Molluscum contagiosum (MC) is a very common infectious dermatosis. It is caused by a double-strand DNA virus of the same name, which belongs to the Poxviridae family. Estimated prevalence is 7% in children and up to 18% in immunocompromised adults. The virus is transmitted by direct contact, fomites, or autoinoculation, and manifests clinically in the form of cupuliform umbilicated papules that the same color as the skin and generally asymptomatic. The papules infrequently appear on glabrous skin.1
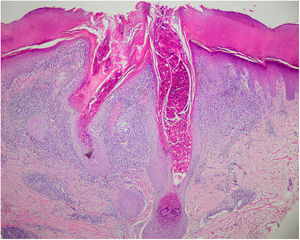
A 43-year-old man with no past medical history of interest visited our department with 2 lesions on the right hand; the lesions caused discomfort when pressed or rubbed and had appeared a week earlier. Physical examination revealed 2 erythematous papules on the hypothenar region of the left palm, with diameters of 2 and 4mm, respectively. Both lesions were slightly infiltrated to the touch and the larger lesion showed central hyperkeratosis and a perilesional erythematous halo (Fig. 1). The rest of the physical examination was normal. One of the lesions was excised and biopsied, and showed lobulation of the epidermis toward the dermis, and keratinocytes with intracytoplasmic inclusion bodies (Fig. 2). The diagnosis of palmar MC was established based on these findings and the other lesion was treated using cryotherapy. Both lesions resolved completely a month after treatment.
In children, infection by the MC virus tends to be located on the face, torso, and extremities. In adults, the most frequent site is in the genital region and surrounding areas.2 Involvement of the palms and soles is exceptional regardless of age. The first case of plantar MC was published by Ingram et al.3 in 1957. To date, a total of 37 cases have been described but only 13 are well documented (Table 1). Involvement of the palms, however, was first described by Legrain and Pierard4 in 1985 and no new cases have been published to date.
Well-Documented Clinical Cases of Infection With Plantar or Palmar Molluscum Contagiosum to Date.
| Reference | Sex and Age | Number of Lesions | Largest Diameter, cm | Site | Pain |
|---|---|---|---|---|---|
| Baxter y Carson6 (1964) | Male, 21 years | 50-60 | 0.1 | LF | No |
| Perry GM (1964) | Female, 31 years | 1 | ND | RF | ND |
| Strani (1967) | Female, 75 years | 1 | ND | LF | Yes |
| Strani (1967) | Male, 7 years | 1 | ND | RF | Yes |
| Bunney et al. (1969) | Female, 21 years | >5 | ND | LF | ND |
| Zichichi (1969) | Male, 23 years | 1 | 1.5 | RF | Yes |
| Campanelli et al. (1978) | Female, 17 years | 1 | 1.2 | RF | Yes |
| Dickinson et al. (1983) | Male, 21 years | 2 | 1/0.3 | LF/RF | ND |
| Ha et al. (1998) | Male, 5 years | 1 | 1.5 | LF | Yes |
| Köse et al. (2009) | Female, 35 years | 1 | 0.5 | LF | Yes |
| Cohen and Tschen5 (2012) | Male, 23 years | 3 | 0.8/0.8/0.8 | RF | Yes |
| Aydoğan et al.7 (2014) | Male, 26 years | 1 | 1 | RF | No |
| Bahali et al.8 (2016) | Male, 36 years | >10 | 0.4-2 | LF | Yes |
| García-Montero et al. (2017) | Male, 48 years | 2 | 0.2/0.4 | LH | Yes |
Abbreviations: LH indicates left hand; ND, not described; RF, right foot, LF, left foot.
The diagnosis of palmar or plantar MC is rarely initially suspected because, as with our patient, the lesions do not tend to present the usual characteristics of infection by this virus. On the soles of the feet, clinical manifestations have been described as single or multiple papules or nodules with varying coloration (normal skin, erythematous, brown, translucent, yellow) and with hyperkeratotic, verrucous, or crusted.5 Only Baxter et al. documented a case in which the lesions presented as umbilicated papules with a central keratin plug.6 Clinical history cannot always guide diagnosis. Our patient had not suffered from this infection in the past, had no lesions in other areas at the time of the consultation, had not been in situations with a risk of infection, and only noted that one of his children had had MC a year earlier.
While infection with the MC virus is more frequent in childhood and in immunocompromised patients, most cases of palmoplantar involvement, including our case, have been reported in adults, and none patients in the published cases were immunocompromised. Past history of trauma or plantar hyperhidrosis have been identified in some patients and it is thought that they may have acted as predisposing factors.7,8 Given that this is a highly prevalent infection, it is not known why it is not seen in this location more frequently, unlike papilloma virus. It may be that the thickness of the stratum corneum on the palms and soles makes entry of the poxvirus more difficult, as it is much larger (150-300nm) than the human papilloma virus (60nm). Palmoplantar involvement also shows that the virus replicates in the keratinocytes and does not require hair follicles.
The differential diagnosis with this type of lesion on the palms or soles is extensive and includes viral warts, pyogenic granuloma, foreign body granuloma, pleomorphic fibroma, carcinoma cuniculatum, and eccrine poroma. Treatment of palmoplantar MC is the same as at other sites.9 In our patient, a single cycle of cryotherapy was effective and the lesions resolved completely in 1 month.
In conclusion, we report the second case of MC on the palm of the hand to date. This entity should be considered when we find papular lesions on the palms or soles, especially in patients with a personal or family history of risk, in order to perform a correct diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Montero P, Serrano-Pardo R, Ruiz-Rodríguez R, Sánchez-Carpintero I. Molusco contagioso palmar, una localización excepcional. Actas Dermosifiliogr. 2019;110:615–617.