The patient was an 89-year-old woman who had been diagnosed 40 years earlier with multiple trichilemmal cysts, and had no other medical history of interest. She was referred to our clinic for an asymptomatic ulcerated lesion on the scalp that had appeared 2 months earlier.
Physical ExaminationPhysical examination revealed a solid-to-keratotic, exophytic, crateriform tumor of 4 cm in diameter located in the occipital region and adhered to deep planes (Fig. 1). The lesion was surrounded by multiple previously diagnosed trichilemmal cysts. No other lesions were detected, and lymph node enlargement was absent.
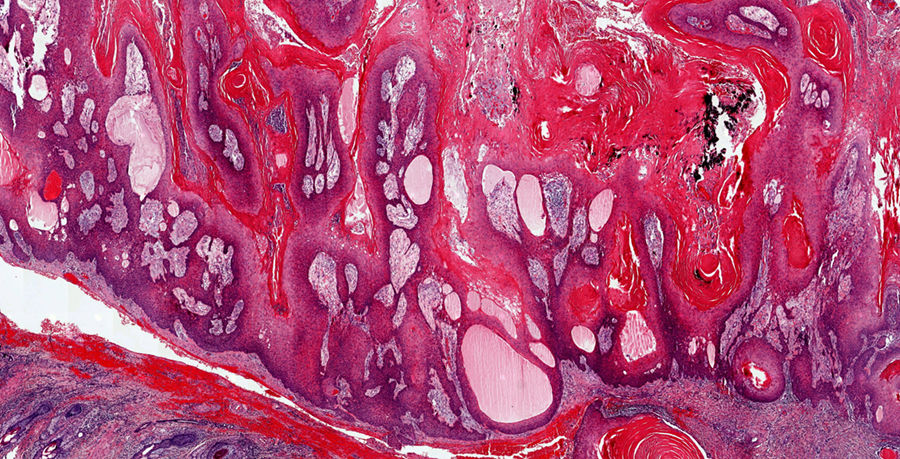
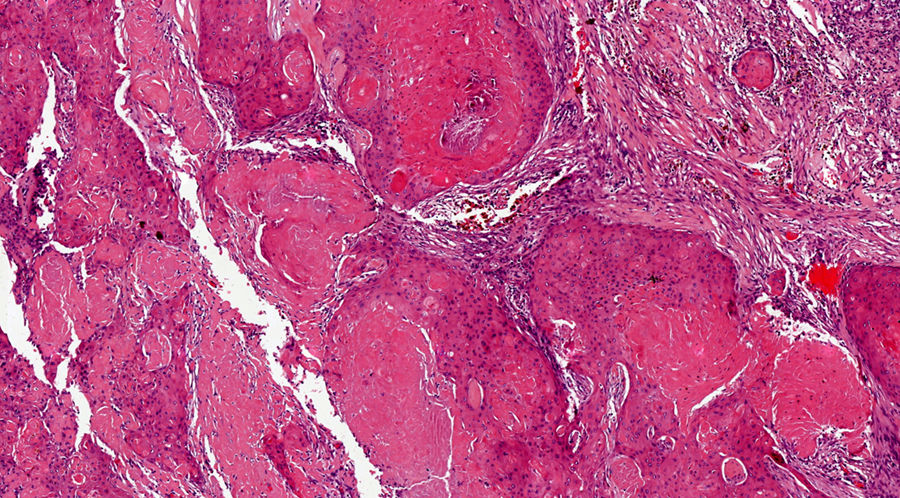
HistopathologyThe lesion was excised for pathological examination, which revealed a well-delimited and unencapsulated epithelial proliferation located in the superficial reticular dermis with an endophytic and exophytic growth pattern. This hyperplasia consisted of multiple partially cystic epithelial cords and lobules, with peripheral palisading and central trichilemmal keratinization. More detailed analysis revealed mild-to-moderate cellular atypia, with no aberrant mitoses or areas of necrosis (Figs. 2 and 3).
What Is Your Diagnosis?
DiagnosisProliferating pilar tumor (PPT).
CourseThe patient showed no recurrence after 6 months of follow-up.
CommentPPT is an adnexal tumor derived from the external radicular membrane of the hair follicle.1 It usually presents as an exophytic scalp tumor, in many cases with ulceration, bleeding, and/or superinfection, and typically affects women aged 40 years and older. However, cases involving tumors in atypical locations, including the thorax, back, buttock, nose, and vulva, have also been described.2 In most cases PPT arises from a pre-existing trichilemmal cyst, although de novo forms, which develop in the absence of pre-existing lesions, are also described.3
Histologically, PPT is characterized by hyperplasia consisting of solid or partially cystic epithelial cords or lobules, with peripheral palisading and trichilemmal keratinization.1–3 Areas of necrosis, anaplastic cells, and aberrant mitoses are common.3,4 PPT can be associated with foreign body reaction, dystrophic calcification, squamous eddies, and areas of vacuolization or dyskeratosis.2,4
When differentiating PPT from squamous cell carcinoma, foci of trichilemmal keratinization, sharp delimitation, areas of calcification, and the absence of premalignant epidermal lesions help orient the diagnosis towards PPT.5 The differential diagnosis should also include sebaceous carcinoma, clear cell hidradenocarcinoma, pilomatrixoma, and trichoblastoma.6,7
PPT follows an unpredictable course and lies on a spectrum ranging from benign trichilemmal cysts with minimal epithelial proliferation to malignant PPT with local invasion, a tendency to recur, and occasional distant metastases.3,5,8 An infiltrative pattern with cellular anaplasia, atypical mitoses, and/or areas of necrosis are considered histological markers of poor prognosis.2 The treatment of choice is exeresis with wide margins (1–2 cm) or Mohs micrographic surgery, although a good therapeutic response has also been reported in patients treated with radiotherapy.8,9
In conclusion, we describe a representative case of a little-known adnexal lesion, knowledge of which is necessary in order to select the appropriate therapeutic measures.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Varas-Meis E, Prada-García C, Fernández-Canga P, Rodriguez-Prieto MÁ. Tumoración occipital de rápido crecimiento. Actas Dermosifiliogr. 2019;110:497–498.