Graft-vs-host disease (GVHD) is a clinical syndrome that occurs when immunocompetent donor cells attack various host tissues, with the skin, gastrointestinal tract, and liver being the main target organs.1 The onset of skin involvement in chronic GVHD is usually more than 100 days posttransplant. Signs basically consist of lichenoid eruptions and sclerodermoid manifestations, although many other patterns have also been described.2 We report a new case of lichenoid chronic GVHD following Blaschko lines.
A 16-year-old boy was seen for a pruritic, linear rash on his left upper limb and the trunk that had appeared 2 weeks earlier. The patient had previously been diagnosed with a blastic plasmacytoid dendritic cell neoplasm, which was in complete remission following chemotherapy and an allogeneic bone marrow transplant with complete hematopoietic chimerism. He also had a history of acute cutaneous and intestinal GVHD. At the time of consultation, 20 months after the transplant, the patient was on low doses of methylprednisolone and ciclosporin and reported no history of herpes zoster.
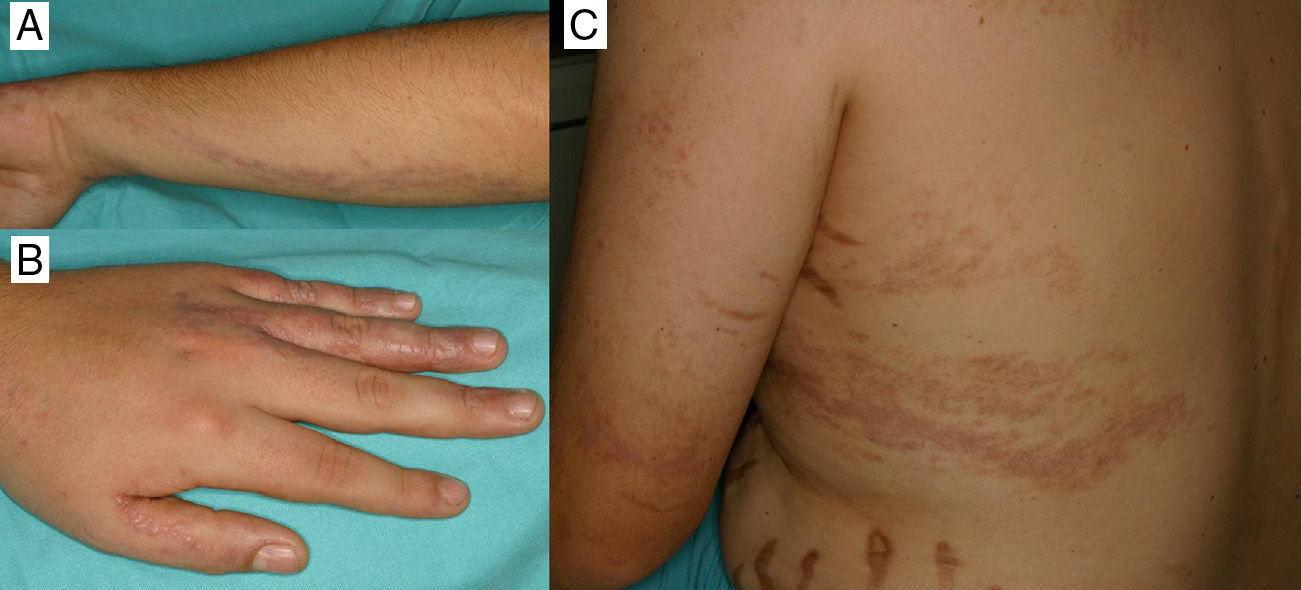
Physical examination revealed 2 linear eruptions on the left upper limb—1 posterointernal and 1 posteroexternal—extending from the shoulder to the distal part of the dorsum of the first, third, fourth, and fifth fingers, respectively, of the left hand. The patient also had 3 similar S-shaped lesions on the left hemithorax that followed Blaschko lines (Fig. 1, A-C). The lesions consisted of flat, erythematous-violaceous papules measuring 1 to 3mm that tended to coalesce. The physical examination was otherwise unremarkable.
