An 8-year-old girl was referred by endocrinology to the dermatology department for assessment of mildly pruritic lesions in both axillae. The lesions had developed over a long period of time and were more severe in the left armpit. The patient, whose parents were natives of Romania, was in follow-up by pediatric endocrinology due to precocious puberty, with slightly elevated testosterone levels (normal Synacthen test). She had also presented with an episode of acute gastroenteritis with liver failure, which required follow-up for 3 years.
Physical examination revealed yellowish elastic papules measuring between 1 and 2 mm, with a perifollicular distribution, grouped in localized plaques in both axillae, with more patchy grouping on the left side (Figs. 1 and 2).
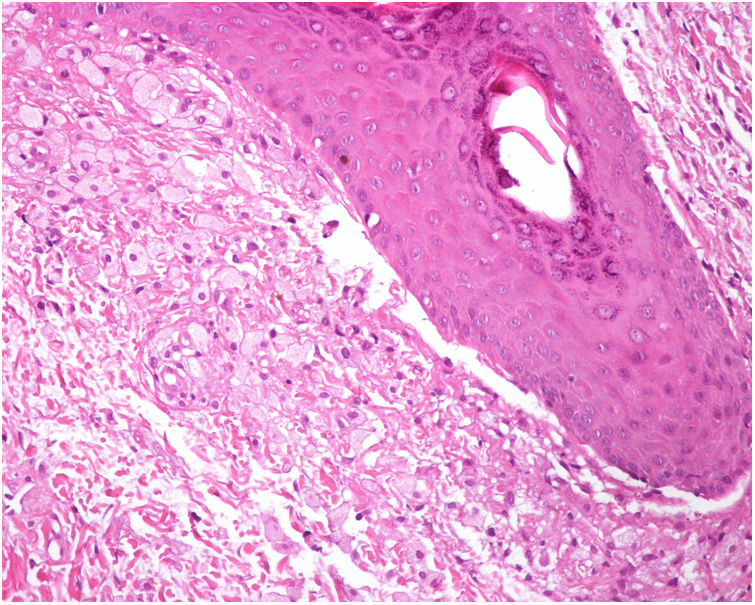
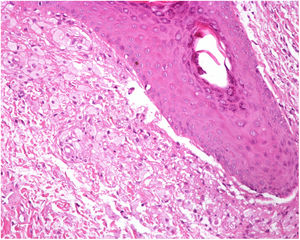
Histology of a punch biopsy of one of the lesions revealed dilation of the follicular infundibulum and a perifollicular aggregation of foam cells (Fig. 3). These results were compatible with a diagnosis of Fox-Fordyce disease (FFD).
The clinical course was favorable, with spontaneous improvement of the lesions. The only relevant family history was that her mother reported hyperhidrosis and axillary bromhidrosis, and she was therefore discharged with local antiperspirant on demand (aluminum chlorohydrate, 15%). It was not possible to establish a temporal relationship between the patient’s underlying endocrinologic disease and the appearance or improvement of the lesions.
FFD, also known as apocrine miliaria, was first described in 1902 by George Henry Fox and John Addison Fordyce. It is a rare chronic disease that typically appears in postpubescent women (15–35 years of age).1 Presentation in childhood is exceptional.2 The etiology is unknown and the cause is probably multifactorial.3 Its association with hormonal factors has been postulated, given the age range in which it appears and the frequent remission of the disease during pregnancy and menopause, although it has not been possible to show any hormone abnormality in patients.1 We do not therefore know whether an association exists with the precocious puberty in our patient. We have found no previous association with liver failure in the literature.
Appearance of the disease as an adverse effect of laser or intense pulsed light (IPL) depilation techniques has been reported.4 In this case, the clinical and histologic findings are very similar to primary FFD.
It presents clinically as small dome-shaped pruritic perifollicular papules the color of yellowish-healthy skin. The most common location is the axillae but the lesions may also present in the periareolar or anogenital region, and, more rarely, on the thighs, the periumbilical region, and sternum. The disease may be associated with hair loss in the affected areas and hypohidrosis.
The lesions improve with pregnancy and the use of hormonal contraceptives, and worsen with heat, hot water, stress, and the menstrual cycle.1
The clinical presentation of the disease is constant and similar. Histological findings, however, vary widely.5 Formation of a keratin plug in the follicular infundibulum, which also obstructs the apocrine duct may be the trigger.3 The most consistent feature is dilation of the infundibulum and hyperkeratosis of the infundibular epithelium.5 The most specific finding is perifollicular xanthomatosis.6
It was traditionally believed that this disease involved only the apocrine glands. Recent histological findings, however, suggest that eccrine and nonfollicular variants (involving the apocrine glands) may exist.3
The clinical differential diagnosis of this entity should basically include eruptive syringoma, lichen nitidus, trichostasis spinulosa, Graham-Little-Piccardi-Lasseur syndrome, and Darier disease.1,7,8
Because it is a rare disease, comparative studies are not available, and treatment remains unclear. Multiple treatments have been described, all of them with variable results. Topical or intralesional corticosteroids are considered to be the treatment of choice. Topical and systemic retinoids, topical antibiotics such as clindamycin, antiperspirants, oral contraceptives, and topical calcineurin inhibitors have also been used. Curettage and electrocoagulation, modified liposuction techniques, and, more recently, fractional CO2 laser, microwaves, and botulinum toxin A have been used in refractory cases.9–11
Spontaneous remission, as in the case of our patient, is anecdotal.
In summary, we report a case of FFD that is exceptional due to onset in prepubertal age and its atypical course, with spontaneous resolution of the lesions. We cannot state the causal relationship with the patient’s endocrinologic abnormalities, although they probably play a major role in the development of the disease.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Huerta-Vena A, Tardío JC, Hernández-Núñez A, Borbujo J. Enfermedad de Fox-Fordyce en edad infantil. Actas Dermosifiliogr. 2020. https://doi.org/10.1016/j.ad.2019.03.016