The patient was a Moroccan man aged 27 years. He had no known drug allergies and no past history of interest. He was being investigated in internal medicine for a widespread lymphadenopathy that had developed several months earlier. Two months before consultation in dermatology, he developed slightly tender lesions on the forehead that had progressively increased in size.
Physical ExaminationThree nodular lesions measuring between 10 and 20mm in diameter were observed in the left frontal region. There were no changes in the overlying skin (Fig. 1).
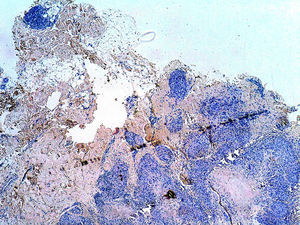
HistopathologyBiopsy of a lesion revealed epithelioid granulomas in the hypodermis with a low-grade lymphocytic response and foreign body material, with no central necrosis. Birefringence for foreign bodies was negative (Fig. 2).
Additional TestsGeneral biochemistry, C-reactive protein, angiotensin converting enzyme, complete blood count, and erythrocyte sedimentation rate were within normal limits. Serology for human immunodeficiency virus, hepatitis A, B, and C viruses, Epstein-Barr virus, cytomegalovirus, toxoplasma, and parvovirus B19 was negative. The Mantoux test was negative. Sputum and urine cultures for mycobacteria were negative. Culture and the polymerase chain reaction for mycobacteria in the skin biopsy were negative. Thoracic and abdominal computed tomography revealed pathological axillary, mediastinal, paratracheal, para-aortic, hilar, subcarinal, cardiophrenic, retroperitoneal, and mesenteric lymph nodes. Fine needle aspiration biopsy of an axillary lymph node showed no signs of malignancy.
What is Your Diagnosis?
DiagnosisSubcutaneous sarcoidosis associated with systemic sarcoidosis.
Clinical Course and TreatmentTreatment was started with prednisone, 1mg/kg/d, by mouth in a tapering regimen, and the patient was administered 3 monthly intralesional injections with triamcinolone acetonide diluted 1-in-3 in normal saline. This produced a slight improvement, with no increase in the number of lesions at subsequent follow-up visits.
CommentSarcoidosis is a chronic granulomatous disease of unknown origin, characterized by the formation of noncaseating granulomas in different organs and tissues. Around 25% of patients develop skin lesions, which can be specific or nonspecific depending on the presence or absence of granulomas on histology. The specific lesions include macules, papules, plaques, lupus pernio, subcutaneous sarcoidosis, and cicatricial sarcoidosis, while the nonspecific lesions are erythema nodosum, plaques of alopecia, calcifications, and pruritic lesions, among others.1
Subcutaneous sarcoidosis, also known as Darier-Roussy sarcoid, is the least common specific form (12%) and only affects the hypodermis. It is most common in white women aged between 40 and 60 years. Clinically it presents as multiple firm, slightly painful, mobile, round, skin-colored nodules that typically arise on the limbs bilaterally but asymmetrically. They have also been reported on the trunk, face, buttocks, and head and neck.2
Ahmed and Harshad3 reported a strong association between subcutaneous sarcoidosis and moderate systemic involvement by sarcoidosis. Lesions of subcutaneous sarcoidosis are observed in up to 2% of cases of systemic sarcoidosis. Although the lesions may be the first sign of the systemic sarcoidosis, it is more common for them to develop during the course of the disease; they are rarely an isolated finding.4
The diagnosis is based on the clinical manifestations and histology, which reveals a predominantly lobular panniculitis with noncaseating epithelioid granulomas, with no peripheral lymphocytic corona, but with a large number of multinucleated giant cells. Schaumann (conchoidal) bodies and asteroid bodies may be seen; although these lesions are characteristic, they are not pathognomic of sarcoidosis.
The differential diagnosis should include erythema nodosum, tuberculosis, and other granulomatous diseases, such as fungal or atypical mycobacterial infections, birefringent foreign bodies, and autoimmune diseases such as rheumatoid arthritis or lupus erythematosus.5
Some authors have reported spontaneous resolution of the nodules. However, when associated systemic disease is present, the oral corticosteroids, hydroxychloroquine, tetracyclines, methotrexate, dapsone, clofazimine, and nonsteroidal anti-inflammatory drugs have been found to be effective.6
Our case is interesting because the appearance and easy accessibility of lesions in the frontal region enabled us to make a diagnosis of systemic sarcoidosis associated with subcutaneous sarcoidosis (Darier-Roussy sarcoid). It should be noted that sarcoid nodules are very rare on the forehead.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr. Antonio Aguilar Martínez for his help in making the diagnosis.
Please cite this article as: Lobato-Berezo A, Burgos-Lázaro F, Gallego-Valdés MÁ. Nódulos frontales asociados a adenopatías generalizadas. Actas Dermosifiliogr. 2015;106:579–580.