Epidermal effacement, also known as consumption of the epidermis, is a histologic feature that can be seen in a number of malignant melanomas.1–4 It consists of the thinning or disappearance of epidermal cell layers overlying the melanoma.1,2 Hantschke et al1 found epidermal effacement in 88 (86%) of 102 melanomas but in only 12 (9.6%) of 125 Spitz nevi. They also studied 61 spitzoid lesions without a clear diagnosis using genomic hybridization techniques and found epidermal effacement in 6 (14%) of 42 lesions that were reclassified as benign lesions and in 14 (74%) of 19 lesions that were reclassified as malignant lesions. Walters et al2 found epidermal effacement in 92 (43%) of 213 melanomas but in just 4 (4.2%) of 94 melanomas in situ or high-grade dysplastic nevi. There was no effacement in 146 benign nevi (114 low-grade dysplastic nevi, 8 congenital nevi, and 24 common nevi). In other words, epidermal effacement could be used, with caution, as a diagnostic criterion for differentiating melanoma from Spitz nevus or dysplastic nevus.
Even though epidermal effacement is a relatively common finding in melanomas (found by Hantschke et al1 and Walters et al2 in 86% and 43% of cases, respectively), very few studies have analyzed it. Furthermore, we believe that this histologic feature is unfamiliar to the majority of dermatologists.
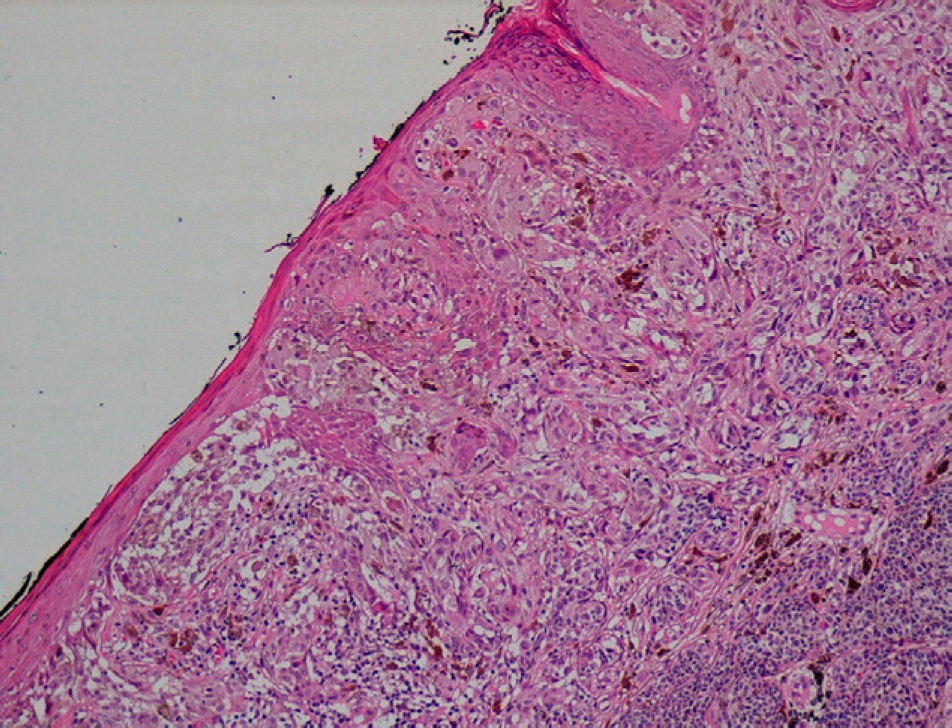
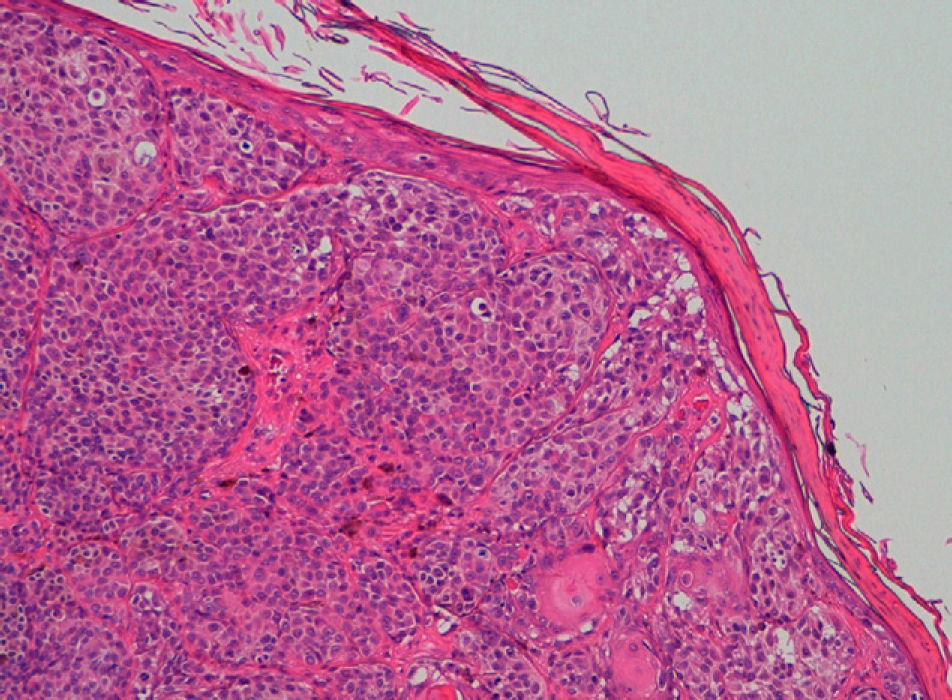
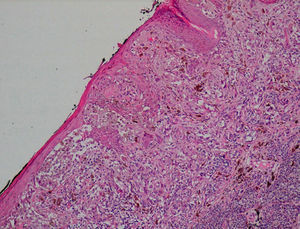
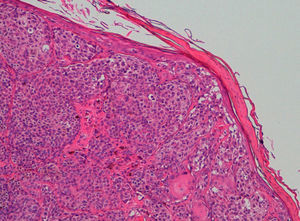
We recently saw 2 cases of malignant melanoma with epidermal effacement. The first was a superficial spreading melanoma (SSM), located on the right arm, that had entered the vertical growth phase (Breslow depth of 0.95mm and Clark level III) (Fig. 1). The second was also a SSM in the vertical growth phase (Breslow depth of 1.87mm and Clark level IV) but located on the abdomen (Fig. 2). The tumors had been removed from a 51-year-old and a 50-year-old man, respectively.
