together with the application of topical corticosteroid therapy under occlusion controlled the lesions and significantly improved symptoms in all 3 patients. Only 1 patient required a single course of a tapered regimen of oral corticosteroids for a severe deterioration of the lesions on the dorsum of the hands that interfered with her activities of daily living.
Epidemiologic, Clinical, and Therapeutic Details of 3 Cases of Periarticular Thenar Erythema and Onycholysis Syndrome.
| Sex | Age, y | Tumor | Adjuvant Chemotherapy | Latencya | Cumulative Doseb | NCI Gradec | Treatment | |
|---|---|---|---|---|---|---|---|---|
| 1 | Female | 56 | Infiltrating ductal adenocarcinoma of the right breast, T2N1M0 | Docetaxel+ cyclophosphamide | 12 d | Third cycle | 2 | Topical corticosteroid Oral pyridoxine |
| 2 | Female | 35 | Infiltrating ductal adenocarcinoma of the left breast, T2N0M0 | Docetaxel+ cyclophosphamide+ G-CSF | 3 d | Second cycle | 3 | Topical corticosteroid Tapering regimen of prednisone |
| 3 | Female | 68 | Infiltrating ductal adenocarcinoma of the left breast, T2N0M0 | Docetaxel+ cyclophosphamide+ G-CSF | 8 d | Second cycle | 2 | Topical corticosteroid |
Abbreviations: G-CSF, granulocyte colony stimulating factor; NCI, National Cancer Institute.
Periarticular thenar erythema and onycholysis syndrome: Docetaxel-induced skin and nail changes. A, Patient1. Erythematous-violaceous plaques on the dorsum of the hands and over the proximal phalanx. B, Nail changes in patient 3: parallel Beau lines and onycholysis of the distal third of the nail plate.
Histology of the lesion on the dorsum of the hand of patient2. A, Hyperkeratotic epidermis with parakeratosis, foci of vacuolar degeneration of the basal layer, and a band-like perivascular infiltrate with occasional eosinophils. Hematoxylin and eosin, original magnification ×10. B, At higher power, evidence of necrotic keratinocytes in the epidermis. Hematoxylin and eosin, original magnification×40.
PATEO syndrome is a manifestation of taxane-induced cutaneous toxicity predominantly affecting acral areas and with associated nail alterations. The frequency of this complication has been reported as 10% and 5%, respectively, in patients treated with paclitaxel and docetaxel, and its intensity appears to increase with the cumulative dose and with weekly regimens.2,3 Skin involvement is characterized by the presence of painful erythematous-violaceous plaques on the dorsum of the hands, on the feet, and in the area of the Achilles tendon; these lesions can subsequently develop vesicles and flaking. Severity is very variable, from asymptomatic forms to ones that have a marked impact on the basic activities of daily living. Some classifications, such as those of the World Health Organization and the National Cancer Institute, have established criteria of severity to evaluate acral skin involvement.4,7
Nail changes in these patients are due to the cytotoxic effect of taxanes and their presence is characteristic of this condition, in contrast to other hand-foot syndromes secondary to anthracyclines or multikinase inhibitors.5 The cytotoxicity of these agents is due to their inhibition of microtubule function in cell division, and is most intense in those epithelia with high rates of cell proliferation, such as the nail matrix. The most common changes described after the administration of these drugs are Beau lines, onychomadesis, onycholysis, subungual splinter hemorrhages, subungual hematomas, leukonychia, paronychia, and nail hyperpigmentation.4,5 Although the clinical manifestations are not usually severe, some manifestations, such as subungual hematomas, abscesses, and distal onycholysis can cause significant morbidity in oncologic patients and must be taken into consideration.6
Histology of the skin lesions reveals changes similar to those observed in typical palmar-plantar erythrodysesthesia induced by other chemotherapeutic agents. It is characterized by the presence of a hyperkeratotic and acanthotic epidermis, with necrotic keratinocytes, focal vacuolar degeneration of the basal layer, blood-vessel dilatation, and a lichenoid inflammatory infiltrate with few lymphocytes, neutrophils, or eosinophils.3,7
In clinical practice, the impact of PATEO syndrome on the quality of life of oncology patients is a frequent cause of dose reduction of the chemotherapy regimen, as occurred in our patient number 2. In the most severe and disabling cases, discontinuation of treatment may even be indicated.8 Preventive measures are an essential strategy to reduce the morbidity associated with these treatments in debilitated patients. Local hypothermia using socks or gloves during infusions of the drug can be effective, though this cannot be extended to other chemotherapy regimens with oral administration.9,10
Given the high frequency of dermatologic consultations related to the side effects of chemotherapy in oncology patients, we consider it important to be aware of this atypical form of acral erythema and of its management as, in disabling cases, it can require dose reduction or a temporary interruption of the chemotherapy treatment. It is notable that all 3 of our patients were on combined treatment with cyclophosphamide and docetaxel for adenocarcinoma of the breast, and the possibility that the combination may have increased the cutaneous morbidity compared with the administration of docetaxel in monotherapy cannot therefore be excluded.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rodríguez-Lomba E, Molina-López I, Suárez-Fernández R, Baniandrés-Rodríguez O. Síndrome de eritema tenar periarticular y onicolisis: una manifestación de toxicidad cutánea por taxanos. Actas Dermosifiliogr. 2017;108:595–597.