The lateral walls and alae of the nose are cosmetic and functional units of the external nose and are areas where malignant skin tumors, particularly basal cell carcinoma, are common. During reconstruction of this region, we must take into account not only the function of the nares, avoiding retraction, which would lead to collapse during inhalation, but also their symmetry, aiming to achieve the best possible cosmetic result.1
The problem is greater if there is a full thickness surgical defect affecting all the tissue planes (mucosa, cartilage, muscle, and skin), as this will considerably reduce the options for reconstruction.
Local intranasal flaps with re-epithelization of the secondary defect are very useful for repair of the mucosal plane, but the technique is laborious. Mucoperichondrial flaps from the nasal septum, wall, or conchae have the added advantage of providing cartilaginous support.2,3 Cartilage grafts from the septum, helix, or costal cartilage, combined with local flaps are an excellent option.4 Finally, the use of inert alloplastic materials, such as titanium or polyethylene mesh, can be a good alternative, particularly in large defects, but none of these materials is free of risks such as necrosis, infection, or extrusion.5
In the case presented, after considering all possible options, and in an attempt to minimize their aforementioned drawbacks, we decided to use a myochondromucosal rotation flap from the adjacent ala combined with an ipsilateral melolabial flap. The procedure can be seen in the video.
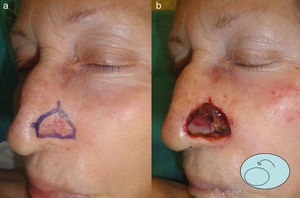
TechniqueThe patient was a 79-year-old woman in whom a recurrent basal cell carcinoma was fully excised after 2 stages of Mohs micrographic surgery (Fig. 1 A). The lesion infiltrated the lateral wall of the nose and a large part of the ala, with full-thickness involvement of the central part of the ala (Fig. 1 B). The size of the overall defect created was 2×2cm; the central full-thickness defect measured 1×1.2cm. Closure was performed using a myochondromucosal rotation flap from the whole of the adjacent ala combined with an ipsilateral melolabial flap.
When creating the myochondromucosal flap, we had to ensure that there was an adequate pedicle to avoid necrosis. After rotation onto the area of the tip of the nose, the borders were fixed with an absorbable 4/0 polyglycolic acid suture.
When creating the skin flap, we had to consider not only the length to width ratio, in order to avoid necrosis, but also its thickness, in order to achieve an acceptable cosmetic result and avoid the very undesirable trap-door effect. After resection and adjustment, the tip of the skin flap was sutured with 4/0 silk.
The functional and cosmetic result 8 weeks after the operation was excellent (Fig. 2).
Indications- -
Reconstruction of partial, full-thickness defects of 1 to 1.5cm in diameter affecting the alar and perialar regions of the nose.
- -
Very small full-thickness defects in which cartilage repair is not necessary or when the defect can be closed by direct suture.
- -
Very large defects in which there is insufficient adjacent tissue to cover the defect.
- -
Infection.
- -
Postoperative chondritis.
- -
Trap-door effect.
- -
Retraction of the ala.
- -
Unsightly scarring.
- -
Free cartilage grafts from the ear, nasal septum, or ribs; these are more laborious techniques with a high risk of necrosis.
- -
Alloplastic materials (titanium or polyethylene mesh). Experience is necessary with these materials. There is a risk of infection, extrusion of the material, or a trap-door effect, which would require reoperation.
- -
Inverted melolabial flap; this does not provide cartilage support.
Although chondromucosal flaps from the adjacent ala and the melolabial flap are extensively described in the literature, the combination of the 2 flaps has not previously been reported.
We present this combined flap as an excellent option for the reconstruction of partial, full-thickness defects of the alar and perialar regions of the nose. This method of reconstruction offers cartilaginous support without the need for alloplastic materials and with a lower risk of necrosis than other options. This simple and original technique is performed in a single operation under local anesthesia and will stimulate the creative capacity of the dermatologic surgeon.
Please cite this article as: Valladares-Narganes L, González-Sixto B, Otero-Rivas M, Rodríguez-Prieto M. Colgajo mio-condro-mucoso de rotación combinado con colgajo de trasposición melo. Actas Dermosifiliogr. 2013;104:821–823.