Angiolymphoid hyperplasia with eosinophilia (ALHE), also known as epithelioid hemangioma, is a chronic, benign vascular proliferation for which no cases of malignant transformation have been reported to date. Spontaneous resolution has been described in some patients,1 particularly in those with small lesions. ALHE is characterized by a high rate of recurrence (approximately 30%), regardless of treatment modality.2,3
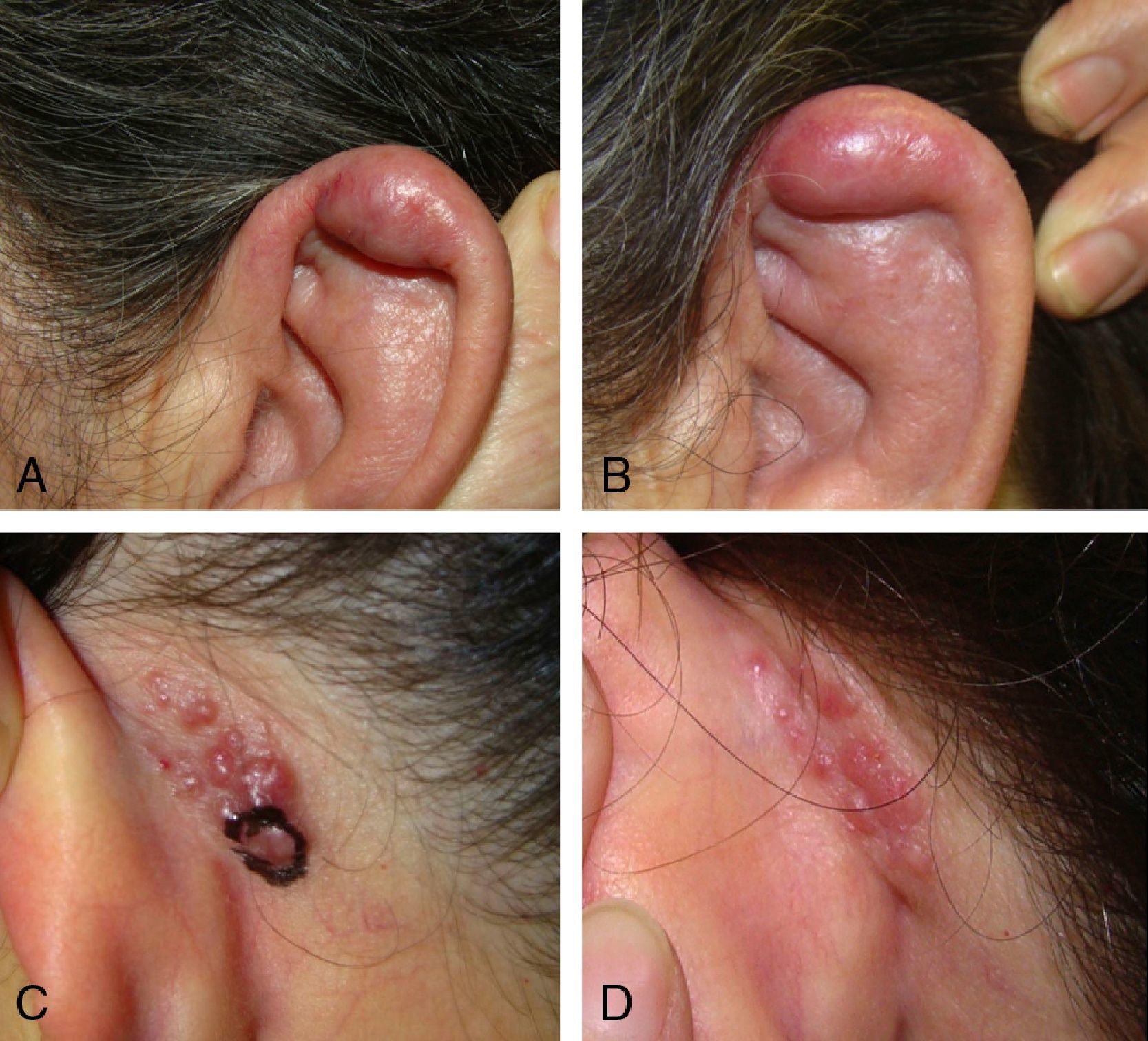
We describe the clinical and pathologic characteristics of 7 cases of ALHE diagnosed in our hospital between 2005 and 2011 (Table 1). Six of the patients were women; 5 of these were in their 40s and 1 was aged 75 years when the disease was diagnosed. The seventh patient was a 43-year-old man. The predominant clinical presentation was erythematous papules and plaques (Fig. 1). Subcutaneous masses were observed in 2 cases. In all 7 patients, the lesions were located on the head and neck, specifically in retroauricular areas, on the helix of the ear, on the nose, on the temple, in the posterior cervical region, and in the frontal region (2 cases). The most common treatment was surgical excision (5 cases). This produced a satisfactory clinical outcome, although recurrence was observed in 4 cases. Recurrent lesions were treated with cryotherapy, intralesional corticosteroid injections, and electrocoagulation, resulting in complete resolution in 1 case; the remaining lesions remained stable. Spontaneous involution following biopsy was observed in 1 patient with a single papular lesion on the nasal dorsum.
