Intralymphatic histiocytosis is a benign condition characterized by poorly defined erythematous plaques (sometimes forming a reticular pattern) as well as the presence of nodules and vesicles. Its etiology and pathogenesis appear to be related to chronic inflammation in the affected area, prior surgery, or systemic disease, particularly rheumatoid arthritis. We report on 2 new cases, both associated with joint surgery in the affected area and osteoarticular disease (primary synovial osteochondromatosis and rheumatoid arthritis). This is a chronic disease and there is no specific treatment. Different treatment options were chosen in the 2 cases described. A spectacular response to treatment with oral pentoxifylline and topical tacrolimus was observed in 1 of the patients.
La histiocitosis intralinfática es un proceso benigno caracterizado por placas eritematosas mal delimitadas, a veces reticuladas, otras con nódulos o vesículas en su interior. Su etiopatogenia parece estar relacionada con procesos inflamatorios crónicos en el área afectada, cirugía previa o con enfermedades sistémicas, sobre todo con la artritis reumatoide. Presentamos 2 nuevos casos, ambos asociados a cirugía articular del área afecta y enfermedad osteoarticular (osteocondromatosis sinovial primaria y artritis reumatoide). Esta entidad tiene un comportamiento crónico y no existe un tratamiento específico. En los 2 casos presentados se plantearon distintas opciones terapéuticas, mostrando uno de ellos una respuesta espectacular al tratamiento con pentoxifilina oral junto con tacrolimus tópico.
