A 24-year-old woman with no relevant past history presented with a fast-growing, asymptomatic nodular lesion on the left lower eyelid that had first appeared 5 months earlier. The patient reported no history of manipulation or trauma in the affected area. However, she did report an episode of pain, redness, and edema on the left cheek a month earlier, which was resolved with an oral antibiotic.
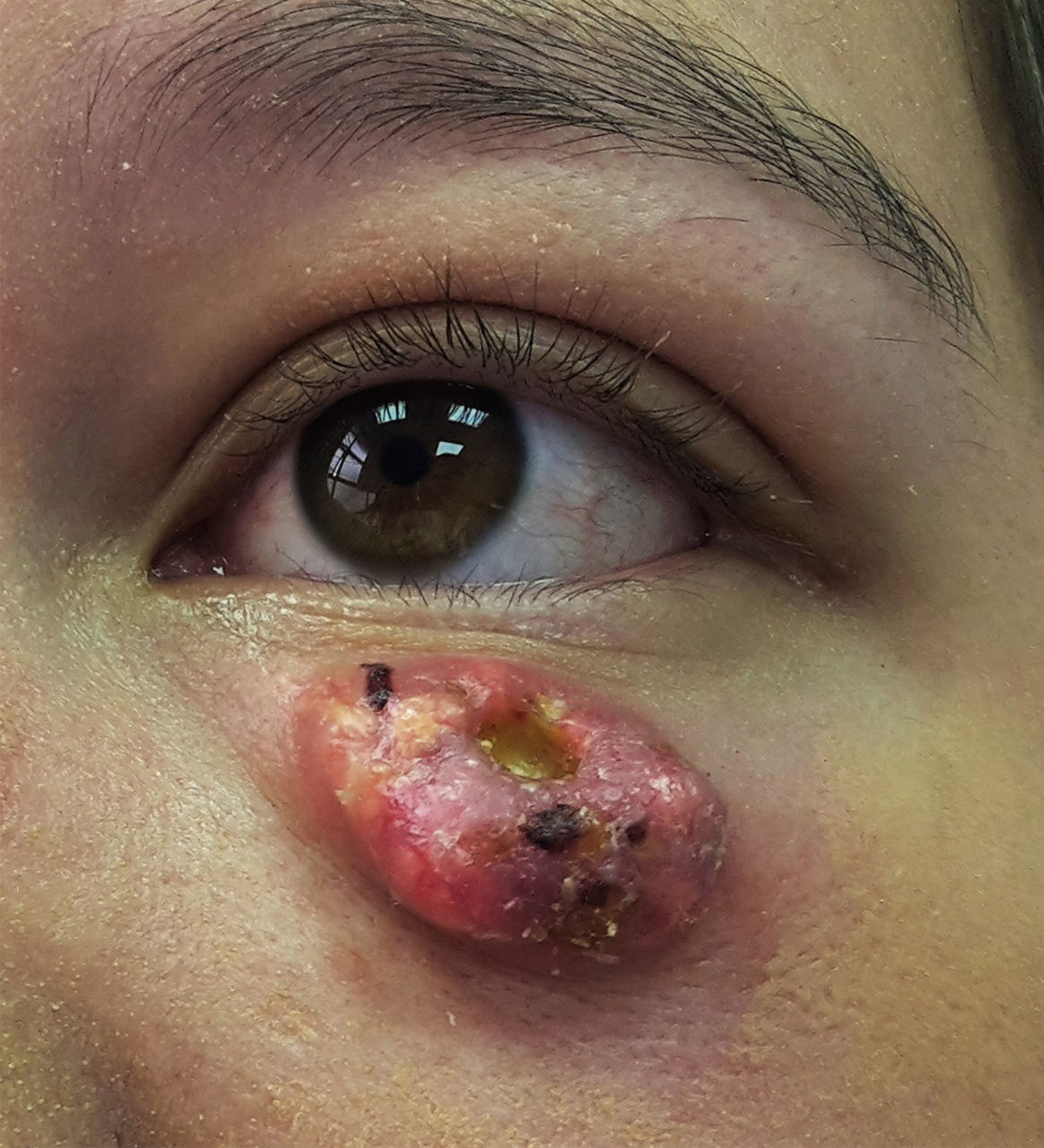
Physical ExaminationPhysical examination revealed a 2.5×1.5cm multilobulated, erythematous nodule with yellowish-white areas that was firm on palpation and had a smooth, friable surface, a few telangiectasias, hematic crusts, and an ulcerated central depression (Fig. 1).