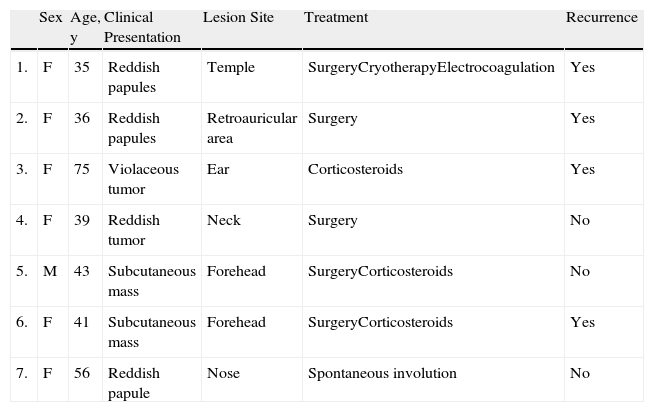
Review of 7 Cases of Angiolymphoid Hyperplasia With Eosinophilia Treated at our Hospital Between 2005 and 2011.
| Sex | Age, y | Clinical Presentation | Lesion Site | Treatment | Recurrence | |
| 1. | F | 35 | Reddish papules | Temple | SurgeryCryotherapyElectrocoagulation | Yes |
| 2. | F | 36 | Reddish papules | Retroauricular area | Surgery | Yes |
| 3. | F | 75 | Violaceous tumor | Ear | Corticosteroids | Yes |
| 4. | F | 39 | Reddish tumor | Neck | Surgery | No |
| 5. | M | 43 | Subcutaneous mass | Forehead | SurgeryCorticosteroids | No |
| 6. | F | 41 | Subcutaneous mass | Forehead | SurgeryCorticosteroids | Yes |
| 7. | F | 56 | Reddish papule | Nose | Spontaneous involution | No |
Abbreviations: F, female; M, male.
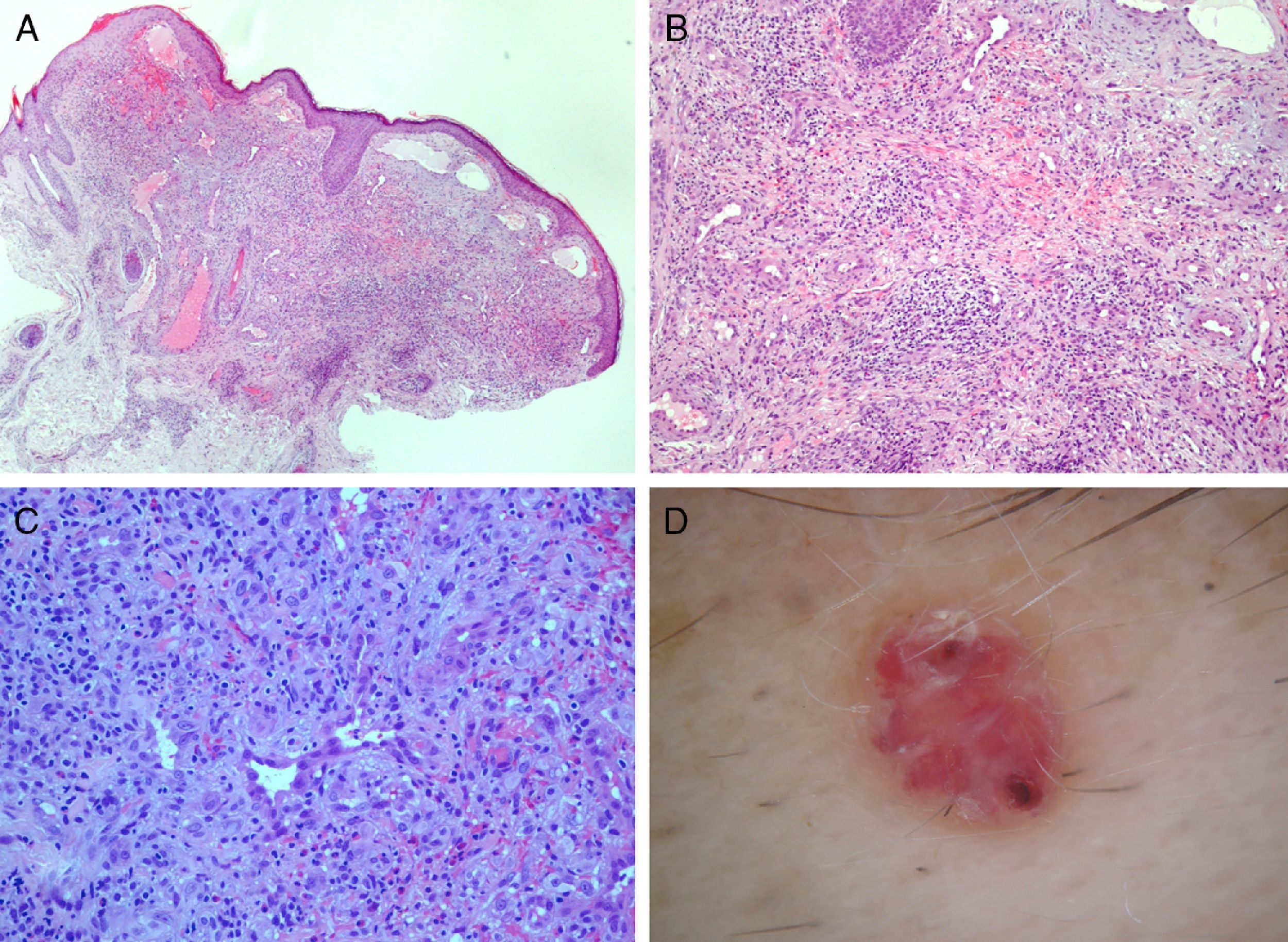
None of the patients had peripheral eosinophilia, palpable lymph nodes, or a history of trauma in the area of the lesions. Dermoscopic evaluation of 1 of the lesions showed a lacunar pattern similar to the characteristic pattern seen in hemangiomas (Fig. 2).
ALHE is considered a rare entity, although it is also believed to be underdiagnosed because of its diverse clinical presentations. Histology, therefore, has a key diagnostic role in this disease. Characteristic findings include prominent epithelioid-like endothelial cells lining the vascular lumen and surrounded by a mixed, predominantly eosinophilic, inflammatory infiltrate (Fig. 2).4,5
The differential diagnosis is very wide, with Kimura disease generating the most controversy.6 Until recently, ALHE and Kimura disease were considered to represent opposite ends of the same entity, but they are now considered to be separate diseases due to their clinical and histologic differences. Considering the large number of disorders in the differential diagnosis, biopsy of lesions is a key diagnostic tool in ALHE. There are many treatment options for ALHE, the most common of which are surgical