Merkel cell carcinoma is a malignant skin tumor with a poor prognosis that primarily affects photoexposed areas of elderly patients. Tumor size is a very strong prognostic factor, with much better outcomes associated with small lesions, measuring less than 1cm. However, such lesions are rarely seen in the clinic in view of the rapid growth of this tumor.
We report 2 cases of incipient Merkel cell carcinoma. Both cases of incipient Merkel cell carcinoma measured approximately 5mm in diameter. One tumor was confined to the epidermis and papillary dermis on the nose of a 79-year-old man and the other was located in the deep dermis, almost in the hypodermis, on the buttock of an 82-year-old woman. In both cases, the lesions had appeared weeks earlier. The first tumor seemed to originate in the dermoepidermal junction whereas the second originated almost in the hypodermis. Although the lesions were at a similar disease stage and had a similar size, their different locations within the dermis highlight once again the controversy about which cells give rise to Merkel cell carcinoma. The precursor cells could feasibly be Merkel cells in the first case but not in the second.
El tumor de Merkel es una neoplasia cutánea de mal pronóstico que afecta preferentemente a pacientes ancianos en áreas fotoexpuestas. El tamaño tumoral es un factor pronóstico muy importante en este tumor, de modo que las lesiones pequeñas, menores de un centímetro, tienen un comportamiento mucho mejor que el resto. Sin embargo, el crecimiento rápido de este tumor hace difícil encontrar casos de pequeño tamaño.
Describimos dos pacientes con sendos tumores de Merkel incipientes, de aproximadamente 5 milímetros cada uno, uno de ellos en la nariz de un varón de 79 años confinado a la epidermis y dermis papilar, y el otro en la nalga de una mujer de 82 años, localizado en la dermis profunda, casi en la hipodermis. En ambos casos se trataba de lesiones de semanas de evolución, y sin embargo el primer tumor parecía proceder de la unión dermoepidérmica, mientras que el segundo se iniciaba casi en la hipodermis. Estos dos casos son similares en cuanto a tiempo de evolución y tamaño, pero opuestos en lo que respecta a su localización dentro de la dermis, por lo que ponen de manifiesto una vez más lo controvertido de la célula de origen del tumor de Merkel, que se hipotetiza que sea la célula de Merkel, y que sería factible en el primer caso, pero no en el segundo.
Merkel cell carcinoma is a rare malignant neuroendocrine tumor with a poor prognosis. It primarily affects photoexposed areas of skin in elderly patients. Incidence is higher in immunodeficient patients and a probable etiologic role has recently been attributed to polyomavirus infection.1,2
Tumor size is an essential prognostic factor in Merkel cell carcinoma and early diagnosis and early surgical resection are therefore very important. The rapid rate at which these tumors normally grow means that they are rarely removed at a size of less than 1 centimeter. Published cases of intraepidermal Merkel cell carcinoma are even more rare, and most of them are diagnosed coincidentally on removal of another epidermoid or basal-cell carcinoma.3,4 We report 2 cases of incipient Merkel cell carcinoma not associated with another lesion; both tumors had a diameter of less than 5mm. We discuss the most appropriate treatment in these cases of small Merkel cell carcinoma and highlight the distinctive histologic aspect and unusual location—the dermoepidermal junction in one case and the junction between the dermis and the subcutaneous tissue in the other case.
