The patient was a 60-year-old woman, allergic to metamizol, acetylsalicylic acid, boric acid and oxaliplatin, with untreated rheumatoid arthritis and stage IV colon adenocarcinoma, for which she had undergone surgery (sigmoidectomy and hepatic metastectomy) 6 months previously, and was receiving chemotherapy with 5-fluorouracil and bevacizumab. She presented at the emergency room with erythematous lesions on the limbs and a fever of 24 hours’ duration.
Physical ExaminationPhysical examination revealed erythematous macules and plaques that were very painful on palpation on the inner aspect of the right foot, the palm of the left hand, and the abdomen and thighs (Fig. 1).
A skin biopsy was taken from the affected area of the right foot.
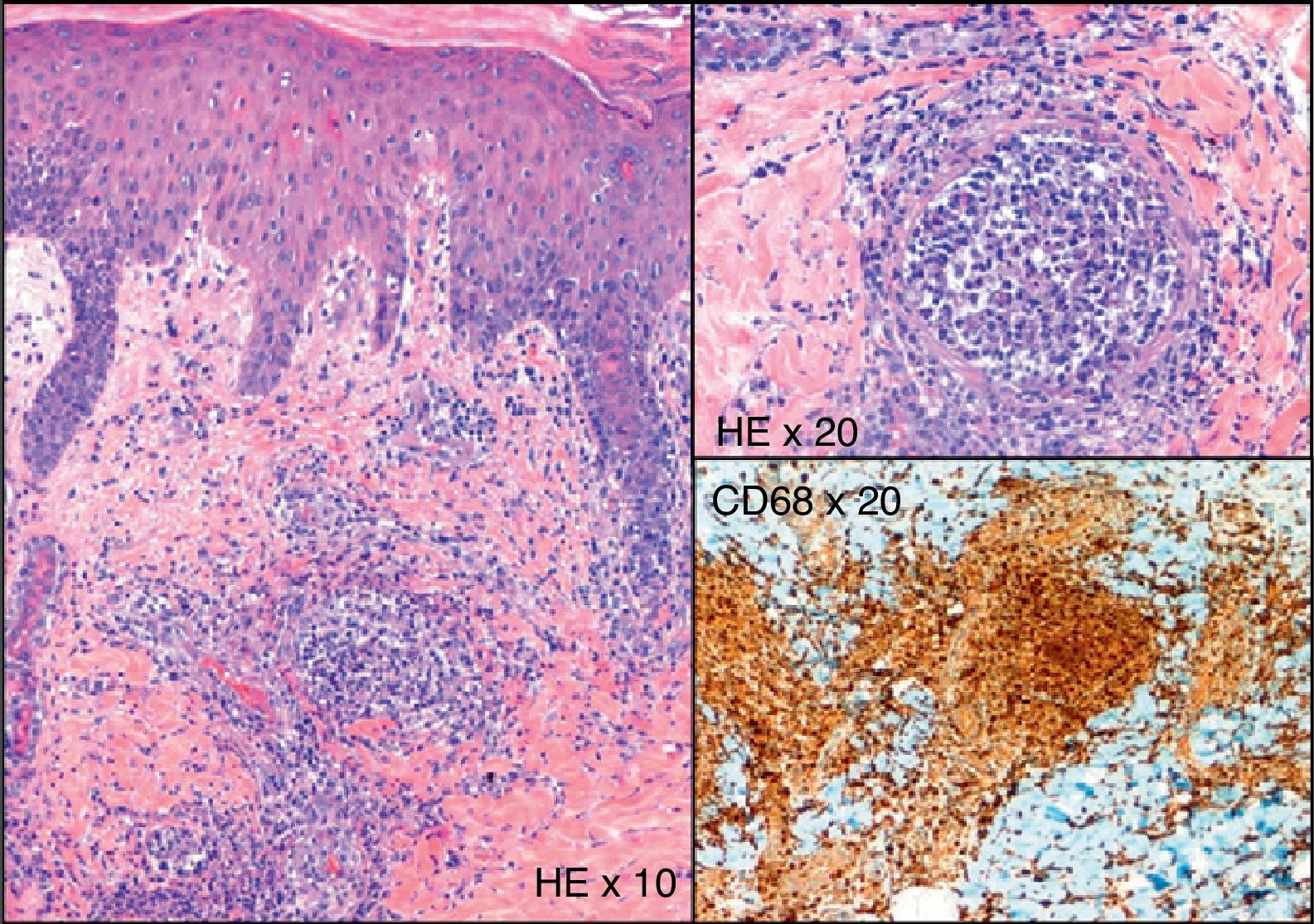
HistopathologyHistologic examination revealed marked dilatation of vessels of the superficial and deep dermis, the lumina of which contained large mononuclear cells with broad granular, eosinophilic cytoplasm and little atypia (Fig. 2). Immunohistochemistry revealed that these cells were positive for CD68, CD45, and CD43, and negative for CD20, CD3, cytokeratins 7 and 20, CD31, and factor VIII. The endothelium was positive for D2-40. No neutrophilic elements or markers of malignancy were observed.