excision, cryotherapy, and intralesional corticosteroids. Cryotherapy was used to treat papular lesions on the face of 1 of our patients, with favorable clinical and cosmetic results. Considering that it is fast and simple, this treatment modality is a viable option for superficial lesions. Electrocoagulation is also useful for superficial lesions, particularly when they are small. We achieved control of a lesion located on the edge of the helix of an elderly patient with intralesional corticosteroids, although the lesion did not resolve completely. The patient refused to undergo more invasive treatment. Surgical excision is perhaps the most viable therapeutic option for subcutaneous masses in ALHE.7
Less common treatments described in the literature include laser therapy (considered the first-line alternative for superficial lesions), pentoxifylline, indomethacin, retinoids, chemotherapeutic agents (bleomycin, vinblastine, fluorouracil), levamisole, and interferon.8
As seen, many treatment options exist for ALHE, but there is no consensus on the treatment of choice due to the shortage of studies. Considering that ALHE is a benign condition that follows a chronic, recurrent course, perhaps the best option in the majority of cases is a conservative, watch-and-wait approach.
The largest series of ALHE cases identified in our review of the literature was one involving 116 patients (with a predominance of men) reported in 1985.9 In Spain, the largest series published to date involved 52and 310 patients. In this second study, good results were achieved with vascular laser therapy.
With 7 cases, ours is the largest series of ALHE to be published in Spain to date. We have performed a review of the literature on this entity and described the first—to our knowledge—dermoscopic analysis of an ALHE lesion.
Please cite this article as: Padilla-España L, et al. Hiperplasia angiolinfoide con eosinofilia. Revisión de 7 casos. Actas Dermosifiliogr. 2013;104:353–5.