Intralymphatic histiocytosis is a rare entity that was first described by O’Grady et al1 in 1994. Some 54 cases have since been reported, most in association with rheumatoid arthritis and in patients with prosthetic joint replacements.2,3 Because the clinical presentation is nonspecific, diagnosis is fundamentally based on histologic findings. Immunohistochemistry demonstrates the presence of dilated lymphatic vessels (positive for D2-40, CD34, and CD31) in the reticular dermis and aggregates of (CD68-positive) intraluminal histiocytes.2 It has been hypothesized that this dilation of the lymphatic vessels is caused by an obstruction of lymphatic drainage arising from either a congenital abnormality or acquired damage in the vessels.2
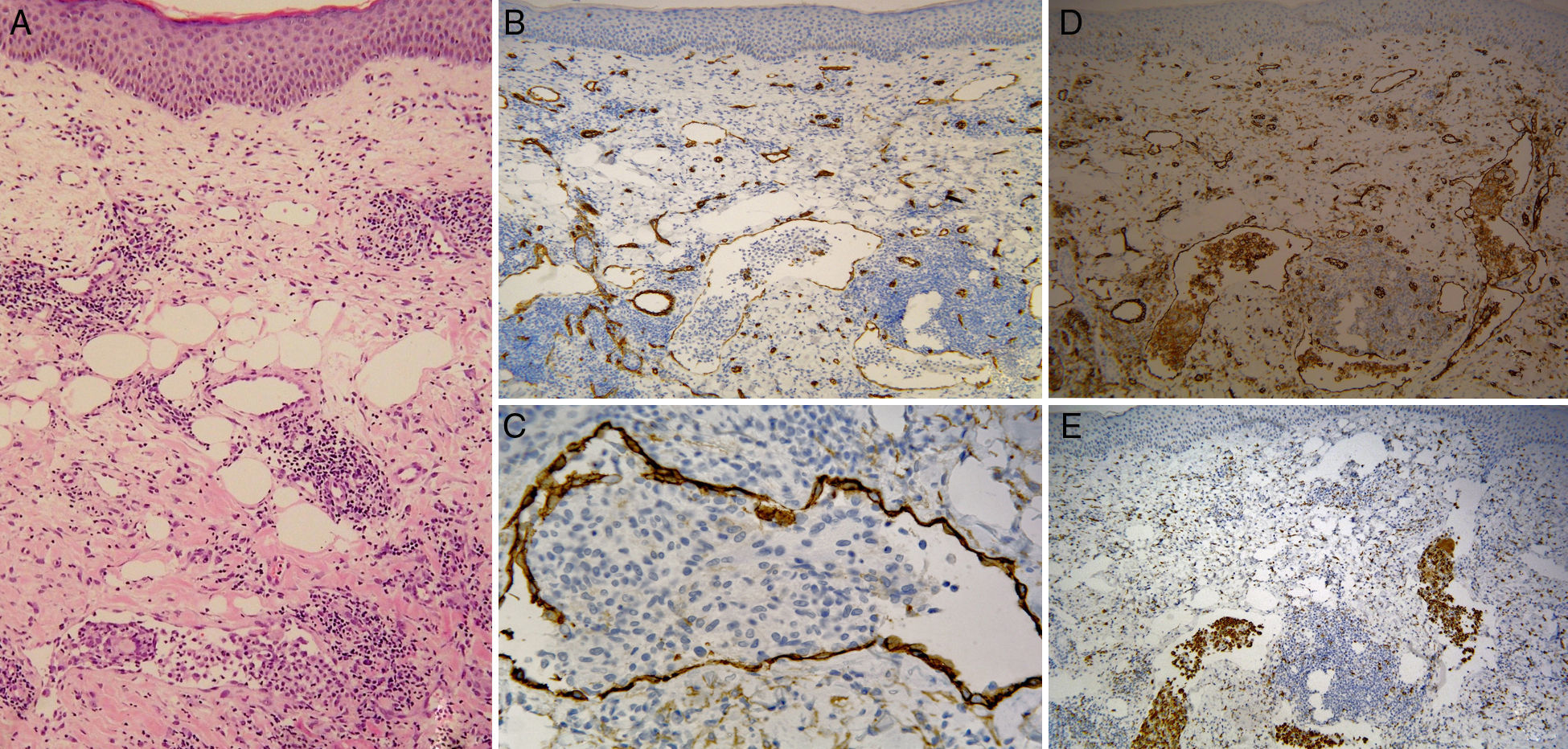
Case DescriptionsThe first patient was a 65-year-old woman who had undergone surgery to repair the rotator cuff of the left shoulder 1 year earlier. She had no history of rheumatoid arthritis or other diseases. The patient sought care for an erythematous and slightly pruritic patch on the left shoulder that had appeared 2 months earlier and had not responded to various regimens of oral antibiotics prescribed to treat the initial suspicion of cellulitis. Physical examination revealed an erythematous, edematous plaque with a livedoid appearance and poorly defined borders, covering the entire shoulder region and extending to the proximal third of the deltoids (Fig. 1). A 4-mm punch biopsy was diagnostic, showing dilated vessels in the reticular dermis that were positive for CD31, CD34, and D2-40 as well as CD68-positive intraluminal cell aggregates (Fig. 2). The results of a full blood workup were normal, including levels for complement, immunoglobulins, rheumatoid factor, and C-reactive protein. Magnetic resonance imaging showed signs of advanced joint degeneration and the possible existence of evolved primary synovial osteochondromatosis, although no malignancy has been demonstrated to date.
