The incidence of melanoma has increased significantly in Spain in recent decades, and this tumor is now a public health problem.1 The role of the dermatologist is fundamental to the identification of high-risk patients and to the adoption of appropriate primary and secondary preventive measures for the early detection of skin cancer.1–3
Several well-standardized international clinical guidelines have been drawn up on the management of patients with melanoma,4–9 but no protocols exist on how to take an appropriate medical history and physical examination. The Australian guideline proposes an initial evaluation to determine the future risk of melanoma (grade B recommendation) looking at various factors, including age, sex, past history of melanoma or nonmelanoma skin cancer, family history of melanoma, number of melanocytic and atypical nevi, skin and hair color, skin phototype, and actinic damage.4
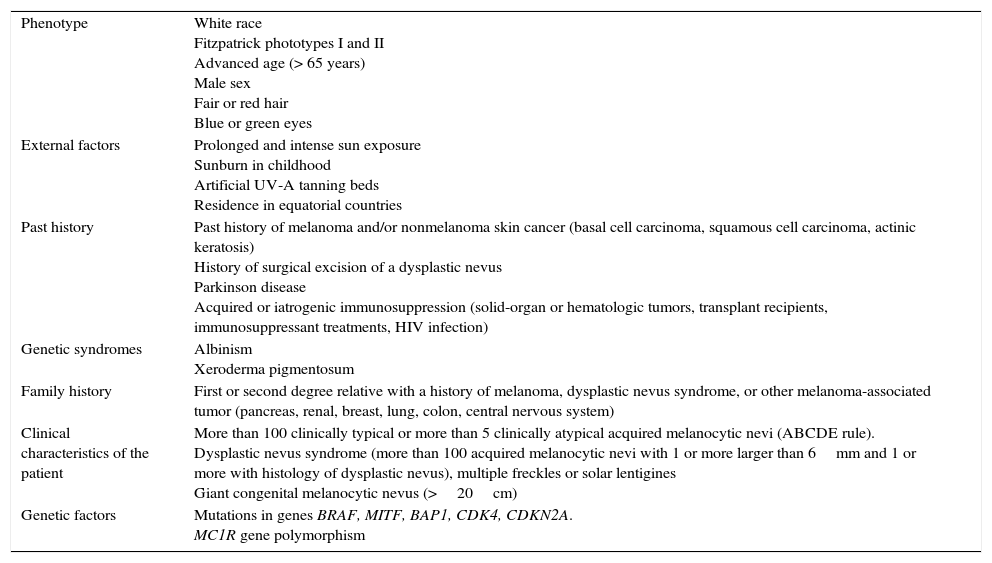
When a patient attends dermatology outpatients for an initial clinical evaluation of a nevus or suspected melanoma, an exhaustive medical history must be taken to detect the main risk factors (Table 1) and a complete physical examination performed.1–3 In the literature, we have found no descriptions of a protocol for the initial clinical evaluation of this type of patient. We therefore present our standard approach to the first consultation in the melanoma unit of Hospital Clínic in Barcelona:
- −
Personal history of drug allergy, drinking and smoking, current and previous occupations, known diseases, surgical history, noncutaneous tumors, and usual medical treatments.
- −
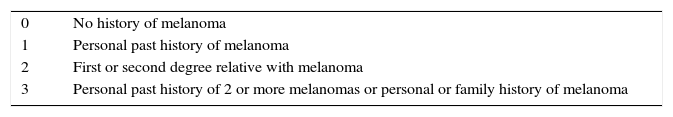
Past dermatologic history: known dermatoses, history of skin tumors, dysplastic nevus syndrome, treatments performed, previously excised nevi, and risk classification (Table 2).
- −
Family history of dysplastic nevus syndrome and of skin and other tumors.
- −
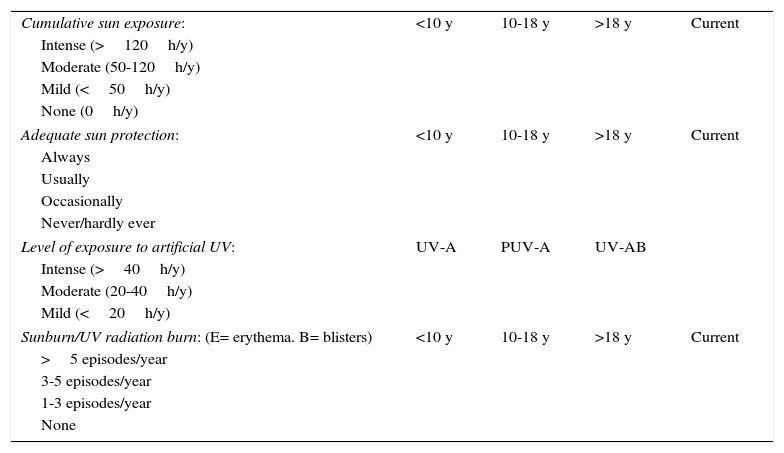
History of sun exposure, UV protection (Table 3), pattern of intermittent or chronic exposure, and time dedicated to outdoor occupational or leisure activities.
