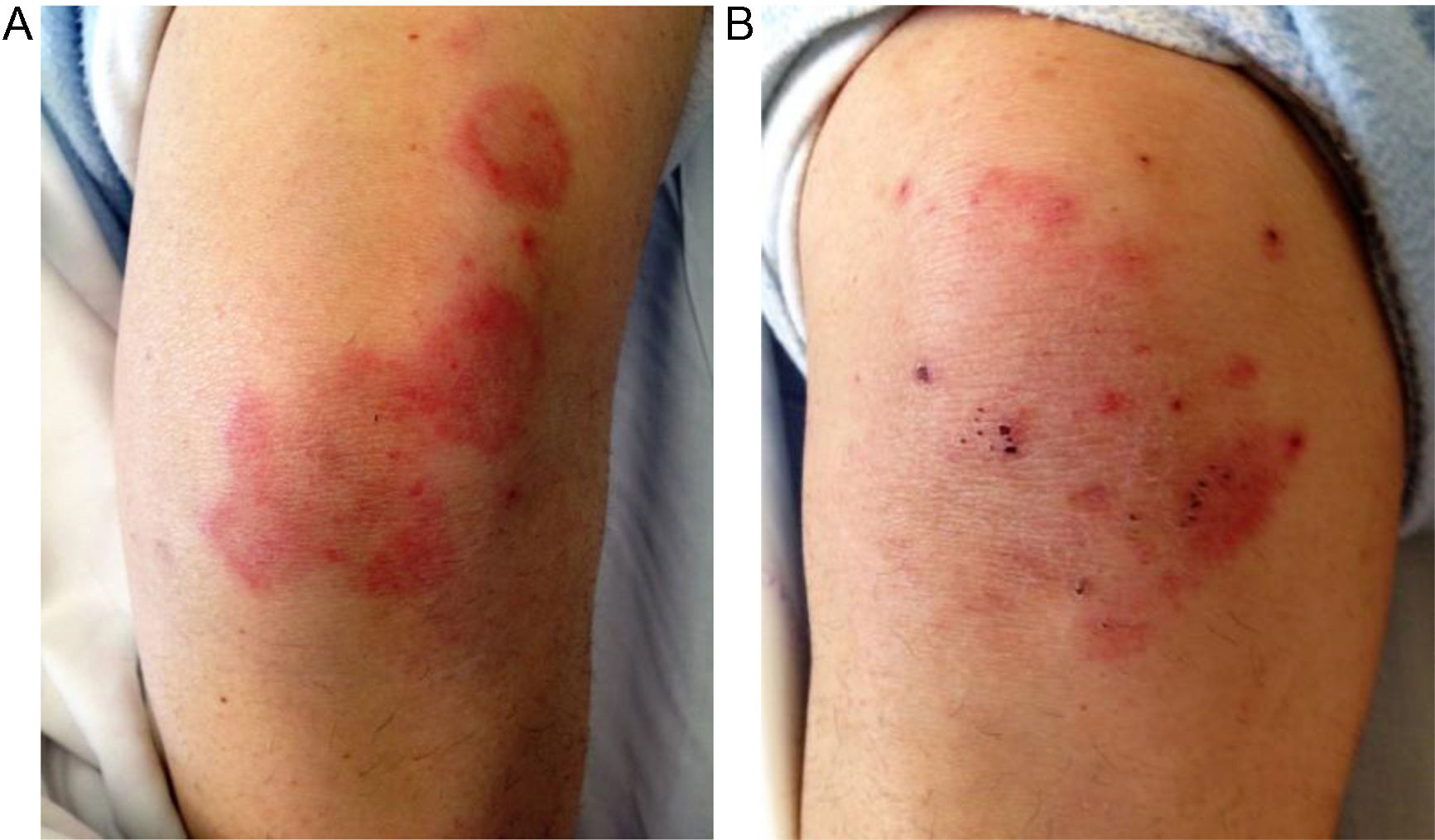
A 56-year-old woman was observed for non-pruritic erythematous annular plaques, located symmetrically on knees, which have started 3 months before and had been progressing with peripheral extension and central clearing (Fig. 1). Past medical history was unremarkable until 1 week before, when she presented with abdominal pain, nausea, hepatomegaly, ascites, decreased urinary output and asthenia. Family history was irrelevant and the patient denied taking any medication.
