Postirradiation morphea is a rare complication that may develop in areas treated for cancer with radiation therapy, usually in breast cancer patients. We present the case of a patient with carcinoma of the breast treated with surgery and radiation therapy who developed postirradiation morphea 1 year later.
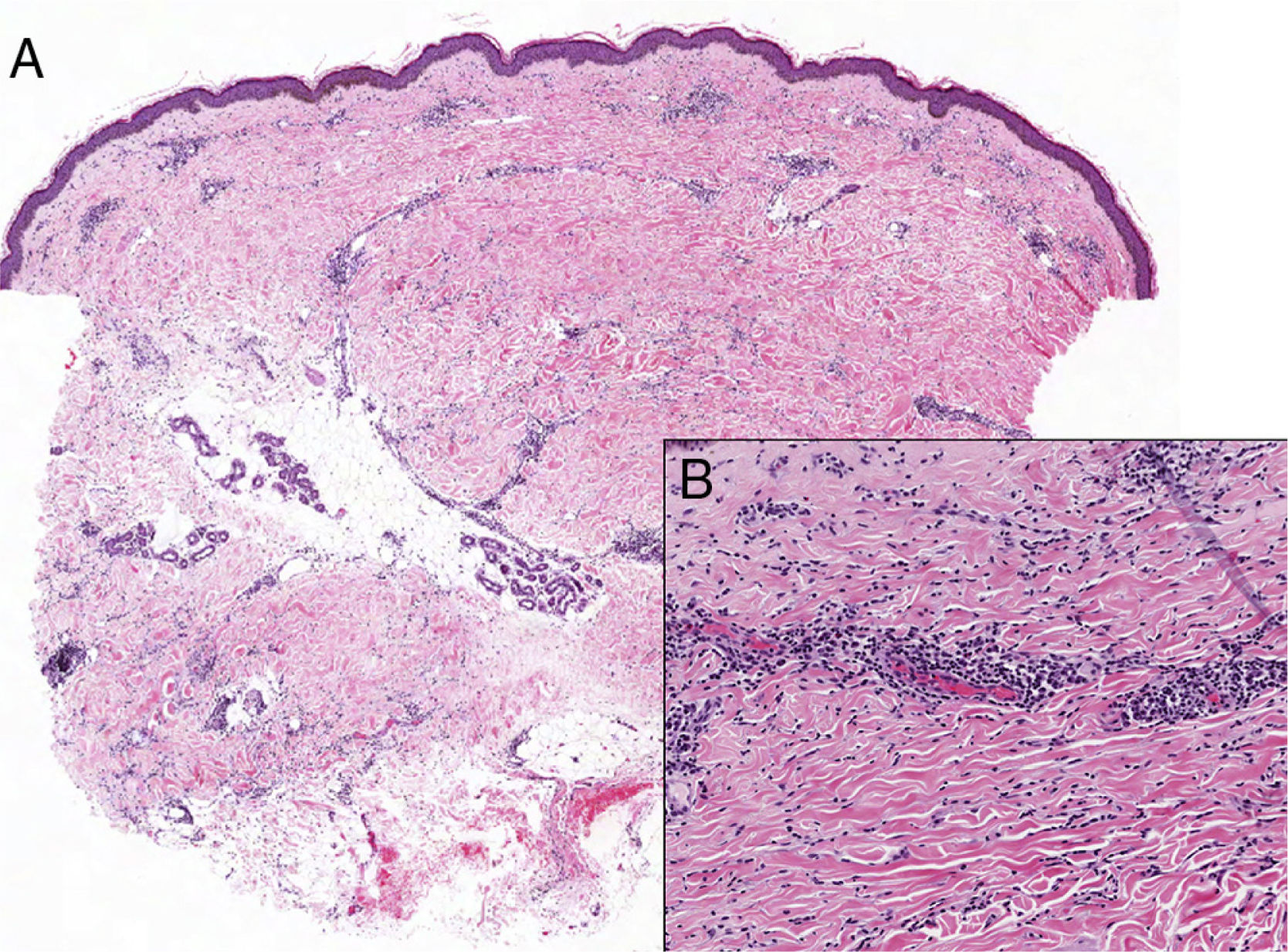
The patient was a 56-year-old woman who had been diagnosed with infiltrating ductal carcinoma of the left breast and treated with lumpectomy. Sentinel node biopsy results were negative. The patient had received adjuvant treatment consisting of chemotherapy, letrozole endocrine therapy, and external beam radiation therapy applied to the mammary gland using 6- and 18-MeV photons at a dose of 50Gy followed by boost irradiation of the tumor bed at a dose of 66Gy. Treatment was well tolerated. One year after completion of radiation therapy, there was a sudden onset of painful induration of the left breast, which also decreased in size. Physical examination revealed asymmetry of the two breasts and a well-demarcated woody plaque with an erythematous border in the irradiated area (Fig. 1). Biopsy showed slight atrophy of the epidermis, hyperpigmentation of the basal layer, thickening of dermal collagen, loss of adnexal structures, and a discrete perivascular and interstitial lymphoplasmacytic inflammatory infiltrate that was both deep and superficial, with few interstitial eosinophils in the deep dermis (Fig. 2). Immune status was normal and serological testing for Borrelia was negative. Magnetic resonance imaging and mammography showed no abnormalities of the mammary gland. After treatment with oral prednisone at a dose of 0.5mg/kg/d tapered over 2 months and topical treatment with clobetasol, the patient's pain disappeared, induration and erythema decreased, and occasional vesicles developed. One year later the patient remained stable without tumor recurrence.