Skin biopsy. A, Panoramic view (hematoxylin-eosin, original magnification ×100) showing dilated vessels in the reticular dermis, some with empty lumens and others with mononuclear cell aggregates. B, Positive staining for CD34 (original magnification ×100). C, Positive staining for D2-40 (original magnification ×400). D, Positive staining for CD31 (original magnification ×100). E, Intraluminal cells positive for CD68.
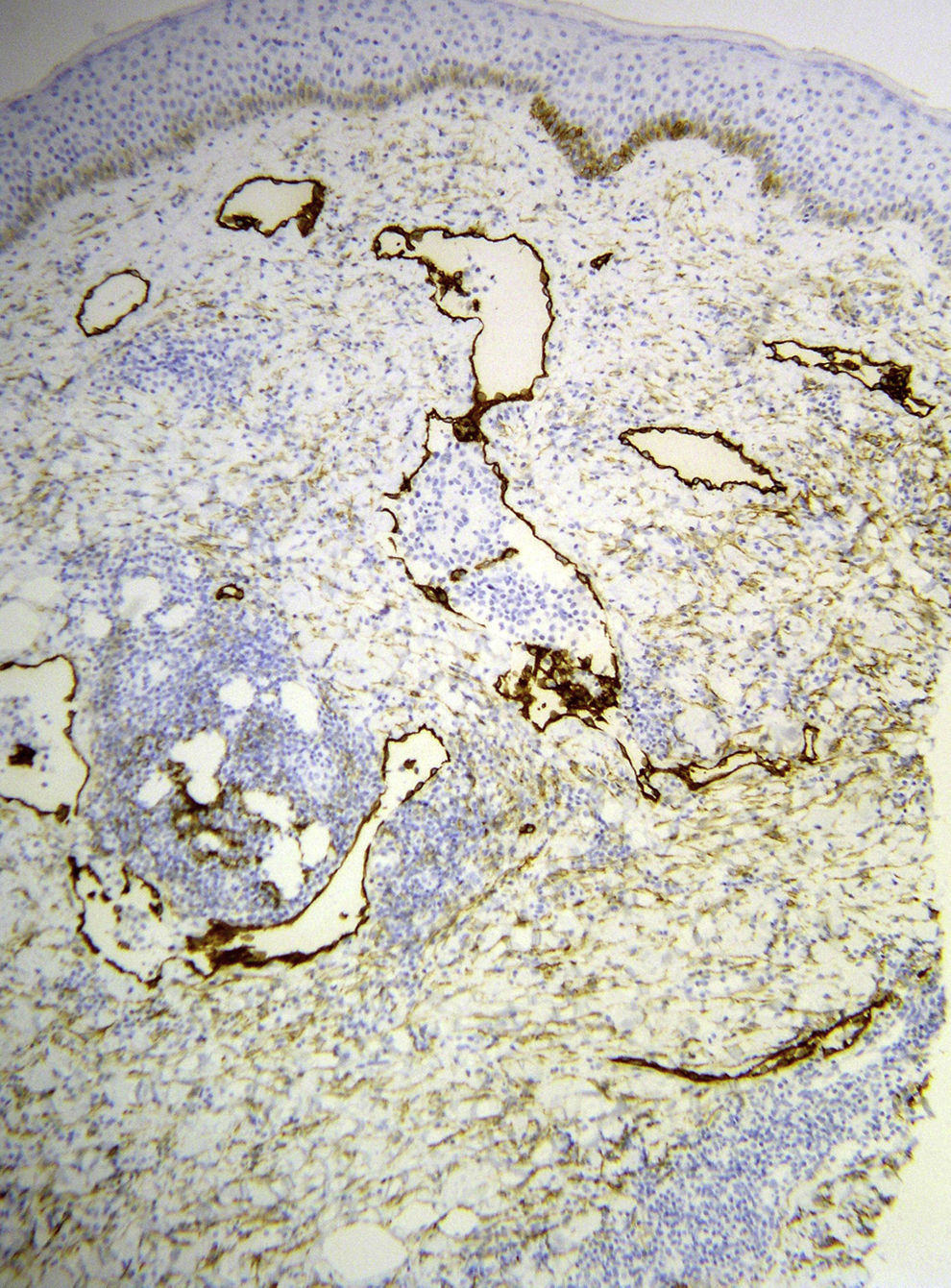
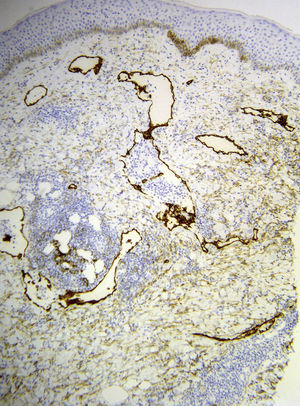
The second patient was a 77-year-old woman who had been diagnosed with rheumatoid arthritis 20 years earlier and was receiving treatment with nonsteroidal anti-inflammatory drugs. Two months after surgery on the left shoulder (repair of a partial biceps tendon rupture), she sought care for an asymptomatic patch that had gradually appeared in the weeks following the procedure (Fig. 3). During rehabilitation treatment, she was diagnosed with contact dermatitis, although no clear causative agent was identified. Topical corticosteroid treatment was prescribed, but no response was achieved. Physical examination revealed an erythematous, edematous plaque with imprecise borders on the anterior surface of the left shoulder, extending to the pectoral area. Skin biopsy, performed on the basis of clinical suspicion of intralymphatic histiocytosis, showed dilated vessels in the reticular dermis that were positive for CD31, CD34, and D2-40 (Fig. 4), CD68-positive cell aggregates inside lymphatic vessels of the reticular dermis, and perivascular lymphohistiocytic inflammatory cellularity, all confirming the diagnosis. Treatment was started with topical tacrolimus, applied once daily, and oral pentoxifylline (400mg/d), achieving an excellent response and practically complete resolution after 4 months of treatment (Fig. 5).
