A 87 year-old-man presented with a two-month history of pruritic lesions on the scrotal area. He developed a similar episode one year earlier, that lasted for a couple of weeks and improved spontaneously. There were no associated cutaneous or extracutaneous symptoms.
He was chronically under enalapril and allopurinol, but denied the introduction of new systemic drugs or the application of skin products on that area.
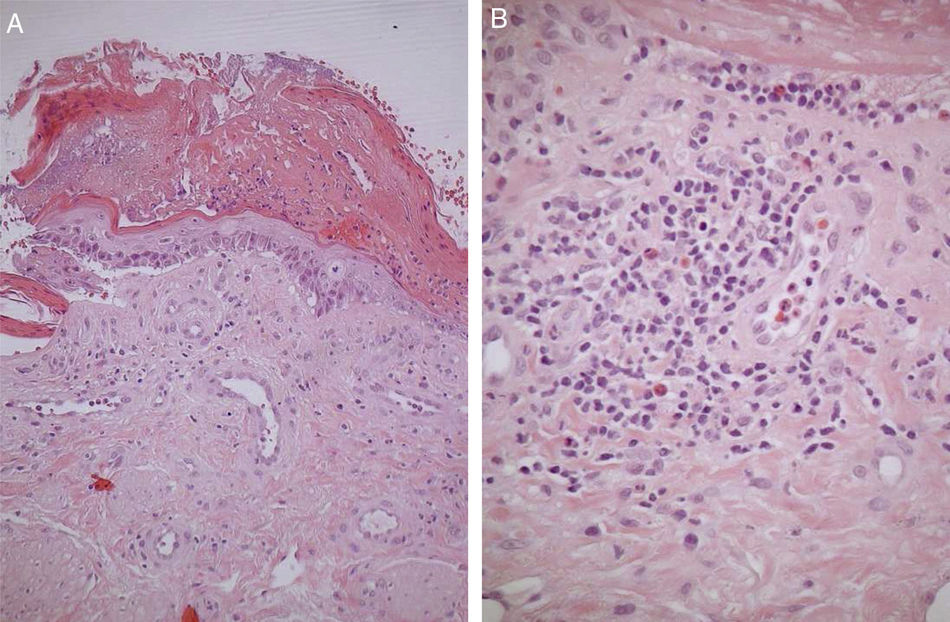
Physical examinationOn physical examination we observed several tense bullae and vesicles located on the scrotal area, filled with clear citric fluid, grouped over erythematous patches (Fig. 1). Some of the lesions had already ruptured, leaving eroded and crusted areas. He had no other cutaneous or mucosal lesions. Nikolsky’s and Asboe-Hansen’s sings were negative.
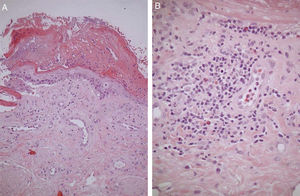
Histopathologic evaluationA punch biopsy specimen was obtained for histopathologic evaluation, revealing a subepidermal blister (Fig. 2A) accompanied by a dermal inflammatory infiltrate composed of mononuclear cells and eosinophils (Fig. 2B).
Other TestsDirect immunofluorescence was temporarily unavailable, however indirect immunofluorescence and ELISA revealed IgG autoantibodies directed against bullous pemphigoid (BP) antigen 230, on a titer of 56.9 U/mL (N < 20).
What is the diagnosis?
DiagnosisGenital bullous pemphigoid (GBP).
Clinical Course and TreatmentThe patient then began treatment with ultrapotent topical corticosteroids (0.05% clobetasol propionate ointment once a day), leading to complete resolution of skin lesions over the course of 4 weeks. No recurrence was observed during a 6-month follow-up.
CommentBullous pemphigoid (BP) is a common autoimmune subepidermal blistering disease, presenting typically in the elderly patients as a generalized pruritic bullous eruption. This entity is an example of an immune-mediated disease that is associated with a humoral and cellular response directed against two self-antigens: BP antigen 180 and BP antigen 2301,2. The clinical presentation can be rather polymorphic, particularly during the early stages of the disease or in atypical variants.
Localized BP is a clinical variant of bullous pemphigoid and its exact pathogenesis is yet to be elucidated, although factors such as trauma, ultraviolet light and hydrostatic pressure have been proposed3. Genital bullous pemphigoid (GBP) is a rarely reported localized subset4,5 that affects mainly women and paediatric patients. GBP in adult men is exceptionally rare, and to our knowledge only three cases were previously reported6.
The clinical differential diagnosis of GBP includes several other conditions, such as acute eczema, herpetic and fungal infections, epidermolysis bullosa and linear IgA disease. Clinical-pathological correlation is of major importance, and these entities can be differentiated on the basis of distinctive immunopathologic findings and clinical context. Early diagnosis will help avoid unnecessary and costly treatment for unrelated conditions.
Please cite this article as: Alves F, Pinho A, Cardoso JC. Ampollas aisladas del escroto en un varón de 87 años. Actas Dermosifiliogr. 2021;112:449–450.