Lichen sclerosus is a chronic inflammatory disease that has a particular affinity for the anogenital region. Only 6% of patients present solitary extragenital lesions, although this percentage can rise to 15% during childhood.1
We present the case of a patient with lichen sclerosus lesions following a jellyfish sting in the context of Koebner phenomenon.2
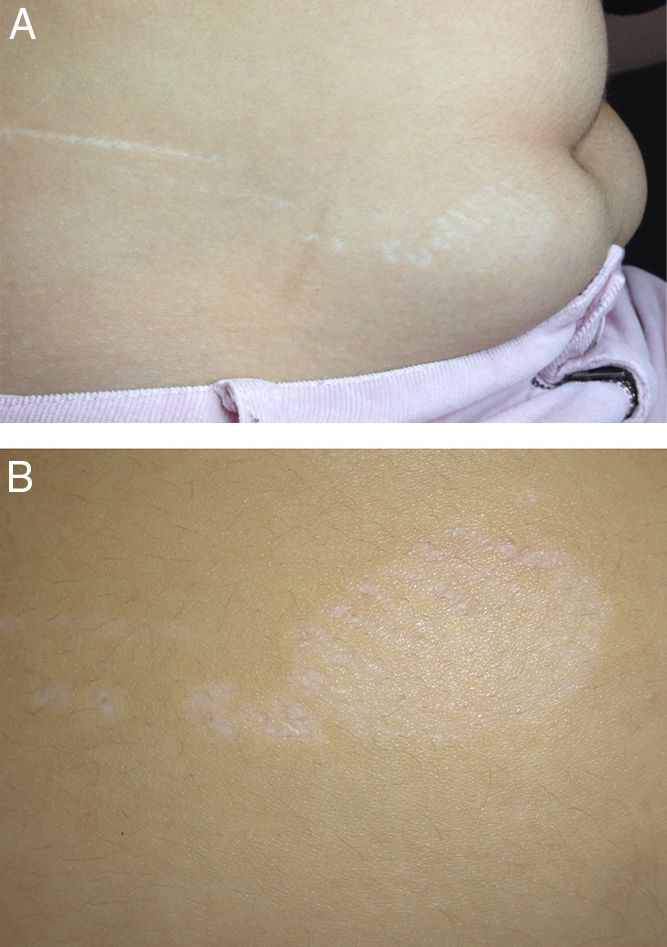
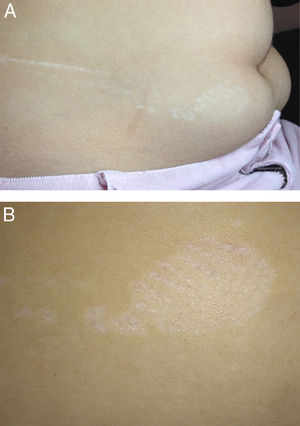
The patient was a 13-year-old girl with an unremarkable family history who consulted for a whitish, atrophic, and pruriginous plaque on the vulva and gluteal cleft, together with whitish indurated papules spread throughout the trunk. A skin biopsy revealed orthokeratotic hyperkeratosis in the epidermis, with hydropic degeneration and atrophy of the basal layer, in addition to edema and homogenization of collagen. The patient was treated with topical tacrolimus and her lesion improved considerably after 4 months. One year later, while asymptomatic, she was stung by a jellyfish. Papules and plaques appeared in a linear pattern (17cm long) on the right abdomen. These were clinically compatible with lichen sclerosus lesions (Fig. 1A) and very probably originated as a result of Koebner phenomenon (Fig. 1B). The patient refused a second skin biopsy, since she was receiving treatment with topical tacrolimus and was progressing favorably. She now has small active lesions on the genital region.
Lichen sclerosus can occur at any age, although the peak incidence is noted in childhood and after the menopause.2 It most commonly appears on the anogenital region and, even though it is not unusual for it to be accompanied by extragenital lesions, involvement of these areas alone is very infrequent. The etiology of lichen sclerosus is unknown. Possible causes include a hormonal disorder, autoimmune mechanisms, infection (eg, human papilloma virus, hepatitis C, Borrelia burgdorferi), genetic factors associated with various HLA subtypes, and repeated insults associated with the appearance of new lesions due to the Koebner phenomenon that is typical of lichen sclerosus.3,4 Koebner phenomenon is caused by damage to the dermis and, especially, the epidermis, which is the main event in its development. This event causes an increase in levels of CD4 lymphocytes, cytokines, and adhesion molecules that could lead to the appearance of lesions that are typical of associated diseases, such as, in the present case, lichen sclerosus.4 The lesions of lichen sclerosus are typically ivory-white papules and macules that are clearly defined and can coalesce to form plaques, as occurred in the case we report. Furthermore, the presence of dilated pilosebaceous openings containing keratin plugs, purpura, and telangiectasia are usually characteristic signs.3,4 The differential diagnosis for the case we present included lichen planus, lichen simplex chronicus, vitiligo, and lichen planus–like lesions. Bullous diseases affecting the mucosa, pemphigoid, and intraepithelial neoplasms of the penis and vulva should be taken into consideration in anogenital lichen sclerosus.5,6
Our case is exceptional because of the way the lesions appeared and their morphology, since the mark left by the jellyfish tentacles was visible. Jellyfish stings usually cause acute local reactions characterized by a burning sensation and pruritus. The lesions are most often erythematous papules or papulovesicles and may be accompanied by regional vascular and lymphatic reactions.7 Although less frequent, delayed reactions are not uncommon; the most frequents reactions are keloids, pigmented striae, lichenified lesions, granuloma, ulceration, and necrosis.8 Gangrene, fat atrophy, and retractile scars are less typical, although they have been reported in the literature.8 In the case we report, the lesions were clinically compatible with lichen sclerosus, although they had taken on the morphology of the tentacles of the jellyfish that had stung the patient, thus constituting another potential late complication that should be taken into account in the differential diagnosis of jellyfish stings.8
Please cite this article as: Pérez-López I, Garrido-Colmenero C, Blasco-Morente G, Tercedor-Sánchez J. Fenómeno de Koebner en un liquen escleroso tras una picadura de medusa: una morfología excepcional. Actas Dermosifiliogr. 2015;106:238–239.