The patient was a 24-year-old woman with no relevant medical history. She presented with a raised lesion on her back that caused discomfort when it came into contact with her clothing. This lesion had appeared on 1 of several asymptomatic plaques that had been present on her back since birth and had grown along with the patient.
Physical ExaminationThe patient's presenting complaint was a brown verrucous lesion clinically suggestive of intradermal melanocytic nevus without atypia. Of greater interest, however, was the presence of multiple well-defined, slightly raised, smooth brown plaques of different sizes that showed no scaling. The plaques were located close together, but without coalescing, on the lower back region and on the right side of the back, stretching as far as the ipsilateral shoulder (Figs. 1 and 2). The patient had no hypopigmented, periungual, or facial skin lesions.
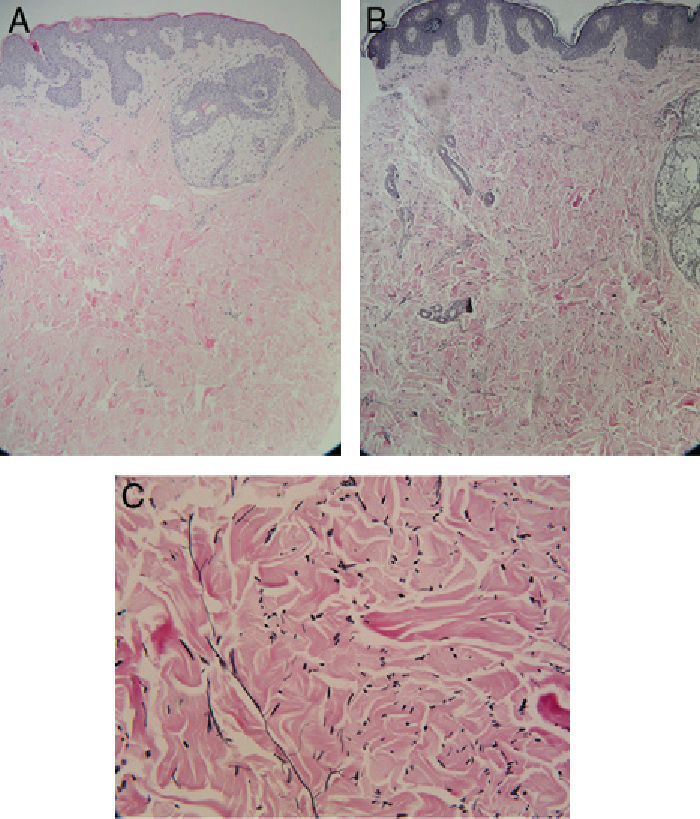
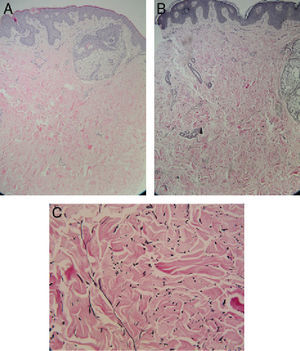
HistopathologyBiopsy of the congenital lesions showed thickened dermal collagen bundles and no epidermal abnormalities. Verhoeff-van Gieson staining revealed elastic fibers that were thinner than those found in normal skin (Fig. 3). The sebaceous glands exhibited no changes.
What Is Your Diagnosis?
DiagnosisMultiple grouped congenital collagenomas on the back.
Clinical Course and TreatmentThe patient had no hereditary diseases, no family history of similar lesions, no history of neurocutaneous syndromes, and no skin lesions characteristic of tuberous sclerosis. Because the lesions were asymptomatic, benign, and extensive, no treatment was given.
CommentReticular connective tissue nevi are classified according to the component present in unusually large amounts; they are known as collagenomas when there are elevated levels of collagen fiber and as elastomas when there are elevated levels of stromal proteoglycans.1
Collagenomas, or collagenous connective tissue nevi, are hamartomatous lesions of the dermis with increased collagen levels. They can be either hereditary or sporadic, and are usually present at birth or appear in early childhood, although acquired forms also exist. They present as firm skin-colored or lightly pigmented papules, nodules, or plaques, and can be solitary, multiple, or even segmental; they can occur on any part of the body.
Several types of collagenoma have been described, including familial cutaneous collagenoma, which follows an autosomal dominant pattern of inheritance, presents as multiple lesions, usually on the trunk during adolescence, and is associated with cardiovascular and systemic disorders.2 Eruptive collagenomas are clinically indistinguishable from familial cutaneous collagenomas, except for the fact that family history is negative and onset is abrupt. Plantar cerebriform collagenoma can occur in isolation but is usually associated with Proteus syndrome.3 The shagreen patch is a form of collagenoma that usually occurs on the lower back of patients with tuberous sclerosis. Other types of connective tissue nevi include knuckle pads, collagenomas associated with Down syndrome, ichthyosis, multiple fibrofolliculomas, cardiomyopathy, and hypogonadism; there have also been reports of collagenomas in Cowden syndrome4 (storiform collagenomas), multiple endocrine neoplasia type 1, and Ehlers-Danlos syndrome.
Collagenomas are histologically characterized by the proliferation of connective tissue due to an increase in collagen fibers—especially type I collagen, the most abundant form of collagen in the dermis—and a resulting proportional decrease in elastic fibers.
Although the etiology and pathogenesis of connective tissue nevi are unknown, sporadic collagenomas may be related to trauma, since they appear most frequently in areas subject to friction.
We found no signs or symptoms of neurocutaneous disease in our patient and were thus able to rule out the presence of shagreen patches, which are a manifestation of tuberous sclerosis and a key consideration in the differential diagnosis.
Collagenomas can be treated, purely for cosmetic reasons, with surgery, although some cases have been treated successfully with intralesional corticosteroids.5
The literature contains few cases of congenital giant or multiple grouped collagenomas occurring in isolation, rather than in association with another disease.6 The clinical cases that have been reported describe a large plaque formed by the coalescence of multiple lesions. Our case is the first reported instance of multiple independent, yet closely grouped, collagenomas covering such a large area of the body.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rodríguez-Vázquez M, et al. Múltiples placas asintomáticas congénitas en la espalda. Actas Dermosifiliogr. 2012;103:241–242.