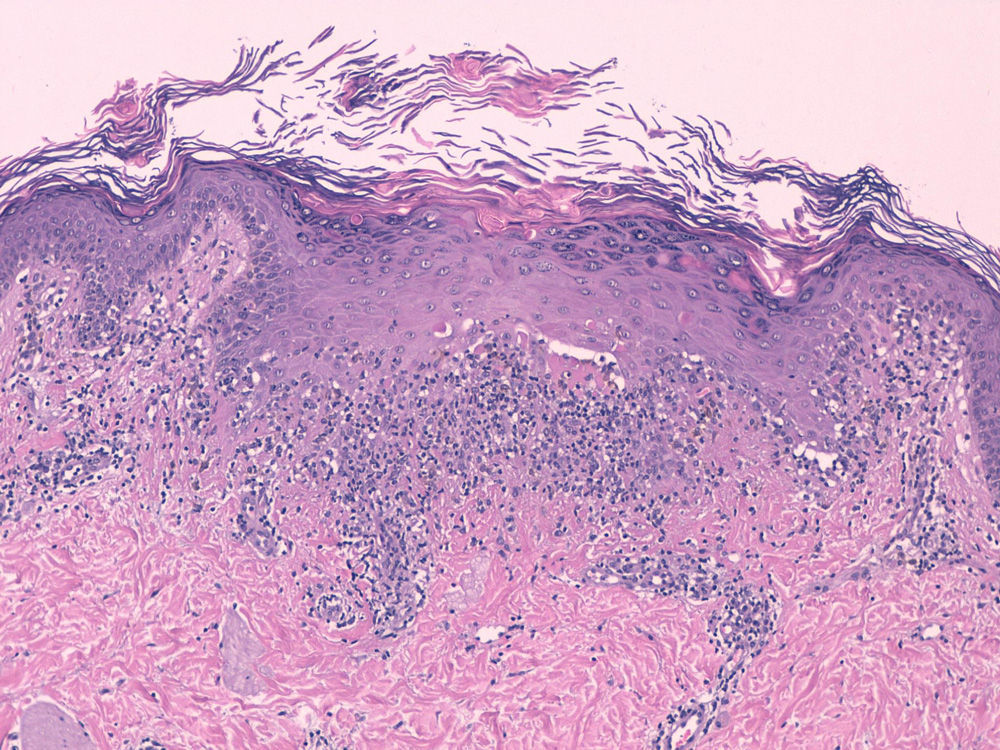
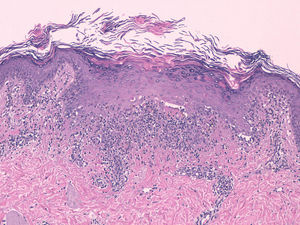
Biopsy of a papule revealed features suggesting lichenoid dermatitis (Fig. 2). The patient was diagnosed with lichenoid chronic GVHD following Blaschko lines and, because no extracutaneous involvement was present, high-potency topical corticosteroids were prescribed. The lesions resolved after 1.5 months, leaving a slight hyperpigmentation.
Given the presence of an acquired linear lichenoid eruption along Blaschko lines, we considered the following differential diagnoses: linear lichen planus, lichen striatus, inflammatory linear verrucous epidermal nevus, linear porokeratosis, and linear psoriasis.1,3–6 Nevertheless, given the patient's history of allogeneic bone marrow transplantation, localized lichenoid chronic GVHD was the first option.
