Imiquimod 5% is a drug approved by the US Food and Drug Administration (FDA) for the topical treatment of genital warts, actinic keratosis, and basal cell carcinoma (BCC). While this drug is commonly used in daily clinical practice, no reports to date have associated its administration with alterations in scar formation.
We describe 2 cases of abnormal scar formation after treatment with imiquimod 5% cream.
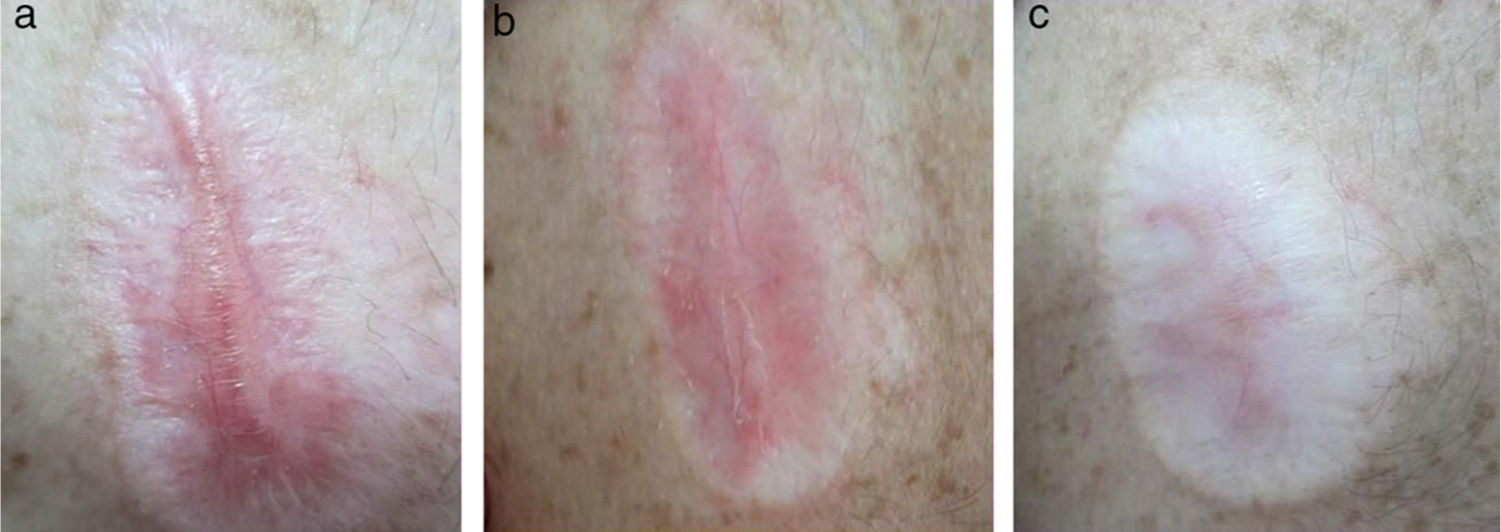
Patient 1The patient was a 32-year-old man with no drug allergies and no relevant past medical or surgical history. He presented with a lesion in the right pectoral region that had developed 2 years previously and had been treated with antifungals for a suspected fungal infection. Examination revealed an erythematous desquamative plaque of 2cm in diameter consistent with Bowen disease. The patient was treated with imiquimod 5% cream once daily, Monday through Friday, for 6 weeks. Sixty days after starting treatment the patient developed in the treated area a raised, pearly, linear lesion with superficial telangiectasias, surrounded by a halo of atrophic and hypopigmented skin (Fig. 1A). Based on these findings it was decided to perform a skin biopsy of the lesion for histopathological analysis. This revealed a focally granulomatous, nonspecific, chronic inflammatory process, with fibrotic scarring and the absence of malignant neoplastic elements, ruling out a tumoral process and leading to a diagnosis of hypertrophic scarring.
Treatment with topical corticosteroids and silicone gel sheets resulted in flattening of the lesion and a reduction in both pruritus and telangiectasias, but hypochromia and atrophy persisted 9 months after treatment (Figs. 1B and 3C).
Patient 2The patient was a 71-year-old woman with no known drug allergies and a medical history of dyslipidemia, osteoarthritis, and pollinosis. She had no past surgical history. She presented with a pearly lesion of 1cm in diameter in the left pectoral region that had developed 2 years previously. Dermoscopy revealed central keratosis and thick telangiectasias (Fig. 2A). A diagnosis of superficial BCC was established and treatment was initiated with imiquimod 5% cream once daily, Monday through Friday, for 6 weeks.
Two months later the patient developed an erythematous, indurated, and slightly painful plaque containing 3 branched linear elements of elastic consistency. The plaque was 7cm in diameter, extending beyond the area of the initial tumor. A clinical diagnosis of keloid after application of imiquimod 5% cream was established (Fig. 2B).
Treatment with topical corticosteroids for 2 months resulted only in a reduction in erythema (Fig. 2C).
Imiquimod 5% cream is indicated for genital warts, superficial BCC, and actinic keratosis.1 However, its off-label use in numerous dermatologic conditions has produced favorable results.2,3
The most common local secondary effects are erythema, pruritus, burning, ulceration, erosion, crusting, and flaking, and the most commonly described systemic symptoms are headache, fatigue, fever, malaise, pains, nausea, diarrhea, and joint pain.4,5
Imiquimod has been proposed as an alternative treatment in areas in which surgery is technically difficult, specifically because of the better aesthetic results obtained. It has even been proposed for the treatment of hypertrophic scars and keloids.6,7 However, it is important to be aware that inflammation is often associated with imiquimod administration. This inflammatory reaction, which varies in intensity and nature, can even cause hypertrophic scars or keloids in anatomic areas that are prone to scarring (pectoral region, sternum, clavicle, etc.)
In the cases described here the lesions were located on the anterior surface of the chest. This area is prone to hypertrophic scarring and keloids, which should be borne in mind when prescribing imiquimod in these locations.
As neither of the patients had any relevant history of surgery or trauma, it was impossible to ascertain their predisposition to impaired scar formation. However, both patients developed severe inflammation in keloid-prone areas, which may account for the observed clinical course.
Please cite this article as: Márquez García A, Ojeda Vila T, Ferrándiz L, Ríos Martín JJ. Cicatriz hipértrofica y queloide después de la aplicación de imiquimod 5% crema. A propósito de 2 casos. Actas Dermosifiliogr. 2014;105:795–797.