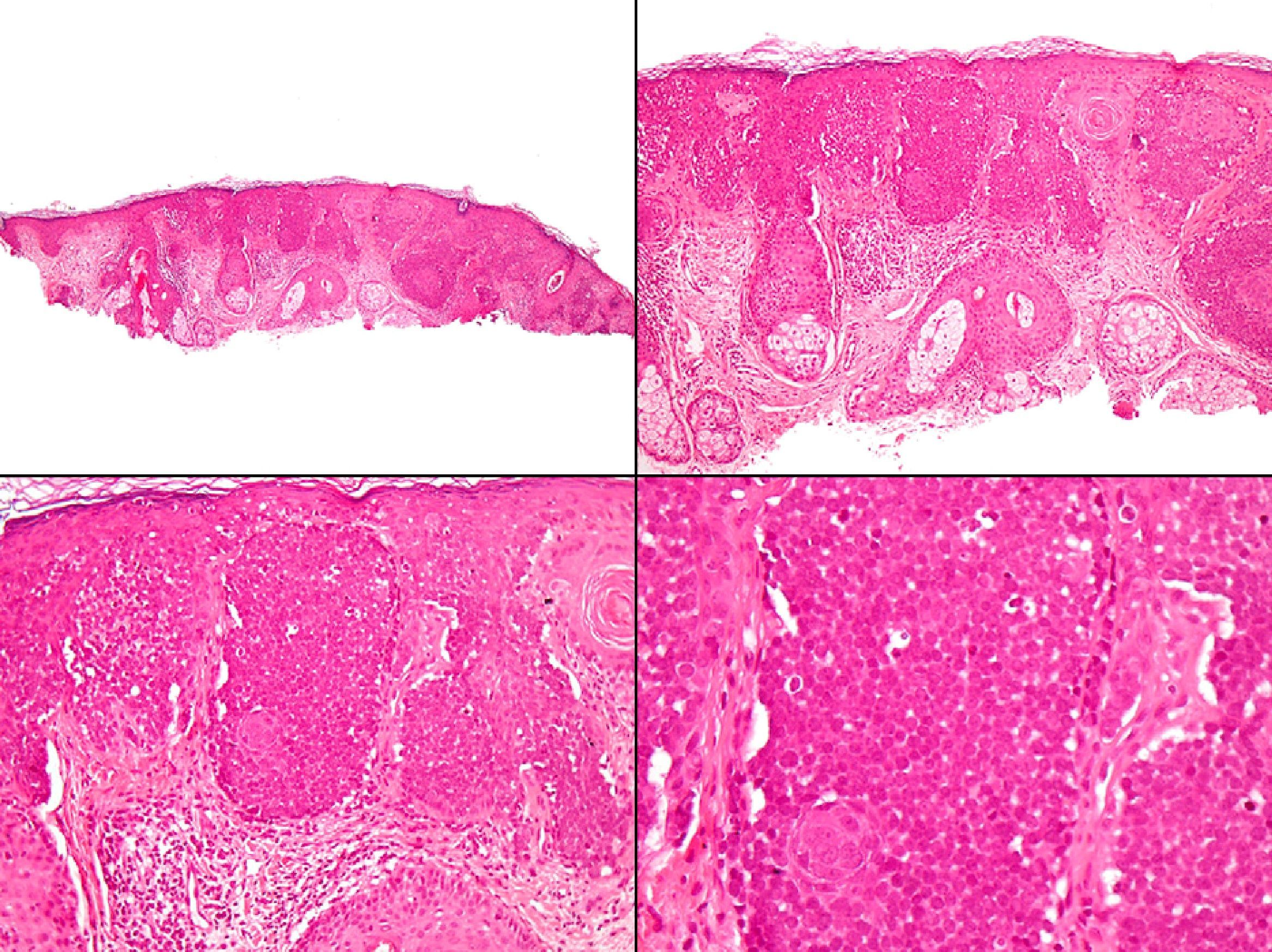
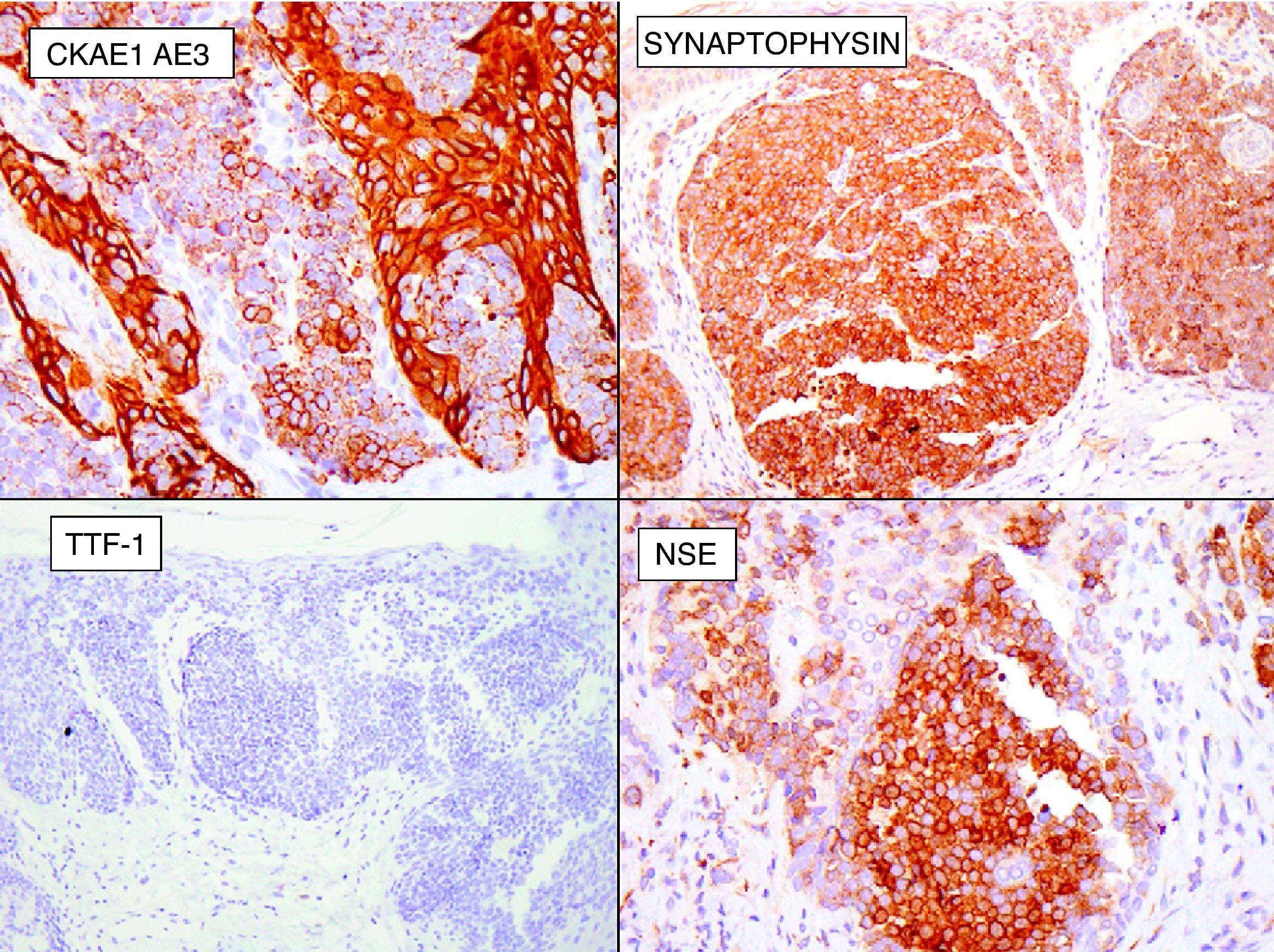
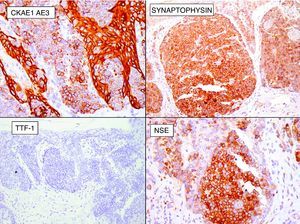
Case 1The first case was a 79-year-old English patient with a history of gastric ulcer and occupational exposure to asbestos. The patient was being followed up in our department because of a basal cell carcinoma located on the tip of the nose; the tumor had been treated 2 years earlier with Mohs surgery and the site was reconstructed with a graft. A routine review detected a lesion that had gone unnoticed by the patient, an erythematous papule with a diameter of approximately 2mm, located on the right nostril. Owing to a clinical suspicion of basal cell carcinoma a shave biopsy of the lesion was performed. Pathology identified a tumor located in the dermoepidermal junction and papillary dermis; the tumor consisted of clusters of monomorphic round basophilic cells with large vesicular nuclei, no visible nucleoli, and scattered signs of mitosis (Fig. 1). Immunohistochemistry showed the cells to be positive for pancytokeratin, chromogranin A, synaptophysin, and neuron-specific enolase, and negative for cytokeratin 20, thyroid transcription factor 1 (TTF-1), and S-100 protein (Fig. 2).
Once the tumor had been diagnosed as Merkel cell carcinoma, treatment was completed using Mohs surgery to ensure complete excision of the malignant lesion; the margin was negative after a single stage. The staging study, which included computed tomography (CT) of the chest, abdomen, and pelvis, was negative for tumors; the CT scan incidentally revealed calcified pleural plaques characteristic of asbestosis. The patient was free of disease after 10 months of follow-up.