Table 3.Clinical Data to Be Considered in the History of Sun Exposure.
Cumulative sun exposure: <10 y 10-18 y >18 y Current Intense (>120h/y) Moderate (50-120h/y) Mild (<50h/y) None (0h/y) Adequate sun protection: <10 y 10-18 y >18 y Current Always Usually Occasionally Never/hardly ever Level of exposure to artificial UV: UV-A PUV-A UV-AB Intense (>40h/y) Moderate (20-40h/y) Mild (<20h/y) Sunburn/UV radiation burn: (E= erythema. B= blisters) <10 y 10-18 y >18 y Current >5 episodes/year 3-5 episodes/year 1-3 episodes/year None - −
Detailed history of the suspected melanoma lesion3,10: site, time since onset, presence of a precursor lesion, symptom or sign that prompted consultation, pruritus, pain, bleeding, erosion, ulceration, suppuration, changes in color (multiple shades of dark brown or black, or appearance of various colors, including light brown, dark brown, black, red, blue, gray, and white), changes in morphology (appearance of irregular margins), change in size (rapid or continuous growth), elevation of the lesion, changes in the surrounding skin (erythema, edema, satellite pigmentation), changes in consistency (softening, friability), and previous treatment of the lesion.
- −
Systems review: constitutional, neurologic, otorhinolaryngologic, respiratory, musculoskeletal, hepatic, gastrointestinal, cutaneous, subcutaneous, and lymphatic signs and symptoms.
Main Risk Factors for Melanoma.
| Phenotype | White race Fitzpatrick phototypes I and II Advanced age (> 65 years) Male sex Fair or red hair Blue or green eyes |
| External factors | Prolonged and intense sun exposure Sunburn in childhood Artificial UV-A tanning beds Residence in equatorial countries |
| Past history | Past history of melanoma and/or nonmelanoma skin cancer (basal cell carcinoma, squamous cell carcinoma, actinic keratosis) History of surgical excision of a dysplastic nevus Parkinson disease Acquired or iatrogenic immunosuppression (solid-organ or hematologic tumors, transplant recipients, immunosuppressant treatments, HIV infection) |
| Genetic syndromes | Albinism Xeroderma pigmentosum |
| Family history | First or second degree relative with a history of melanoma, dysplastic nevus syndrome, or other melanoma-associated tumor (pancreas, renal, breast, lung, colon, central nervous system) |
| Clinical characteristics of the patient | More than 100 clinically typical or more than 5 clinically atypical acquired melanocytic nevi (ABCDE rule). Dysplastic nevus syndrome (more than 100 acquired melanocytic nevi with 1 or more larger than 6mm and 1 or more with histology of dysplastic nevus), multiple freckles or solar lentigines Giant congenital melanocytic nevus (>20cm) |
| Genetic factors | Mutations in genes BRAF, MITF, BAP1, CDK4, CDKN2A. MC1R gene polymorphism |
We also present our standard procedure for complete physical examination:
- –
Skin phototype (I-VI),2,3 race (white, black, yellow), eye color (green, blue, gray, brown, black), hair color at 18 years of age (red, fair, brown, black).
- –
Complete dermatologic examination, including scalp, intertriginous areas, oral, ocular, genital, and anal mucosas, palms, soles, and nails.
- –
Presence of freckles, solar elastosis, solar lentigines in sun-exposed areas, actinic keratoses, basal cell carcinoma, and squamous cell carcinoma.
- –
Estimation of the total number of acquired melanocytic nevi, whatever their size (<50, 50-100, 100-200, >200). Evaluation of the number of these lesions and of the clinical type (junctional, compound, intradermal) and size (small, 2-6mm; intermediate, 6-15mm; or large,>15mm) on the trunk and on the upper limbs. Evaluation of the number of clinically atypical nevi and presence of congenital nevi.
- –
Description of the suspected lesion: site, diameter, palpation, presence of papules or nodules, size, pigmentation, clinical type, ulceration, areas of regression, adjacent nevi. Physical examination of the regional lymph nodes, presence of hepatomegaly, splenomegaly, and locoregional and/or distant subcutaneous masses or nodules.
- –
Dermoscopic features.
- –
Photographs of the lesions prior to the surgical excision of suspicious skin lesions (essential).
In conclusion, the objective of this article has been to present the guideline used in our center for the initial clinical evaluation of nevi or suspected melanoma in the hope that it will help dermatologists evaluating patients with such lesions. Finally, it is essential that we undertake patient education regarding periodic self-examination, the clinical characteristics of melanoma (ABCDE rule and ugly duckling sign), and appropriate measures of photoprotection.1–3,10
Please cite this article as: Imbernón-Moya A, Podlipnik S, Malvehy J, Puig S. Valoración inicial del paciente con lesiones cutáneas pigmentadas. Actas Dermosifiliogr. 2016;107:616–618.