Chronic cutaneous GVHD can follow 2 main patterns: lichenoid eruptions and sclerodermoid manifestations. Other, less frequent manifestations include xerosis, poikiloderma, keratosis pilaris, ichthyosis, psoriasiform lesions, palmoplantar eczema, erythroderma, exfoliative dermatitis, and manifestations that mimic other annular dermatoses such as pityriasis rosea, centrifugal annular erythema, erythema multiforme, and subacute lupus. Most patients present generalized lesions but localized linear lesions, both lichenoid and sclerodermoid, have also been reported. Some lesions follow Blaschko lines, whereas others—with or without a history of herpes zoster in the same area—follow a metameric pattern.1–10
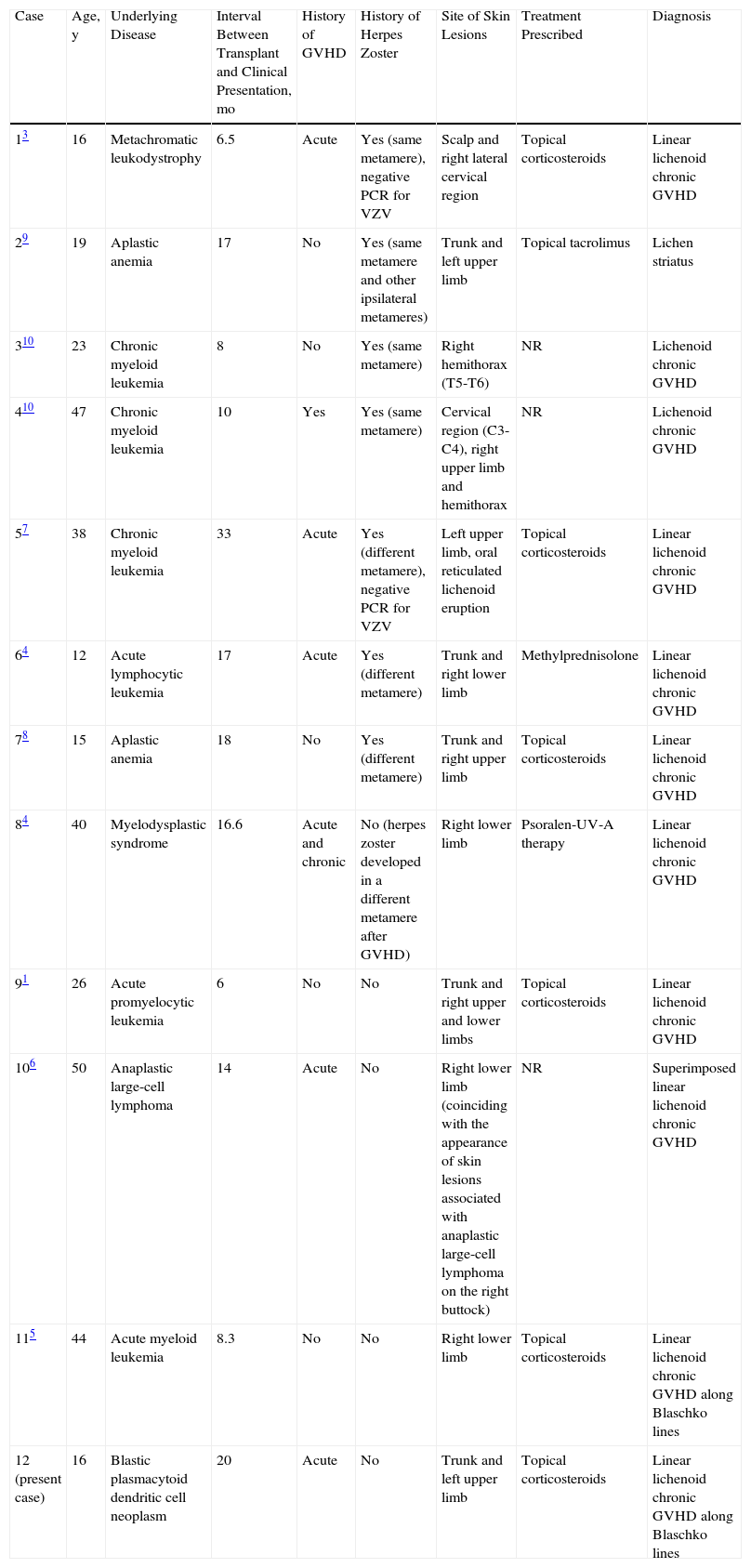
We found 11 reported cases of lichenoid chronic GVHD (Table 1). More than half of these patients had a history of acute GVHD. A prior history of herpes zoster was present in 7 patients, 4 of whom developed lichenoid papules in the same metameres that had been affected by the viral infection. Topical corticosteroids were prescribed to 6 patients, topical tacrolimus to 1 patient, oral methylprednisolone to 1 patient, and psoralen-UV-A therapy to 1 patient.1,3–10
Characteristics of Published Cases of Linear Lichenoid Graft-vs-Host Disease.