Additional TestsAnalyses performed in the emergency room revealed a normal blood count and elevated levels of fibrinogen and C-reactive protein. All other biochemical and coagulation parameters were normal. Blood, urine, and skin biopsy cultures were all negative.
What Is Your Diagnosis?
DiagnosisIntralymphatic histiocytosis.
Clinical Course and TreatmentThe patient was treated empirically with amoxicillin-clavulanate (875mg/125mL) every 8hours, and treatment with prednisone (0.5mg /kg/day) was initiated 5 days later. Within 2 weeks both the fever and skin lesions had resolved.
CommentIntralymphatic histiocytosis is a rare condition with diverse clinical manifestations but characteristic histology and immunohistochemistry. Most reported cases are associated with chronic inflammatory processes, particularly rheumatoid arthritis, and less frequently joint replacement and tumors such as breast cancer, Merkel cell carcinoma, and colonic neoplasia.1–5 While the etiology and pathogenesis of this condition are unknown, its association with these diseases suggests that it could be due to lymphatic stasis and dilation of lymphatic vessels, in which the persistent presence of antigens stimulates the aggregation and proliferation of histiocytes.1
The most common clinical presentation is characterized by poorly defined erythematous plaques, mainly on the limbs, sometimes in association with livedo reticularis or superficial papules, vesicles, or nodules.1,2 Fever has not been reported in any of the cases described to date, but is commonly observed in immunosuppressed patients undergoing chemotherapy. Similarly, local pain has not been previously reported, and may be due to the almost total vascular occlusion observed in our patient.
Histologically, intralymphatic histiocytosis is characterized by dilatation of vessels in the dermis and the presence of large mononuclear cells with granular eosinophilic cytoplasm in the vascular lumina. Immunohistochemical techniques are fundamental to confirm that the dilated vessels are lymphatic vessels (positive for D2-40, Lyve-1, and Prox-1), and that the cells occluding the vessels are histiocytes (CD68+).1,2
The lesions usually follow a benign course and tend to resolve spontaneously, although in many cases a chronic course is observed. Multiple treatments have been used,1 including radiation therapy, topical corticosteroids, cyclophosphamide, pentoxifylline, infliximab,5 amoxicillin, and aspirin.
Histologic differential diagnosis should include intravascular lymphoma and reactive angioendotheliomatosis.1,2 Intravascular lymphoma is a rare and aggressive subtype of large B-cell lymphoma, which mainly affects the vessels of the skin and central nervous system and is associated with a poor prognosis. Histologic examination and immunohistochemistry can confirm that the dilated vessels are blood vessels and the cells they contain are lymphocytes, usually B-lymphocytes and hence CD20+ and CD79a+. Angioendotheliomatosis is a benign reactive process characterized by the proliferation of endothelial cells that obliterate blood vessels, and is associated with infectious diseases such as tuberculosis, hematologic neoplasms, leukocytoclastic vasculitis, occlusive vascular disorders, and rheumatoid arthritis The blood vessels are dilated and are not reactive to D2-40, Lyve-1, or Prox-1, while endothelial cells exhibit CD31, CD34 and factor VIII immunoreactivity.
Other conditions that present with histiocytes are Rosai-Dorfman disease (with emperipolesis and S-100 immunoreactivity), Melkersson-Rosental syndrome, sclerosing lymphangitis of the penis, and granulomatous lymphangitis of the penis and scrotum.1 Furthermore, in cases where the vascular lumina are occluded by abundant cellular elements, metastasis of solid carcinomas and leukemias must be ruled out.
Conflict of InterestThe authors declare that they have no conflicts of interest.
We are sincerely grateful to the department of pathology, whose input is often essential in diagnoses.
Please cite this article as: P. Borregón, J.A. Avilés, V. Parra. Placas eritematovioláceas en extremidades de paciente con arthritis reumatoide y cáncer de colon. Actas Dermosifiliogr. 2012;103:543-4.