Reconstruction of defects of the eyelids after oncologic surgery can be complex. The techniques required at this site can be some of the most difficult in dermatologic surgery. After appropriate oncologic surgery to the eyelids, reconstruction must be extremely precise in order to preserve palpebral function.1 Optimal cosmetic and functional results can be achieved if, additionally, care is taken with a series of intraoperative factors.
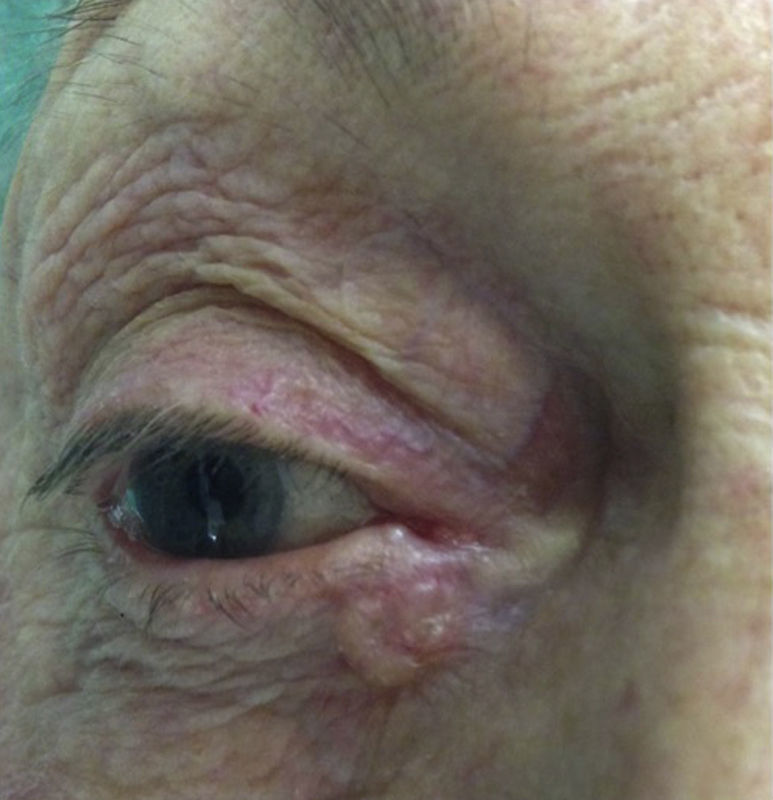
Description of the TechniqueWe present the surgical excision of a basal cell carcinoma affecting the free margin of the lower eyelid at the medial canthus, with reconstruction of the resulting defect, and we describe aspects of intraoperative care (Figure 1). Prior to the intervention, we applied 4% lidocaine eyedrops and a protective hydroxypropylmethylcellulose gel. After infiltration of the skin, tarsus, and conjunctiva with 2% mepivacaine, an eye guard was inserted as a mechanical protector and a 3/0 silk suture was placed in the mid zone of the tarsus for traction and to facilitate mobilization of the lower eyelid during the operation. A dilator was used to visualize the 2 lacrimal ducts and we then proceeded to the full-thickness surgical excision of the lesion, with a wide surgical margin that included the inferior lacrimal duct.2 The incision was performed with a no. 15 scalpel, dissection with Stevens scissors, and meticulous hemostasis was performed with bipolar electrocautery (the patient had a pacemaker).
The resulting defect affected more than a quarter and less than a third of the length of the eyelid, making it necessary to perform a tension-releasing incision horizontally from the lateral canthus toward the lateral margin of the orbit (canthotomy). The deep part of the orbicularis oculi muscle was divided, positioning the scissors along the bisector of the angle of the lateral canthus.3 This allowed tension-free transposition and final closure of the defect. The tarsus was sutured to the medial canthal tendon with a 6/0 absorbable suture and the skin with 5/0 silk, taking care to align the gray line and fixing the free ends of the suture with Steri-Strips to prevent them damaging the cornea. The canthotomy was then closed by suturing the skin to the superior tarsus with 5/0 silk. The superior lacrimal duct was dilated to prevent epiphora, and finally we administered dexamethasone and tobramycin eyedrops.
Histology confirmed the diagnosis of basal cell carcinoma and the borders were free of tumor. The cosmetic and functional results 5 days and a month after the intervention were very good (Figures 2 and 3).
IndicationsThis technique is suitable for patients with tumors that affect the free margin of the lower eyelid and whose surgical excision leaves a defect of between a quarter and a third of the length of the lower eyelid.
Advantages and DrawbacksCanthotomy allows defects of up to a third of the lower eyelid to be closed without tension.
The main drawback is that canthotomy is sometimes insufficient, and cantholysis must also be performed to release the lower eyelid from the orbital ring and achieve additional relaxation of the lower eyelid.
In our patient, although the defect was slightly less than a third of the lower eyelid, canthotomy was performed in order to avoid tension that could provoke symptoms. Furthermore, as it was necessary to fix the tarsus to the medial canthal ligament, we considered it advisable to reduce tension as much as possible. This is a simple technique that does not carry major risks for the patient and that preserves eyelid function.
ComplicationsThe palpebral reconstruction we present is very safe, and complications are rare. One issue to avoid is leaving a notch at the palpebral margin; this can be prevented by careful suturing. In our patient, as the tumor affected the entire medial canthus, we had to fix the tarsus to the medial canthal ligament using an absorbable suture. Excessive tension in the lateral segment of the eyelid can provoke lateral ectropion.
Regarding intraoperative care, we would like to draw attention to the importance of protecting the surface of the eye both with lubricant gels and with mechanical guards to avoid possible complications from ocular damage. Apart from the metallic guard we present in the video, corneal shields are used throughout surgery to avoid injury to the cornea; these are more comfortable for patients operated under local anesthesia.
Considerations Regarding the TechniqueFor the excision of lesions on the free border of the eyelid using the V technique, it is helpful to design a pentagonal V in the skin and a smaller V at the conjunctival border to facilitate closure of the defect.
ConclusionsWe have focused on the peculiarities of oncologic surgery of the eyelids. In addition to appropriate surgical excision and reconstruction, eyelid function must be preserved to avoid adverse effects that could damage the anterior pole of the eye and affect visual acuity. It is important to use the correct instruments for intraoperative care.4
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Xabier Belzunegui of the Communication and Design Unit of Navarra Biomed for recording and editing the video.
Please cite this article as: Iglesias-Zamora ME, Oscoz-Jaime S, Larumbe-Irurzun A, Bonaut-Iriarte B. Cuidados intraoperatorios en cirugía palpebral. Actas Dermosifiliogr. 2016;107:855–857.
The video received 2nd prize in the first “Best Video in Dermatologic Surgery” competition organized by the Spanish Academy of Dermatology and Venereology (AEDV), and was screened at the XXVIII Meeting of AEDV's Dermatologic Surgery, Cutaneous Oncology and Laser Therapy Group held in Valencia on 27 and 28 November, 2015.