Osteonevus of Nanta is a rare condition characterized by osseus metaplasia in an intradermal nevus.1 The lesion was first described by Heidesfield in 1908, and in 1911, it was reported in a publication by French dermatologist André Nanta.2
Bone formation in the skin is uncommon and can be primary (when there is no evidence of a pre-existing lesion) or secondary to an inflammatory and/or neoplastic process.3 Secondary bone formation has been reported in a range of lesions, including pilomatrixoma, basal cell carcinoma, acne, pyogenic granuloma, and dermatofibroma. Ossification of an intradermal nevus, however, is very rare.1,4
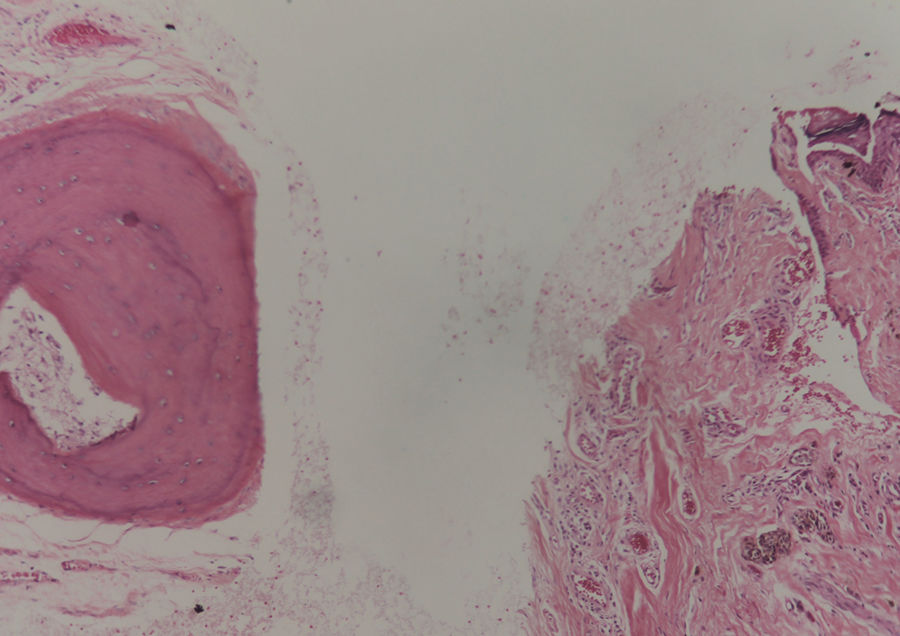
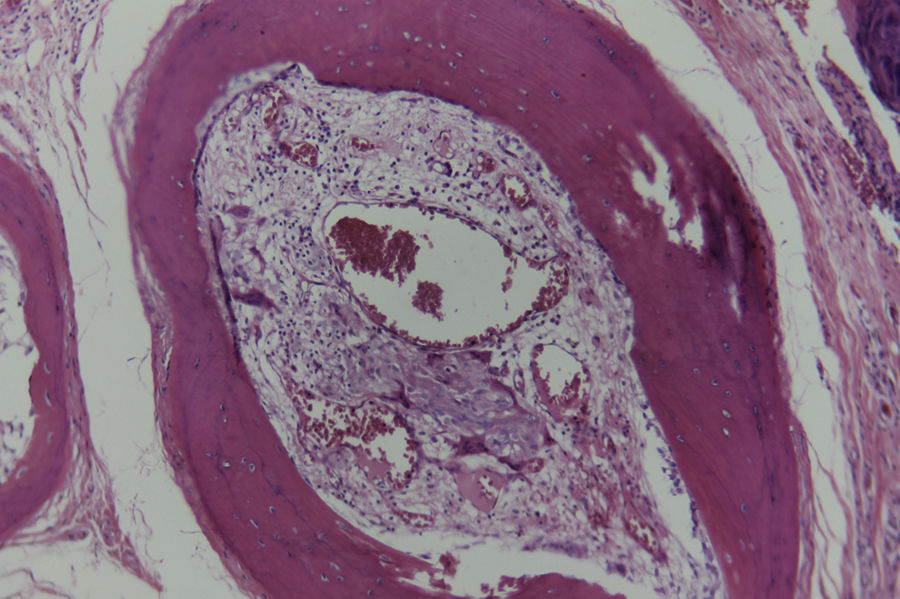
A 38-year-old man with no remarkable history presented with a hyperpigmented lesion on his left cheek that had grown and become progressively harder with time. Physical examination showed a hard, black nodule that measured 1.5cm in diameter and was not painful on palpation (Fig. 1). The lesion was fully excised and a sample sent for evaluation. Histologic examination showed nests of nevus cells with appropriate maturation in the superficial dermis and, underneath, in the deep dermis, bone marrow trabeculae containing osteocytes (Fig. 2). Signs of intramedullary hematopoiesis and mature adipocytes were observed in the center (Fig. 3). The lesion was diagnosed as osteonevus of Nanta and the patient was scheduled for regular follow-up.
Primary cutaneous bone formation has been described in Albright hereditary osteodystrophy, progressive osseous heteroplasia, myositis ossificans progressiva, and osteoma cutis.4 Secondary cases, in turn, have associated with scars, pyogenic granuloma, epidermal cyst, fibroxanthoma, and lipoma, and there have also been reports at the site of trauma or injection.3,4 Rarer associations include burns, dermabrasion, stasis dermatitis, and cutaneous metastases from breast, bladder, or bronchial cancer.5 Benign tumors, and melanocytic nevi in particular, are the most common causes of secondary osteoma formation.3
Clinically, osteonevus of Nanta resembles an intradermal nevus, is more common in women,6 and tends to be located in the upper part of the body, in particular the face, suggesting a potential pathogenic role for repeated hair follicle trauma and chronic inflammation.3,7 Lesions with necrosis, bleeding, and tissue regeneration could affect physical and chemical factors, such as calcium and phosphorous ion concentrations, pH, oxygen levels, and enzyme activity.3 These factors could induce a granulomatous reaction, triggering the transformation of mesenchymal cells into osteoblasts and resulting in bone formation.3 The most likely mechanism, however, is fibroblast differentiation (stimulated or not) in bone tissue.6
The higher incidence observed in women has also raised the possibility of a pathogenic role for estrogen.6 Estrogen would bind to osteoblast surface receptors, triggering the release of cytokines and inhibiting bone resorption and osteoclastic activity.1 Certain cytokines, together with cell adhesion proteins and β-transforming factor in particular, would allow mesenchymal stem cells to differentiate into osteoblasts, initiating ossification.8
Histologic examination of osteonevus of Nanta shows signs of ossification under nevus cells.3 Characteristic findings include laminated or globular bone with a central cavity containing adipose tissue, osteoblasts, osteoclasts, blood vessels, and occasionally bone marrow elements; hair follicles are almost invariably observed in the lesions.7,9
There is no established management for osteonevus of Nanta, and histologically, the lesion is benign. Culver and Burgdorf,10 however, did report a case of malignant melanoma arising in an osteonevus of Nanta, leading some authors to advise monitoring of patients.
We have presented the case of a patient with a nevus and histologic features consistent with osteonevus of Nanta. The lesion was fully excised and the patient is being monitored. No signs of recurrence have been observed.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr. Gabriela Santacruz, Head of the Dermatology Department at Hospital San Francisco de Quito, and the patient for giving us his written consent to publish the photographs that appear in this article.
Please cite this article as: Alvarado AV, Dávila-Rodríguez JJ, Vélez B, Montenegro-Zumárraga M. Osteonevus de Nanta, un fenómeno cutáneo poco habitual. 2019;110:329–331.