It has been postulated that epidermal effacement is the result of an autoimmune or immunologic process as this histologic feature has also been seen in certain halo nevi (pseudo-epidermal effacement).1–3 Walters et al2 do not believe this to be the case as they found no association between epidermal effacement and either tumor regression or inflammatory infiltrates. It might also be a physical phenomenon related to the compression caused by tumor growth1–3; this, however, would not explain why epidermal effacement is found in some thin melanomas (with a low Breslow depth) or indeed why it is not found in the vast majority of thick melanomas. Epidermal effacement has also been seen in areas adjacent to melanoma ulceration as well as in association with fissures, clefting, and areas of dermal-epidermal separation, explaining why numerous studies have suggested that this histologic feature might be a marker of subsequent progression to ulceration.1–4 In support of this theory, we have seen epidermal effacement in several epidermotropic metastatic melanomas.
Further studies are necessary to determine whether epidermal effacement, like ulceration, is associated with poorer prognosis in melanoma.5,6 Moreover, epidermal effacement is observed more frequently in association with other indicators of poorer prognosis in malignant melanomas5,6: increasing Breslow depth, number of mitoses per field, ulceration, and vertical growth.2 Until it is determined whether or not epidermal effacement, like ulceration, is associated with poorer prognosis, we believe that it should be included in protocols for melanoma histopathology reports.7 It is also interesting to note that paratumoral epidermal hyperplasia, which is precisely the opposite of epidermal effacement, located in zones adjacent to melanoma is associated with better prognosis in thick melanomas.8
The question remains as to why epidermal effacement and ulceration occur in certain malignant melanomas independently of tumor duration, Breslow depth, or faster growth. Epidermal effacement (and therefore subsequent ulceration) might be caused by the action of metalloproteases or the alteration of certain calcium-dependent adhesion molecules such as E-cadherin.2,3,9,10
Please cite this article as: Corbalán-Vélez R, et al. Adelgazamiento epidérmico en melanomas malignos. Actas Dermosifiliogr.2011;102:634-5.