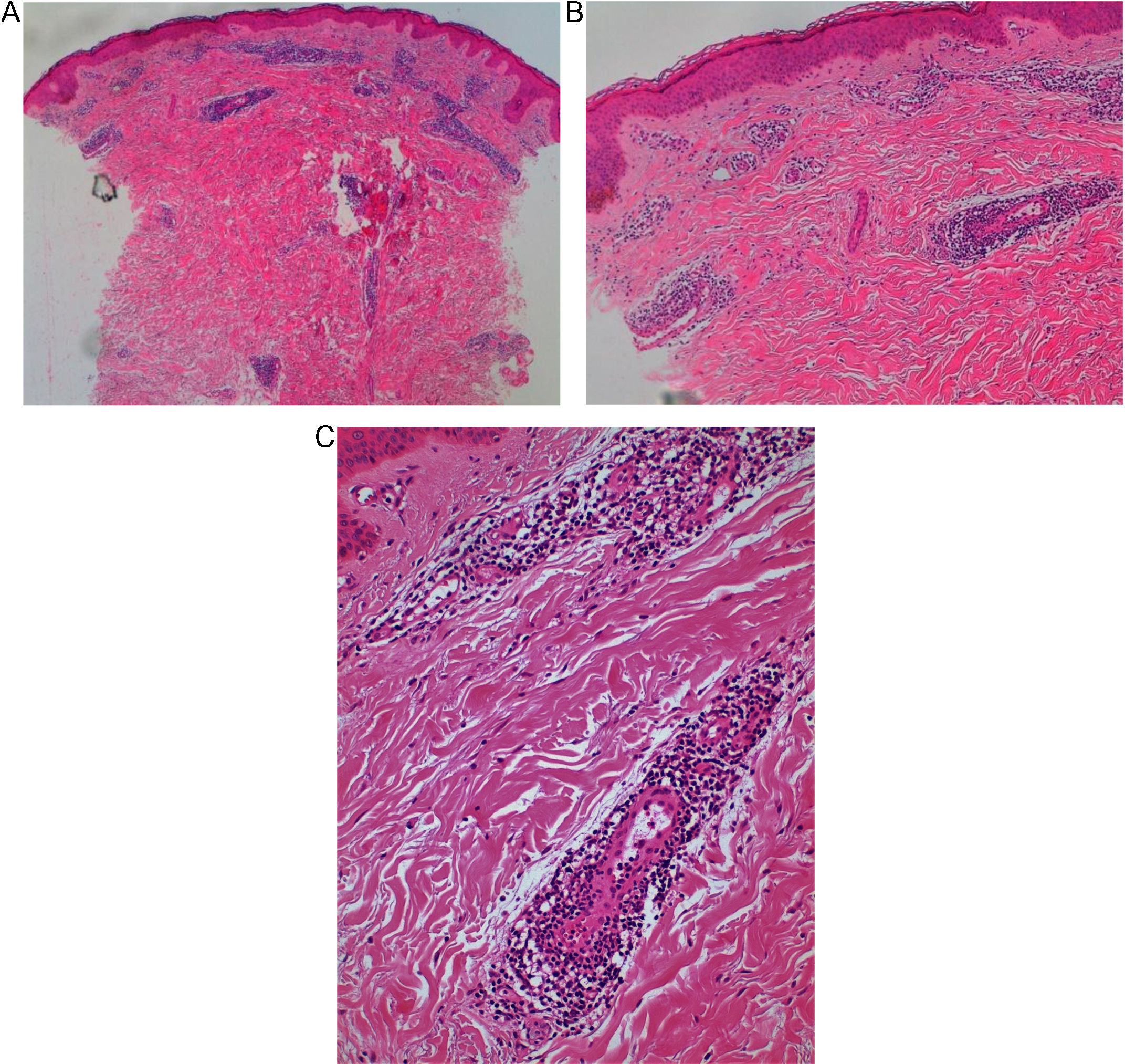
Histopathologic examination of skin lesions biopsy showed a perivascular lymphocytic infiltrate in the superficial and deep dermis, suggestive of erythema annulare centrifugum (EAC), based on the correlation between clinical and histological findings (Fig. 2) on hematoxylin and eosin stain. Periodic acid-Schiff and Pearls colorations did not show remarkable findings.
Laboratory tests detected thrombocytosis; negative viral hepatitis serology, negative HIV, CMV and EBV serology; negative alfa fetoprotein; negative autoantibodies (ANA, anti-sDNA, antiphopholipid); undetected rheumatoid factor; normal levels of protein C, S, antithrombin II and homocysteine, no resistance to activate protein C. The search for prothrombin G20210A mutation was negative.
Doppler ultrasonography and computed tomography examination revealed thrombosis of the sus-hepatic veins and portal hypertension with the diagnostic of Budd Chiari-Syndrome (BCS). Further investigation led to the diagnosis of essential thrombocythemia (ET) JAK2 negative, confirmed by bone marrow examination.
Despite anticoagulation and optimized diuretic therapy, renal function worsened and ascites persisted, and the patient was proposed for liver transplantation. Few weeks after transplantation, spontaneous resolution of cutaneous lesions was noticed, without relapse during 2 years of follow-up. Concerning her hematologic disease, she has been treated with hydroxyurea, however with poor results.
DiscussionErythema annulare centrifugum (EAC) is a rare inflammatory skin disease presenting with erythematous papules or plaques that expand centrifugally with central clearing resulting in an annular shape.1,2 There are two types, superficial and deep, but this classification is not completely accepted and according to some authors the designation EAC should be reserved for the superficial type only.3
EAC has been considered a hypersensitivity reaction, rather than a specific clinicopathologic entity.4 When a trigger is identified, the treatment of the underlying condition mostly results in spontaneous resolution of the skin lesions.5 EAC has been associated with many different entities, including infections, malignant neoplasms,6 various autoimmune diseases2,3,7 and drugs,8 but its association with BCS or liver failure had not been previously described.
BCS is a rare vascular liver disease resulting from the obstruction of the hepatic venous outflow tract that can result in liver failure.9 The most common underlying prothrombotic risk factor is a myeloproliferative disorder as ET, although it is now recognized that almost half of patients have multiple underlying prothrombotic risk factors.10 Some chemical mediators released from activated platelets could explain some cutaneous findings associated with thrombocytosis such as erythromelalgia, acute febril neutrophilic dermatosis and arterial thrombotic diseases11 but not EAC.
In our case, the skin lesion resolved without recurrence after liver transplantation. On the other hand, there was not an haematological improvement despite preconized therapy making the association between EAC and BCS/liver disease more likely than with ET.
To the best of our knowledge, we report the first case of EAC probably associated with BCS in a patient with ET. Our report shows a new association of EAC with a systemic disease, thus emphasizing the importance of clinical and complementary evaluation in a patient with EAC, as well as the importance of more studies to clarify the physiopathology of this clinical identity.
Please cite this article as: Borges AS, Brasileiro A, Santos S, Saiote J. Eritema anular centrífugo en un paciente con síndrome de Budd-Chiari. Actas Dermosifiliogr. 2018;109:755–757.