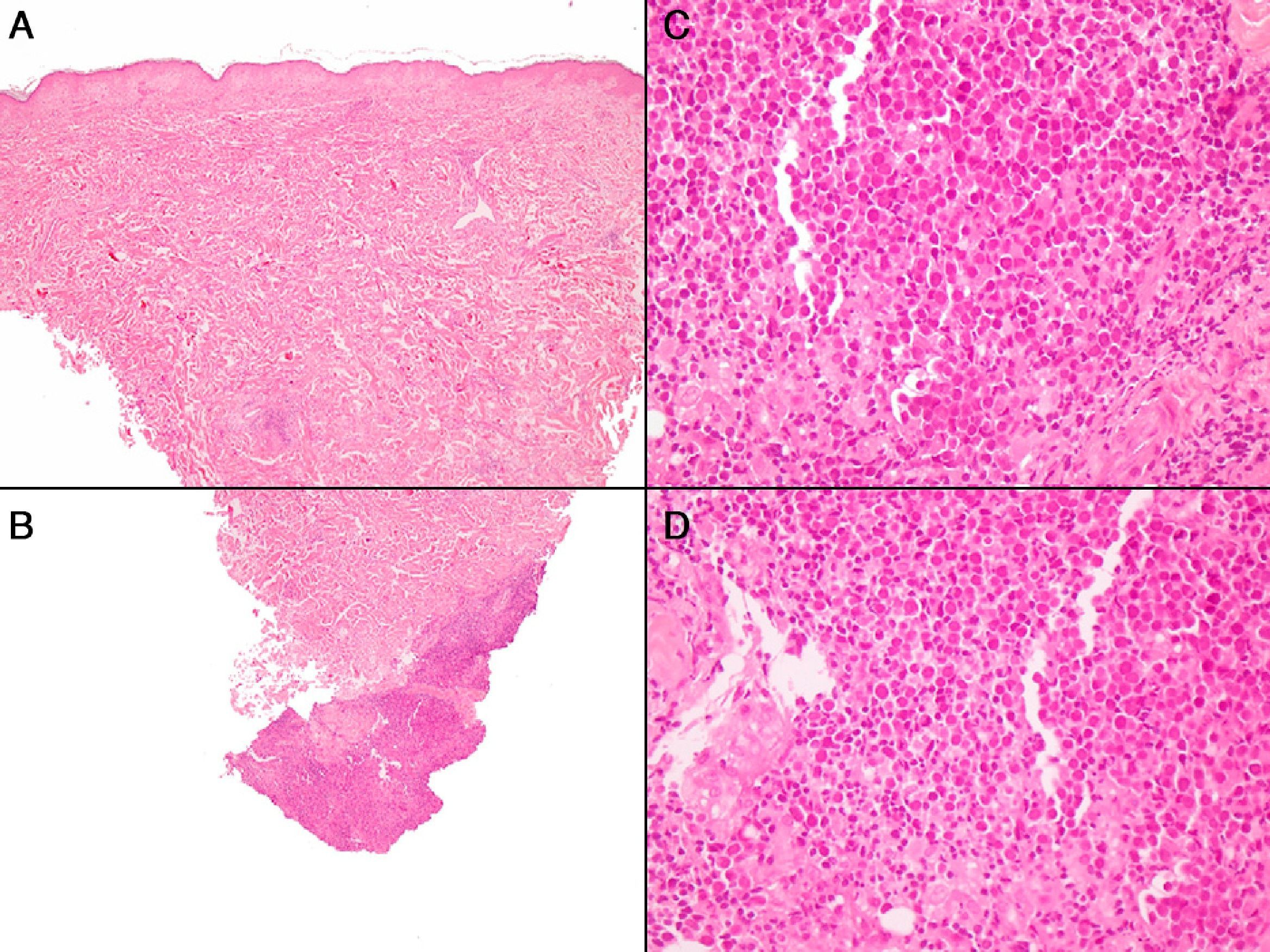
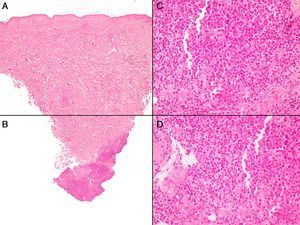
Case 2The second patient was an 82-year-old woman with no relevant history, who visited our department with a lesion that had appeared 2 weeks earlier on the left buttock. Examination revealed a very small subcutaneous nodular lesion measuring less than a centimeter; the lesion was completely nonspecific, covered by normal skin, and palpable but not visible. A punch biopsy showed a proliferation of monomorphic round cells with large vesicular nuclei, no nucleoli, and abundant mitosis in the deep dermis, almost reaching the hypodermis (Fig. 3). This proliferation of cells was accompanied by an infiltrate of nontumorous lymphocytes. Immune staining was positive for cytokeratin 20 and chromogranin A, and negative for TTF-1.
