Idiopathic facial aseptic granuloma (IFAG) is a benign condition that affects children. It was first described in 1999 and named pyodermite froide du visage, due to its similarity with an abscess with few inflammatory signs.1 Subsequently, in 2001, Roul et al.2 gave it its current name. It is characterized by the appearance of 1 or several asymptomatic erythematous-violaceous nodules that arise in the cheeks, with no predisposing factors.3 We present a case of IFAG, paying particular attention to the ultrasound findings that, associated with compatible clinical manifestations, allow us to reach a correct diagnosis without resorting to unnecessary procedures.
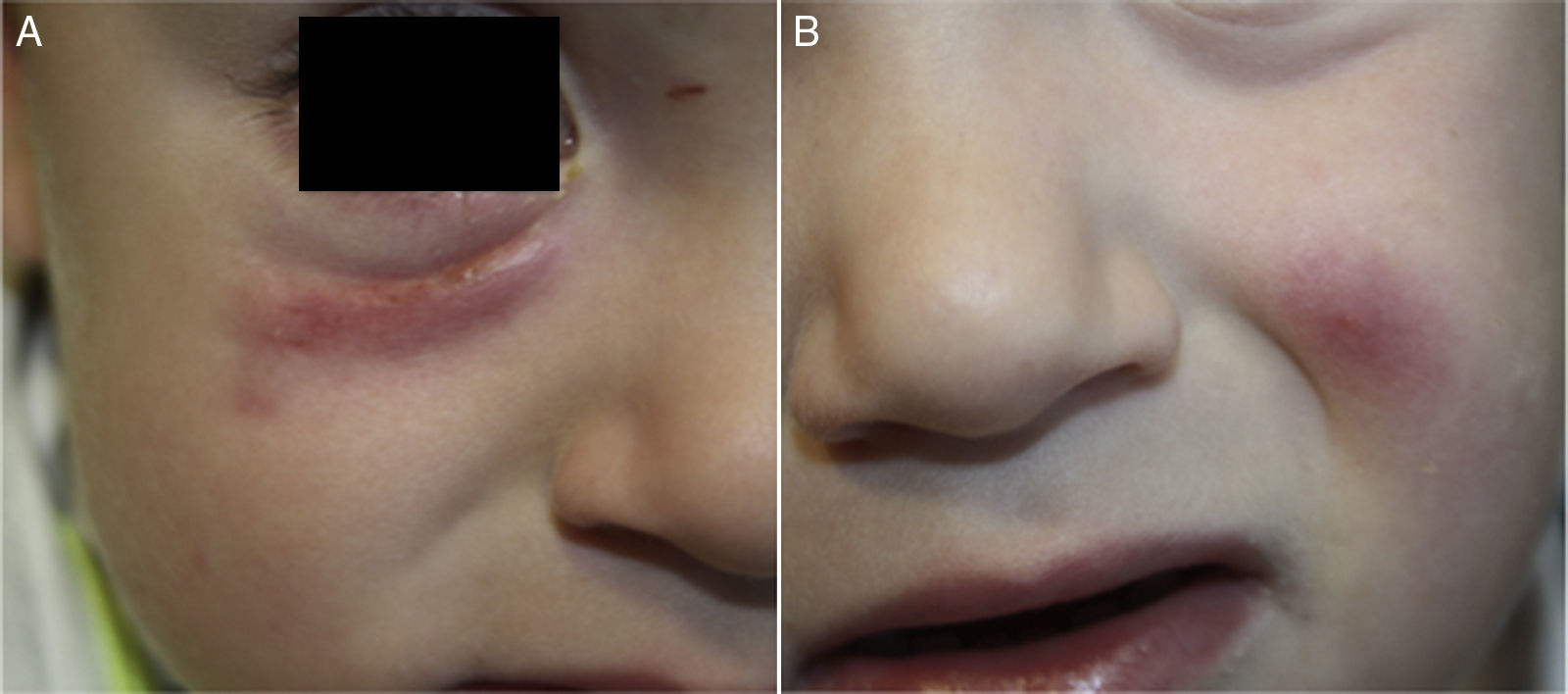
The patient was a healthy, 2-year-old boy who was seen for 2 asymptomatic facial lesions that had arisen 4 months earlier. Physical examination revealed 2 relatively firm, painless erythematous-violaceous nodules in the left cheek and right lower eyelid, measuring respectively 1cm and 3cm in diameter (Fig. 1). The nodules did not fluctuate. There were no palpable locoregional lymph nodes.
The parents did not report bleeding, ulceration or drainage of purulent fluid, and there was no history of insect bite or trauma. At another center, cultures performed for bacteria, fungi, and mycobacteria were negative, and treatment with oral erythromycin and topical metronidazole had been precribed.