| Case | Age, y | Underlying Disease | Interval Between Transplant and Clinical Presentation, mo | History of GVHD | History of Herpes Zoster | Site of Skin Lesions | Treatment Prescribed | Diagnosis |
| 13 | 16 | Metachromatic leukodystrophy | 6.5 | Acute | Yes (same metamere), negative PCR for VZV | Scalp and right lateral cervical region | Topical corticosteroids | Linear lichenoid chronic GVHD |
| 29 | 19 | Aplastic anemia | 17 | No | Yes (same metamere and other ipsilateral metameres) | Trunk and left upper limb | Topical tacrolimus | Lichen striatus |
| 310 | 23 | Chronic myeloid leukemia | 8 | No | Yes (same metamere) | Right hemithorax (T5-T6) | NR | Lichenoid chronic GVHD |
| 410 | 47 | Chronic myeloid leukemia | 10 | Yes | Yes (same metamere) | Cervical region (C3-C4), right upper limb and hemithorax | NR | Lichenoid chronic GVHD |
| 57 | 38 | Chronic myeloid leukemia | 33 | Acute | Yes (different metamere), negative PCR for VZV | Left upper limb, oral reticulated lichenoid eruption | Topical corticosteroids | Linear lichenoid chronic GVHD |
| 64 | 12 | Acute lymphocytic leukemia | 17 | Acute | Yes (different metamere) | Trunk and right lower limb | Methylprednisolone | Linear lichenoid chronic GVHD |
| 78 | 15 | Aplastic anemia | 18 | No | Yes (different metamere) | Trunk and right upper limb | Topical corticosteroids | Linear lichenoid chronic GVHD |
| 84 | 40 | Myelodysplastic syndrome | 16.6 | Acute and chronic | No (herpes zoster developed in a different metamere after GVHD) | Right lower limb | Psoralen-UV-A therapy | Linear lichenoid chronic GVHD |
| 91 | 26 | Acute promyelocytic leukemia | 6 | No | No | Trunk and right upper and lower limbs | Topical corticosteroids | Linear lichenoid chronic GVHD |
| 106 | 50 | Anaplastic large-cell lymphoma | 14 | Acute | No | Right lower limb (coinciding with the appearance of skin lesions associated with anaplastic large-cell lymphoma on the right buttock) | NR | Superimposed linear lichenoid chronic GVHD |
| 115 | 44 | Acute myeloid leukemia | 8.3 | No | No | Right lower limb | Topical corticosteroids | Linear lichenoid chronic GVHD along Blaschko lines |
| 12 (present case) | 16 | Blastic plasmacytoid dendritic cell neoplasm | 20 | Acute | No | Trunk and left upper limb | Topical corticosteroids | Linear lichenoid chronic GVHD along Blaschko lines |
Abbreviations: GVHD, graft-vs-host-disease; NR, not reported; PCR, polymerase chain reaction; VZV, varicella zoster virus.
Several hypotheses have been proposed to explain the pathophysiology of this unusual pattern. Lesions distributed along Blaschko lines might be caused by an underlying somatic mosaicism (a mutation during embryonic development). This cell clone would be tolerated by the host's immunocompetent cells until it is unmasked by the donor cells. According to other theories, metameric patterns of GVHD—whether of lichenoid or sclerodermoid lesions—may be associated with the clinical or subclinical reactivation of the varicella zoster virus. With reactivation, the immunologic characteristics of the keratinocytes become altered, causing them to be attacked by donor lymphocytes (isotopic response, in which a dermatosis occurs at the site of a different healed disease). There have also been cases of sclerodermoid GVHD involving lesions that affect previously irradiated or injured zones. In such cases, the pathophysiological mechanism would be the underlying disease (a Köbner isomorphic response, in which new lesions appear in previously damaged areas). These 2 mechanisms can overlap.1,3,4,7–11
Differential diagnosis between linear lichenoid GVHD and ordinary linear lichen planus is practically impossible. In linear lichenoid GVHD, the papules are less angular, less well-defined, and can be associated with other manifestations of acute sclerodermoid GVHD or poikiloderma. Histologically, both processes are characterized by features of lichenoid dermatitis, although in GVHD the lymphohistiocytic infiltrate is more disperse and follows a perivascular and periadnexal distribution.1,5
In our patient's case—following an allogeneic bone marrow transplantation—the clinical and histologic findings support a diagnosis of lichenoid chronic GVHD distributed along Blaschko lines. In a patient with complete hematopoietic chimerism, this dermatosis would have been caused by the immunocompetent donor cells’ reaction to the host and therefore satisfies the immunologic criteria required for a diagnosis of GVHD. The fact that the disease exclusively affected the skin along Blaschko lines is explained by the presence of a latent somatic mosaicism in the host, which was unmasked by the donor cells.
Please cite this article as: Kennedy FE, Hilari H, Ferrer B, Garcia-Patos V. Enfermedad del injerto contra el huésped crónica liquenoide con patrón blaschkoide. Actas Dermosifiliogr. 2014;105:89–92.