Intralymphatic histiocytosis is a rare entity that appears to be more frequent in older adults and in women.1–5 The most common site is the limbs, including the shoulder and hip areas.6 Intralymphatic histiocytosis has a nonspecific clinical presentation5 and tends to manifest as a single erythematous plaque and occasionally in the form of papules or nodules.3 Most of the fewer than 60 cases described in the literature3 are associated with rheumatoid arthritis,1–9 with skin alterations on the affected joints or, less frequently, in patients with prosthetic joint replacements.1,2,5–7,10 There have also been anecdotal reports of intralymphatic histiocytosis in association with surgical scars in patients with breast cancer1,5 and Merkel cell carcinoma,1,5 in the pectoral region of a patient with cancer of the colon,2,5 in the chest of a patient who underwent axillary lymphadenectomy to treat lymphatic tuberculosis,2 and in a patient with Crohn disease with involvement of the suprapubic region.2,5 Cases of primary intralymphatic histiocytosis, without association with any underlying disease, have also been reported.2
The etiology and pathogenesis of intralymphatic histiocytosis are not entirely understood, as the disease has been associated with pathologic processes of various kinds. Some authors classify it as a cutaneous reactive angiomatosis, a histopathologic pattern that arises in reaction to various inflammatory processes.1,3,7 The most widely accepted hypothesis is that the lymphatic vessels dilate in response to obstruction of lymphatic drainage caused by congenital abnormalities of the vessels, or by acquired damage from trauma, surgery, radiotherapy, or chronic inflammatory processes such as rheumatoid arthritis.1,7 Lymphostasis leads to poor antigen clearance, thus chronically stimulating the proliferation and aggregation of histiocytes.1,2,7 Chronic inflammation and the release of inflammatory mediators such as TNF and interleukin-6 perpetuate the process.3,8
The clinical differential diagnosis includes processes such as cellulitis, contact dermatitis, dermatomyositis, and neoplastic vascular processes.2 Definitive diagnosis is established by histology and immunohistochemistry and the main entity that must be ruled out is intravascular lymphoma.1,5
In both cases reported, surgery performed before the appearance of the skin lesions may have altered lymphatic circulation. A case of intralymphatic histiocytosis associated with severe osteoarthritis of the shoulder and rotator cuff arthropathy has also been reported.11 The magnetic resonance findings in our first patient were consistent with primary synovial osteochondromatosis, a rare entity characterized by the metaplastic formation of multiple cartilaginous nodules in the connective tissue of the synovial membrane of the joints, especially the knee and, less frequently, the hip, with the possibility of malignancy.12
In the management of intralymphatic histiocytosis, systemic diseases—especially rheumatoid arthritis,1–6 the underlying disease in 1 of our patients—must be ruled out. Skin lesions usually appear in the vicinity of affected joints, although the clinical course of the disease does not parallel the activity of rheumatoid arthritis.1,6
Although spontaneous involution is seen in some cases, with regression occurring after treatment of the associated disease6 or replacement of the prosthetic joint replacement in cases triggered by this surgery,1,2 most cases are chronic and indolent.1 There is no specific treatment for intralymphatic histiocytosis. Oral corticosteroids, topical corticosteroids, cyclophosphamide, radiotherapy, antiplatelet drugs such as salicylic acid plus amoxicillin–clavulanic acid, pentoxifylline,5 anti-TNF drugs such as infliximab8 and anti-interleukin-6 agents such as tocilizumab,9 topical tacrolimus,13 etc., have been used, always in isolated cases, usually with partial results and frequent recurrences.2,6 One of our patients responded satisfactorily to treatment with oral pentoxifylline and topical tacrolimus for 4 months, during which time the lesions resolved completely, and no recurrence was detected 6 months after suspension of treatment. Spontaneous involution cannot be ruled out but has not been common in the cases reported to date, which have generally been refractory to treatment. There have been 2 reports5,10 of cases with a positive response to pentoxifylline, due to the anti-inflammatory, antiplatelet, and TNF-inhibitory effects of this drug.10 We found only 1 case13 in which a good response was achieved with topical tacrolimus after 1 month of treatment, although the mechanism of action in this disease is not clear.
ConclusionsWe have reported 2 new cases of intralymphatic histiocytosis, highlighting the importance of histopathologic and immunohistochemical diagnosis of this rare entity. The first patient is the first case in which intralymphatic histiocytosis has been reported in association with primary synovial osteochondromatosis. Both patients had a history of joint surgery that could have caused lymphatic drainage alterations, triggering the onset of the disease. We would also like to highlight the response to combination therapy with oral pentoxifylline and topical tacrolimus, which is a good option for treating this chronic entity. Given the rarity of intralymphatic histiocytosis, it is difficult to carry out controlled studies to assess therapies and determine the role of isolated treatments in the clinical course of the lesions.
Ethical DisclosuresProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for the purpose of this study.
Data confidentialityThe authors declare that no private patient data appear in this article.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gómez-Sánchez ME, Azaña-Defez JM, Martínez-Martínez ML, López-Villaescusa MT. Histiocitosis intralinfática, a propósito de 2 casos. Actas Dermosifiliogr. 2018;109:e1–e5.