A, Low-magnification view showing decreased adnexal structures as well as an interstitial and mildly perivascular lymphoplasmacytic inflammatory infiltrate, both superficial and deep. Hematoxylin-eosin, original magnification ×40. B, Higher magnification shows collagen thickening. Hematoxylin-eosin, original magnification ×100.
Radiation dermatitis, both acute and chronic, is a frequent reaction to treatment, whereas postirradiation morphea is a much rarer occurrence. The first cases of postirradiation morphea were described in 1989 by Colver et al1 in 9 patients. Breast-conserving surgery with adjuvant radiation therapy has become the standard treatment in patients with early-stage breast cancer, who have the highest rate of postirradiation morphea. In one series of female patients with breast cancer the incidence rate was found to be 3 per 6000 patients, which was clearly higher than the 2.7 cases per 100 000 persons per year for the general population.2
Our review of the literature found 68 cases of postirradiation morphea in patients aged 34 to 85 years,1–9 an older population than that with idiopathic morphea. Most patients were white. The majority were women with carcinoma of the breast treated with breast-conserving surgery, though some had undergone mastectomy. One patient also had carcinoma of the endometrium,7 and a small minority of patients had nonbreast cancer (2 had cervical cancer,1,3 1 had axillary adenocarcinoma of unknown origin,1 and 1 had cancer of the endometrium6). There were 4 men with personal histories of subcutaneous lymphoma, carcinoma of the tongue,3 gastric cancer,4 and neck node metastatic cancer of unknown primary site.5
Morphea typically develops within a year of radiation therapy, but has been seen up to 32 years later (range, 1 month to 32 years). Onset is sudden with an inflammatory stage that involves a rapidly growing, generally painful erythematous or violaceous plaque in the irradiated area. Progression leads to plaque induration and pigmentation. Ultimately, these changes cause breast retraction and size reduction, although the mammary gland is not affected. Vesicles and bullae may develop,8 as in our patient's case. In over 25% of cases, induration extends beyond the irradiated area or even spreads to distant areas. One case report describes linear lesions on the lower limbs.6 As with idiopathic morphea, histology varies with disease progression.
The etiology of postirradiation morphea is unknown at present, but age, total radiation dose, dose per fraction, number of fractions, and grade of acute radiodermatitis do not appear to matter. However, risk appears to be higher for patients with connective tissue disorders, chiefly lupus erythematosus and scleroderma.8 The reason for the predominant location on the breast is also unknown, but may have to do with the abundance of fatty tissue and the radiation dose received on overlying skin. Thanks to modern linear accelerators and techniques that achieve dose conformity by modulating the intensity of the radiation beam, skin damage from radiation therapy is minimal. In the breast, however, the skin and fat are included in the irradiated volume because they are close to the irradiation field and become the target organ in postmastectomy patients. This may explain the higher rate of postirradiation morphea on the breast.
Many adverse skin reactions to radiation therapy have been described (Table 1). Some are included in the differential diagnosis for postirradiation morphea. In the inflammatory phase, differential diagnosis includes infection, radiation recall dermatitis, and above all tumor recurrence (erysipelas-like cutaneous metastasis, carcinoma en cuirasse, or carcinomatous mastitis).
Adverse Skin Reactions to Radiation Therapy.
| Acute radiodermatitis |
| In the early weeks. Erythema, edema, alopecia, changes in color. |
| Chronic radiodermatitis |
| Months or years after radiation therapy. Poikiloderma. |
| Radiation-induced fibrosis |
| Within the spectrum of chronic radiodermatitis. |
| Within the first 3 months. Dose-dependent. Deep tissues in the irradiated area are affected without inflammation. |
| Histology: Deep subcutaneous fibrosis, involving even the fascia and muscles. |
| Panniculitis following radiation therapy10 |
| Possible variant of postirradiation morphea. Women with breast cancer, months after radiation therapy. |
| Histology: Lobular panniculitis with adipocyte necrosis and dense inflammatory infiltrate of foamy histiocytes. |
| Primary skin malignancies: angiosarcoma, dermatofibrosarcoma protuberans, basal cell carcinoma, Merkel cell carcinoma |
| Changes in melanocytic nevi |
| Vascular lesions |
| Radiation recall dermatitis |
| Lichen sclerosus et atrophicus |
| Cutaneous and mucosal lichen planus |
| Polymorphic, itchy, eosinophilic rash |
| Psoriasis |
| Vitiligo |
| Autoimmune bullous disorders (pemphigus vulgaris, pemphigus foliaceus, bullous pemphigoid) |
| Autoimmune diseases of connective tissue (lupus erythematosus, dermatomyositis) |
| Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme |
| Sweet syndrome |
For follow-up of postirradiation morphea patients, ultrasound imaging is recommended instead of mammograms. While the natural history of this condition is poorly understood, it may improve after months or years, although asymmetry and pigmentation will persist. No effective treatment has been described. Treatment is as for idiopathic morphea, but immunosuppressive agents are not recommended. Treatments attempted include topical, intralesional, and systemic corticosteroids, topical calcipotriol, intravenous penicillin, hydroxychloroquine, phototherapy, and methotrexate (2.5-15mg/wk). In extreme cases with very severe pain, palliative mastectomy may be necessary, but reconstructive surgery is contraindicated.
Please cite this article as: García-Arpa M, Lozano-Martín E, Ramos-Rodríguez C, Rodríguez-Vázquez M. Morfea tras radioterapia en paciente con cáncer de mama. Actas Dermosifiliogr. 2015;106:243–245.