The patient was a black male, 38 years old, who was seen for a lesion that had been developing for 15 days on the external aspect of the ankle of the left foot. The lesion was painful and made walking difficult. Of interest, the patient lives in Kenya, in an area of extreme poverty where going barefoot is common.
Physical ExaminationPhysical examination showed a hyperpigmented plaque, 4×4 cm, with poorly defined borders. The plaque consisted of several confluent papules, each of which had a dark brown spot at its centre, surrounded by a white halo with a hyperkeratotic surface (Fig. 1).
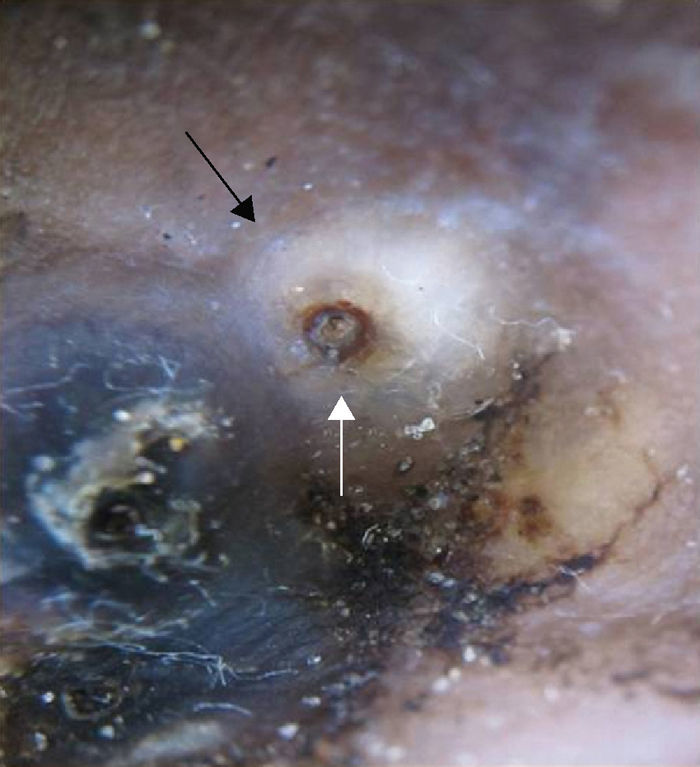
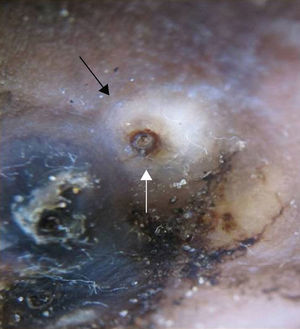
Additional TestsDermoscopy (Fig. 2) showed that this spot was in fact a brown pigmented ring around a central pore (white arrow), surrounded by a whitish area bounded by a faint pigmented peripheral ring (black arrow).
What Is Your Diagnosis?
DiagnosisThe clinical and dermoscopic characteristics of the lesion allowed us to establish a diagnosis of tungiasis. Once extracted, the dermoscopic image of the flea showed the presence of eggs in the abdominal cavity, as well as the posterior opening of the exoskeleton (Fig. 3).
Clinical CourseSurgery was used to completely extract the parasites, which were 5 in number. Antibiotic prophylaxis and a tetanus booster dose were administered. The patient's subsequent clinical course was satisfactory.
CommentTungiasis is an ectoparasitic infestation by the pregnant sand flea Tunga penetrans. The flea is endemic to Sub-Saharan Africa, South America, the Caribbean, and parts of Asia, where it is a serious health problem.1 The flea is transmitted by direct contact of the skin with soil contaminated by pig or cow feces. It is typically a result of walking barefoot and lesions therefore often appear in the skin of the feet, particularly in the periungal area, although they can be seen in any region of the body.2
The clinical manifestations are highly variable, with isolated or multiple hyperpigmented papules being typical. It may present with pruritus or mild pain, but intense pain may also develop and walking may become impossible. Bacterial superinfection is the most common complication.2 Diagnosis is based on the clinical characteristics of the lesion, although histological study is sometimes needed.
In 2004, Bauer et al.3 used dermoscopy as an effective diagnostic aid for tungiasis. The dermoscopic characteristics they described included the presence of a brown ring around a central pore, which is the pigmented chitin surrounding the posterior opening of the sand flea's exoskeleton (Fig. 3, white arrow). Subsequently, a peripheral pigmented ring or halo was described, which is the posterior part of the abdomen of the parasite.4
Dermoscopy has also led to the description of additional tungiasis characteristics that are more variable and are not present in all patients, such as blue-gray spots, whitish chainlike structures, and the recently described radial crown sign.5,6 It should be noted that some of these signs have been described in white patients and that they are difficult to observe in black patients, as in the case we present.
The differential diagnosis of tungiasis includes myiasis, cutaneous larva migrans, scabies, bacterial infections, tumors, warts, and foreign-body reactions.
The most effective treatment involves surgical extraction of the flea, the administration of antibiotics, and tetanus vaccination; the role of other treatments, such as the use of ivermectin or thiabendazole, remains unclear. The use of adequate footwear is recommended as a preventative measure.1,2
Immigration has produced a significant increase in the incidence of tungiasis outside of areas where it is endemic, leading inevitably to diagnostic difficulties.1 As occurs in other parasitic infestations,5 dermoscopy can be helpful in patients in whom the diagnosis cannot easily be established on the basis of clinical findings.
Please cite this article as: Sendagorta E, Vidaurrázaga C, Raphael Mulekyo. Placa hiperpigmentada en el pie de un paciente keniata. Actas Dermosifiliogr.2012;103:633-634.