Erythema multiforme associated with phenytoin and cranial radiation therapy (EMPACT syndrome) was first described by Ahmed et al.1 in 2004 in a series of patients with dermatosis secondary to cranial radiation therapy and phenytoin treatment. Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are acute bullous dermatoses caused mainly by the use of drugs such as phenytoin.
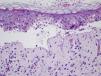
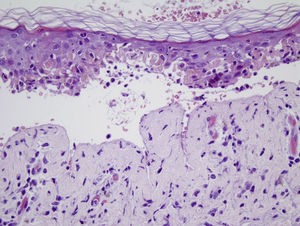
A 54-year-old man diagnosed with pulmonary adenocarcinoma (T3-4N2M1) with a single intracranial metastasis underwent cranial radiation therapy with a total dose of 30Gy (fractional dose=300cGy). The radiation therapy was completed 1 week before the onset of the skin condition. The patient had been receiving phenytoin as a prophylactic anticonvulsant and oral dexamethasone for 5 weeks. Physical examination revealed small, atypical, target-shaped, erythematous-edematous lesions with a tendency to coalesce on the face, neck, trunk, and root of the upper limbs, occupying 35% of the body, with skin detachment in the affected areas. Marked conjunctival injection and intense involvement of the oral mucosa, with labial edema and erosive lesions, were also present (Fig. 1). Biopsy of a lesion in the supraclavicular region revealed an intense interface lesion in both the epidermis and the follicular epithelium, with abundant necrotic keratinocytes (isolated or in groups), a moderate lymphocytic inflammatory response, and areas of epidermal detachment with partial necrosis of the detached epidermis (Fig. 2). As therapeutic management, treatment with phenytoin was suspended and substituted by levetiracetam, and adjuvant therapy was also started. The lesions responded well, remaining stable in relation to the neoplastic disease.
Prophylactic use of anticonvulsants is routine in patients who undergo cranial radiation therapy. As in the case of our patient, phenytoin is usually the drug of choice, although other drugs, such as carbamazepine, levetiracetam, and lamotrigine are occasionally used.
Although skin reactions occur after ingestion of phenytoin in 19% of cases, severe cutaneous manifestations such as SJS and TEN are rare.1,2 Although these conditions are unusual, it is very important that they be taken into account in order to avoid potentially life-threatening complications.
In recent years, the association of cranial radiation therapy and phenytoin has been shown to increase the risk of skin lesions known as the EMPACT syndrome.3 However, severe SJS-type or TEN-type cutaneous-mucosal manifestations, such as those seen in our patient, only occur in a small percentage of cases and can be life-threatening.4 This complication presents as erythematous-edematous macules and papules that are initially limited to the irradiated area, later progressing to epidermal detachment in larger areas (Nikolsky sign) with considerable involvement of the oral and ocular mucosas.5 In our patient, oral mucosal involvement was the first manifestation—an indication of the variability of the first manifestations.
The pathogenesis is unknown, although it has been suggested that radiation therapy could induce a deficit of epoxide hydroxylase, an enzyme responsible for eliminating toxic metabolites of phenytoin.6 More controversial is the possibility of a type IV hypersensitivity reaction to phenytoin and its metabolites, exacerbated by the action of the radiation therapy and the deficient metabolization of the toxic products of the drug.5,7
The use of levetiracetam or gabapentin as alternative drugs—either initially or as a substitute for phenytoin—should therefore be considered because the degradation of these drugs does not take place via the same metabolic pathway.
In conclusion, we present a case of the EMPACT syndrome with unusually severe cutaneous and mucosal involvement. Prophylactic use of anticonvulsants should be considered on a case-by-case basis. If anticonvulsant use is essential, the appearance of cutaneous-mucosal lesions should be monitored closely and the drug should be suspended when the first suspicious symptom appears.
Please cite this article as: Vilas-Sueiro A, Vázquez-Osorio I, Suárez-Peñaranda JM, Sánchez-Aguilar D. Síndrome Erythema Multiforme associated with Phenytoin And Cranial radiation Therapy (EMPACT) en paciente con neoplasia pulmonar. Actas Dermosifiliogr. 2016;107:169–170.