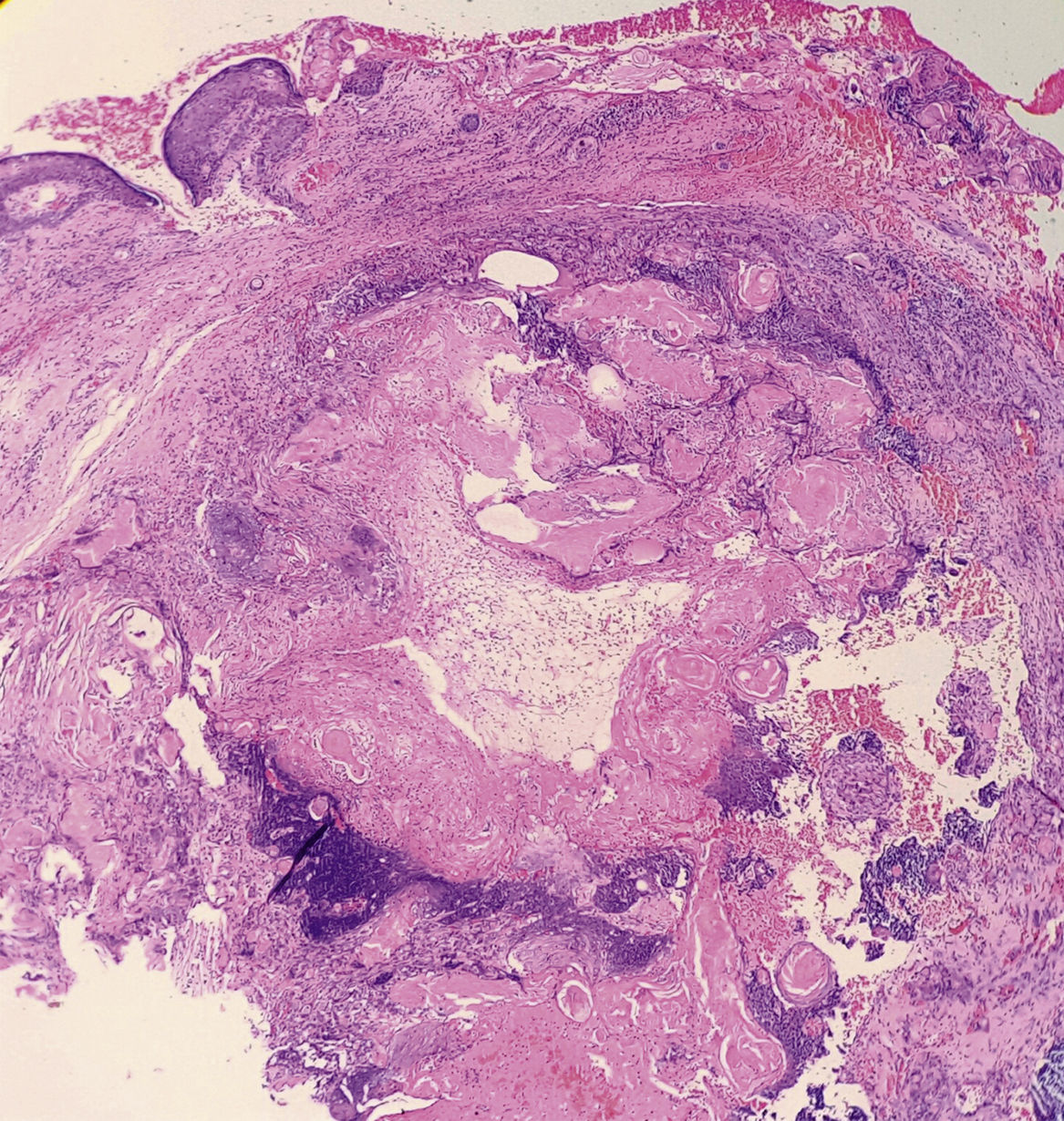
HistopathologyHistologic examination revealed a dermal lesion composed of basaloid cells and ghost cells, with foci of calcification surrounded by fibrous stroma without atypia (Fig. 2).
What Is Your Diagnosis?
DiagnosisPerforating pilomatrixoma.
Clinical CourseComplete excision of the lesion was carried out under local anesthesia. No recurrence of the lesion was observed during a 6-month follow-up period (Fig. 3).
CommentPilomatrixoma, a benign tumor of the hair follicle matrix, is among the most common skin neoplasms in children and young adults.1 It is more common in women and usually appears on the head and neck, where it manifests as a single subcutaneous nodule measuring 0.5-2cm in diameter that is firm on palpation, with blood vessels and discoloration of the overlying skin.2 The perforating presentation is extremely rare and fast-growing; it is characterized by the elimination of the content of the tumor, with or without ulceration, depending on the depth of the lesion.3 Diagnosis is confirmed by histologic examination, which shows basophilic cells, and, in the perforating variant, ossification and transepidermal elimination.4 Pilomatrixoma is usually confused with other lesions such as epidermoid cyst, keratoacanthoma, molluscum contagiosum, foreign body granuloma, juvenile xanthogranuloma, sebaceous carcinoma, matrical carcinoma, dermatofibrosarcoma protuberans, and amelanotic melanoma, and preoperative diagnosis is correct in only 21%5 to 54%2 of cases. Spontaneous remission has not been reported. The lesion is treated by surgical excision, with an estimated recurrence risk of 3%-4%.2
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Morales-Cardona CA, Rodríguez-Zakzuk C, Téllez-Lozada A. Tumor de rápido crecimiento en el párpado. Actas Dermosifiliogr. 2018;109:265–266.