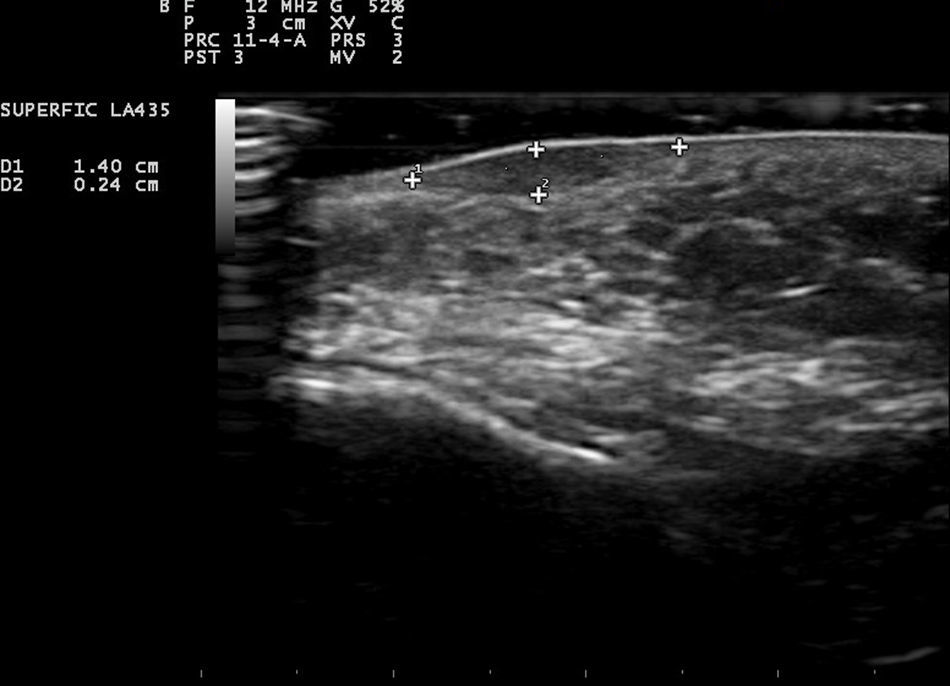
Skin ultrasound (18MHz transducer) of the nodule in the left cheek revealed a well-defined, hypoechoic dermal lesion measuring 1.37×0.24cm, with no posterior enhancement. No Doppler signal was observed and the lesion did not contain calcium deposits (Fig. 2).
A diagnosis of IFAG was made based on the medical history, physical examination, and ultrasound findings. The lesions presented a progressive improvement (Fig. 3) and resolved spontaneously after 8 months.
IFAG is more common in girls, and the mean age at presentation is 42.3 months.4 In 90% of cases the lesions are single and arise in the triangle between the labial commissure, the earlobe, and the medial canthus of the eye.3
The etiology and pathogenesis of IFAG are unknown. It has been associated with insect bites and trauma, but no relationship with immunodeficiency or serious diseases has been demonstrated. No triggering infection has been detected, as microbiology cultures have been negative and there has been no response to antibiotic treatment. An embryogenic theory has been proposed, in which IFAG is the result of a granulomatous reaction to an embryologic remnant derived from cell migration.3,4
Because of the site of IFAGs, their association with recurrent chalazion, and the good response, in some cases, to treatments used in rosacea, some authors have suggested the hypothesis that IFAGs form part of the spectrum of childhood rosacea.3,5 However, the spontaneous resolution of IFAGs without the need for treatment—something not observed in granulomatous rosacea—would argue against such a hypothesis. Prey et al.6 reported that children with IFAG have a higher risk of developing childhood rosacea, particularly the ocular form, and they proposed annual ophthalmologic evaluation to facilitate early diagnosis.
Cultures are systematically negative, except in the event of superinfection, which should be suspected if sudden and rapid growth of the lesion is observed.3,4 Histologically, lesions are characterized by a chronic granulomatous reaction in the superficial and deep dermis, similar to that observed in foreign body or mycobacterial granulomas.3,4
Skin ultrasound can be a useful tool to confirm a diagnosis of IFAG. The typical ultrasound pattern is one of a clearly defined, solid, hypoechoic dermal lesion with no calcium deposits.1 A hyperechoic lesion with a hypoechoic center has only been observed in 2 lesions, 1 of which showed posterior enhancement.5,7 Doppler study was negative except in 2 cases.7,8 In our patient, the absence of a Doppler signal may have been related to the fact that ultrasound examination was performed during an advanced phase of the lesion, as Doppler findings in IFAG may depend on the stage of the lesion when the study is performed.
The following conditions should be included in the sonographic differential diagnosis: epidermal cyst, a round anechoic lesion with posterior enhancement and a lateral acoustic shadow; pilomatrixoma, a round dermal lesion with variable central ecogenicity due to the presence of hyperechoic areas corresponding to calcifications, surrounded by a hypoechoic halo; pyogenic granuloma, a poorly defined, oval hypoechoic lesion, with a peripheral nutrient vessel and intense doppler flow internally; infantile hemangioma, a well-defined, homogeneous hypoechoic solid lesion with abundant blood vessels; and abscesses, well-defined hypoechoic or anechoic lesions with intense Doppler flow and anechoic linear fistulous tracts that communicate with the epidermis.9
The clinical differential diagnosis is also broad: other benign tumors, such as dermoid cyst, juvenile xanthogranuloma, and Spitz nevus, bacterial, fungal, protozoal, or mycobacterial infections; insect bites; arteriovenous malformations; and paucisymptomatic nodulocystic childhood acne.3,10
The lesions tend to resolve spontaneously after a mean period of 11 months and do not leave a scar.3 In general, antibiotic therapy is ineffective, although some cases have shown a good response to oral macrolides or topical metronidazole.7
We must include IFAG in the differential diagnosis of acquired facial nodules in children. The medical history and the clinical, microbiologic, and ultrasound findings enable us to make an early diagnosis and to avoid unnecessary aggressive procedures.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Vázquez-Osorio I, Álvarez-Cuesta CC, Rodríguez-González L, Rodríguez-Díaz E. Granuloma aséptico facial idiopático. Utilidad de la ecografía cutánea. Actas Dermosifiliogr. 2017;108:266–268.