Pediatric anogenital condyloma acuminata (CA) is not infrequent, as increasing reports of its prevalence have demonstrated in recent years.1,2 However, periurethral CA is an unusual location for this virally transmitted disease and is exceptionally reported in medical literature. Human papilloma viruses (HPV) are the etiological causes for all types of warts, and variable modes of transmission both sexual and non-sexual, have been described in the pediatric population.1 Current treatments for anogenital CA in children prove challenging due to their young age, anatomic location and the high recurrence rates.1,3 Multiple therapeutic approaches range from topical treatments to more aggressive procedures, including surgery.4,5
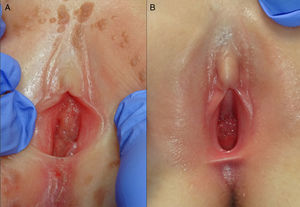
We present an otherwise healthy, 2-year-old girl referred to our Department of Dermatology, with progressively increasing asymptomatic lesions in the diaper area of 2 months in duration. Physical examination showed multiple flesh-colored and brownish papules of 1–2mm in diameter located in the vestibular and vulvar region in a symmetric V-shaped distribution as well as in the perianal region (Fig. 1(A)) Additionally, careful periurethral examination revealed an exophytic, reddish and papillomatous lesion of 1.2cm in diameter (Fig. 2(A)) observing rich vascularity with dermoscopy.
A clinical diagnosis of CA stage IV was established due to the extension of the lesions.2 PCR testing was performed for the vulvar, perianal and the periurethral lesions confirming the diagnosis of CA for HPV subtype 6. Subsequently, the patient was screened for other sexually transmitted diseases and reported to social services for possible child abuse investigations. The father presented genital warts, however, PCR testing results were not conclusive for the detection and typification of the HPV. No further information was retrieved from the mother. The exact source of infection could not be determined, but most importantly, no signs of sexual abuse were identified.
CO2 laser surgery was proposed as a prompt solution for lack of sphincter control and the giant periurethral CA. The procedure was carried out in an in-patient regimen under general anesthesia and prophylactic systemic antibiotic with cefazolin. Under gynecological examination, urethral catheterization was performed. The operators were required to use a mask to prevent HPV in the vapor plume emitted by the CO2 laser. Vaporization with CO2 laser was performed with the following parameters: 5 Watts, continuous mode and repeated pulse in two consecutive passes. After vaporization and using the same CO2 laser parameters, the periurethral wart was coagulated from the base and sent for histopathological analysis. The treated area was covered with mupirocin ointment and a non-adherent dressing, both of which were changed on a daily basis until complete healing was achieved. The laser surgery lasted approximately 30min with no intra or postoperative complications. The histopathological study revealed acanthosis and parakeratosis with elongation of rete ridges and the presence of koilocytes, features consistent with CA. Complete epithelialization was achieved within 9 days and only one session was required to achieve clearance. The giant periurethral and anogenital CA did not recur. A 13-month follow-up shows complete remission and no signs of scarring (Fig. 1(B) and 2(B)).
Anogenital CA in the pediatric population is not rare in daily practice as one may suppose.1,2 However, giant periurethral condyloma occurs exceptionally in association with extensive dissemination of CA.4,5 Most importantly, anogenital HPV infection in this particular age group poses a therapeutic challenge. Among several treatment recommendations for CA are podophyllin or imiquimod,2 trichloroacetic acid, 5-fluorouracil,1 cryotherapy, CO2 laser,3 electrocautery and surgery,5-7 all of which present variable cure and recurrence rates. The multiple approaches and varying responses suggest that there is no gold standard for the treatment of CA in children6-8 and while topical treatments are indicated as a first line approach, there is no consensus regarding pediatric management.7-9
In our case, topical therapy was not a treatment option owing to the clinical presentation of the periurethral CA. Another important factor taken into account, was the infant that required diapers, for the occlusion and constant diaper changes would have interfered with the topical treatments, leading to possible lack of therapeutic effectiveness and adherence. However, the greatest concern was the periurethral wart, which due to size and location required a surgical procedure.5,9
CO2 laser surgery is an effective technique, demonstrating rapid healing and lower recurrence rates as the main advantages.1,4 In our patient's case, after 9 days and only one session, complete epithelialization was achieved and no recurrence was observed in the 13-month follow-up (Fig. 2(B)). To our knowledge, this is the first pediatric case presenting a periurethral CA successfully treated with CO2 laser reported in medical literature.
In summary, we report the outstanding results achieved with the CO2 laser for the treatment of a periurethral and disseminated CA in a pediatric patient. We therefore recommend this surgical procedure in cases where large CA in association with extensive disseminated infection are observed.
Conflicts of interestThe authors declare that they have no conflicts of interest.