Paraneoplastic acral vascular syndrome involves an association between malignancy and Raynaud phenomenon, gangrene, or acrocyanosis of the fingers. Raynaud phenomenon is a transient digital ischemia resulting from vasoconstriction on exposure to cold temperatures or stressful situations. In its secondary form, it is usually associated with rheumatic disease and rarely occurs as a paraneoplastic phenomenon.1–3
We present the case of a 49-year-old man with no personal history of interest who smoked 80 cigarettes and drank 60g of alcohol per day. He visited the emergency department with sudden-onset cyanosis on the first 3 fingers of the left hand that was preceded by cutaneous pallor with paresthesia and intense pain (Figure 1). He had no other symptoms that were indicative of systemic disease, and the remainder of the physical examination was unremarkable. His heartbeat was regular, with no murmurs, and the distal pulses were palpable and symmetrical in all 4 extremities. The coagulation study was normal, except for D-dimer, which was >5000ng/mL. Prothrombin time and activated partial prothrombin time were normal. Arterial Doppler ultrasound showed that the blood supply reached the spaces between the fingers of the affected hand. Arteriography revealed a distal occlusion of the radial artery of the second finger, with proximal occlusion of the palmar digital arteries of the second and third fingers. The chest x-ray revealed a 4-cm mass on the right lower lobe (Figure 2). Fine needle aspiration findings were consistent with giant cell carcinoma of the lung. The extension study revealed no lymph node involvement. Initial treatment was with low-molecular-weight heparin, which led to a slight improvement in the skin symptoms. Therefore, pentoxifylline, acetylsalicylic acid, and intravenous alprostadil were added sequentially, although the results were mediocre. A clear clinical improvement was observed once the tumor was removed, and the Raynaud phenomenon resolved.
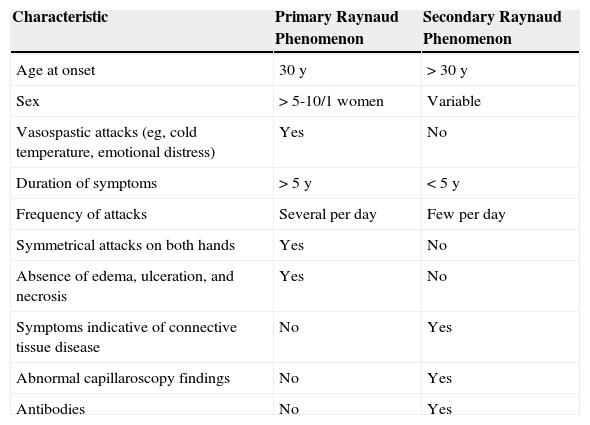
Only 33 cases of paraneoplastic acral vascular syndrome have been reported to date. Adenocarcinomas of the lung, ovary, and stomach account for 60% of all neoplasms, which are almost always in advanced stages with metastasis. The remaining neoplasms comprise sarcoma, hematologic neoplasm, and tumors of unknown origin. Skin lesions precede cancer in 50% of cases, as in the patient we report. Little is known about the pathogenic mechanism underlying this syndrome, although vasoconstrictive substances produced by tumor cells have been implicated. Embolism caused by small tumor thrombi may also play a role. In some hematologic neoplasms (eg, multiple myeloma), ischemia is caused by increased blood viscosity secondary to associated cryoglobulinemia. Histopathology shows fibrinoid necrosis in the veins and arteries.4–6 Our study of the present case shows that a thorough evaluation of the patient should be performed before Raynaud phenomenon can be classed as primary. The criteria for a diagnosis of secondary Raynaud phenomenon are shown in Table 1. Unilateral presentation should alert the physician to involvement of the subclavian artery. Doppler ultrasound and arteriography can confirm the diagnosis, as in the present case. Furthermore, since it is found in 80% of cases, gangrene should raise the suspicion of a paraneoplastic origin. Nailfold capillaroscopy is also very useful: dilated and tortuous capillaries point to early forms of systemic sclerosis.7
Diagnostic Criteria of Raynaud Phenomenon (Modified According to Le Roy Medgester, 1992).
| Characteristic | Primary Raynaud Phenomenon | Secondary Raynaud Phenomenon |
|---|---|---|
| Age at onset | 30 y | > 30 y |
| Sex | > 5-10/1 women | Variable |
| Vasospastic attacks (eg, cold temperature, emotional distress) | Yes | No |
| Duration of symptoms | > 5 y | < 5 y |
| Frequency of attacks | Several per day | Few per day |
| Symmetrical attacks on both hands | Yes | No |
| Absence of edema, ulceration, and necrosis | Yes | No |
| Symptoms indicative of connective tissue disease | No | Yes |
| Abnormal capillaroscopy findings | No | Yes |
| Antibodies | No | Yes |
Treatment of primary Raynaud phenomenon or Raynaud phenomenon associated with rheumatic disease is based on vasodilators, mainly calcium antagonists, the most commonly used of which is nifedipine. New drugs, such as phosphodiesterase inhibitors (sildenafil, tadalafil, and cilostazol), have proven effective in severe Raynaud phenomenon. Anticoagulant therapy with heparin could be indicated in cases of persistent critical limb ischemia or suspected occlusive arterial disease. Local digital sympathectomy can be considered when digital ischemia is severe and does not respond to medical treatment. This approach leads to a rapid increase in blood flow in the fingers. Paraneoplastic Raynaud phenomenon is usually refractory to vasodilators and sympathectomy, and symptoms are improved by treating the underlying malignancy. Complete cure has been reported in 48% of patients, with control of the tumor, as in the present case.8–10 Appropriate diagnosis of paraneoplastic Raynaud phenomenon enables the tumor to be detected early and suitable treatment to be initiated quickly. The condition should be suspected when it appears after age 30 in a patient with no history of autoimmune or vascular disease.
Please cite this article as: Rodríguez Martín AM, Guirao Arrabal E, Jiménez Puya R, Vélez García-Nieto A. Síndrome vascular acral paraneoplásico. Actas Dermosifiliogr. 2015;106:601–602.