A and B, Panoramic image of the second case, with perivascular lymphocytic inflammatory infiltrates; the infiltrates are light in the superficial and middle dermis, and dense in the deep dermis. C and D, Detail of the infiltrate in the deep dermis, showing round cells with large nuclei with loose chromatin, and abundant mitosis accompanied by normal lymphocytes (hematoxylin-eosin, original magnification: A and B, x40; C and D, x400).
In this case, the staging study included a CT scan of the chest, abdomen, and pelvis, and positron emission tomography (PET); the results of all tests were negative. Treatment was completed by extending the margin of excision by 2cm in diameter and down to the fascia and studying the sentinel node. Both the extended margin and the sentinel node were negative for tumors. The patient was still free of disease after a year and a half of follow-up.
DiscussionManagement of patients with Merkel cell carcinoma is often complex. The aggressive nature of the tumor and its low frequency make it difficult to establish a reliable and uniformly accepted management protocol.5 In general, the most appropriate treatment is considered to be surgery plus radiation therapy of the surgical site,6 accompanied, when applicable, by a study of the sentinel nodes or selective lymph node resection, sometimes with radiation therapy of the lymph node drainage area.7 However, the wide surgical excision recommended in the literature is not always possible, and no specific recommendations exist regarding ideal surgical margins. Mohs surgery is increasingly recommended for the treatment of Merkel cell carcinoma, but this modality is not available in many hospitals.8 As the tumor is known to be sensitive to radiation, the use of adjuvant radiation therapy after surgery would seem to be logical. However, in practice, we should always be reticent about treating a very small tumor on the face of a patient (as in our first case) with aggressive initial surgery plus radiation therapy. A study by Stokes et al.9 reviewed 346 cases of Merkel cell carcinoma, with known lymph node staging (either because the tumor had a sentinel node or because selective lymph node resection had been performed) in 213 cases. Those authors correlated lymph node staging with the size of the primary Merkel cell tumor and found that tumors measuring less than 1 centimeter were found in only 2 patients (4%) with lymph node involvement. Furthermore, lymph node involvement in those 2 patients was not detected by means of the sentinel node, as the enlarged nodes in these patients were clinically palpable. The authors therefore concluded that the sentinel node technique is probably not justified in Merkel cell tumors with a diameter of less than 1 centimeter. In our 2 cases, the therapeutic decision was made prior to the publication of that study. The notably small size of both tumors led us to discuss the most appropriate treatment in a tumor committee. We decided to perform a sentinel node study in the second patient but not in the first patient, and treated the tumors somewhat similarly to the way we manage cases of melanoma, that is, based on a pseudo-Breslow assessment of the tumors. Thus, the first case showed a Breslow depth of less than 1mm, whereas the second tumor, which was almost in the hypodermis, had a considerably greater Breslow depth.
The other reason we report these 2 cases is that the histologic appearance of the tumors led us to think about another aspect of Merkel cell carcinoma that is the subject of debate: its phylogeny. It has traditionally been accepted that this carcinoma originates in the Merkel cells, based on the similarities in immunohistochemistry and ultrastructure. However, this has never been conclusively proved the hypothesis currently gaining support is that the origin of these tumors is in pluripotent cells. In our first case, the tumor does appear to originate in the dermoepidermal junction and the origin could therefore be in the Merkel cells, which are found in the basement layer of the epidermis and sometimes in the hair follicles. In the second case, however, the tumor was found in the subcutaneous tissue and had no contact with adnexal epithelia, which makes the possibility that it originated in Merkel cells remote.
In our first case, the absence of cytokeratin 20 in the tumor as shown by immunohistochemistry, is also a rare finding in Merkel carcinoma. Approximately 90% of cases of Merkel cell carcinomas are positive for cytokeratin 20, although a negative result for this marker in no way rules out a diagnosis of Merkel cell carcinoma. In fact, in the differential diagnosis between Merkel cell carcinoma and skin metastasis of a neuroendocrine tumor, negative staining for TTF-1 is considered to be more specific to Merkel cell carcinoma than a positive result for cytokeratin 20 because only 3% of systemic neuroendocrine tumors are negative for TTF-1 but Merkel cell carcinoma is practically never positive for this marker.
In summary, we report 2 cases of very early Merkel cell carcinoma that, owing to the small size of the lesions, probably requires less aggressive treatment than most of these tumors.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Requena C, et al. «Baby Merkel»: tumor de Merkel incipiente; a propósito de 2 casos. Actas Dermosifiliogr.2013; 104:71-4.