Aplasia cutis congenita (ACC) is a rare congenital malformation. Membranous ACC is the most common of the 9 subtypes described. Its clinical presentation is highly variable, with appearances ranging from eroded, ulcerated, or scar-like lesions to a glistening surface. The differential diagnosis is broad, and clinical diagnosis can be challenging. Dermoscopy may be a useful tool for the differential diagnosis, but few studies have analyzed its use in this setting.1,2 We describe the dermoscopic findings of membranous ACC in an infant.
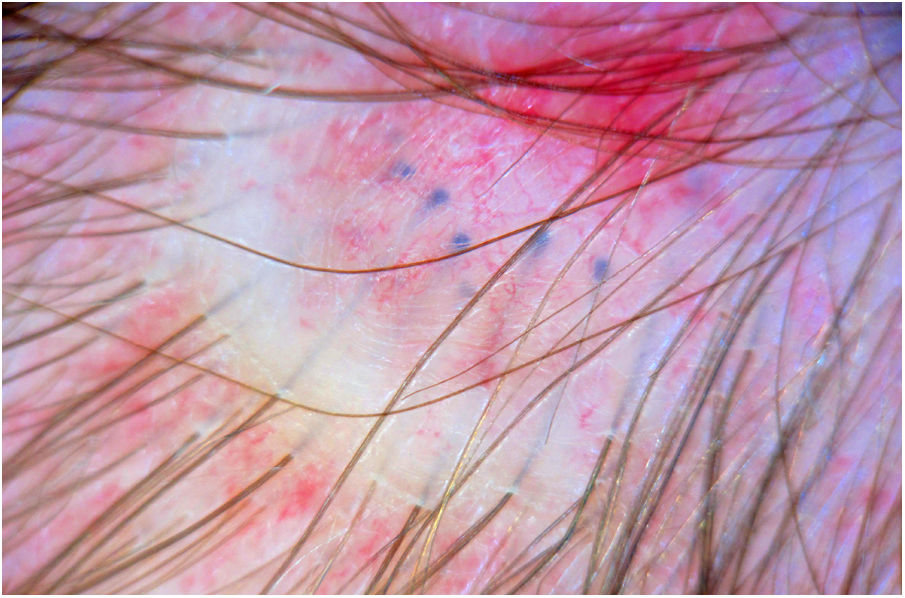
The infant was a 2-month-old boy with no remarkable personal or family history who was seen for a painful alopecic plaque on the vertex of his scalp. His parents reported that the plaque had appeared 3 weeks earlier following the use of a very rigid baby chair. They had applied disinfectants and healing creams, but there had been no clinical response. Physical examination showed a nonscaling erythematous alopecic plaque with a diameter of 8 mm that did not change on palpation (Fig. 1). Dermoscopy showed a shiny surface with thin telangiectatic vessels and bluish globules (Fig. 2). A diagnosis of membranous ACC was established. Transfontanellar ultrasound showed no underlying bone or brain defects. The parents were informed of the benign nature of the lesion. No specific treatment was prescribed.
ACC is a congenital condition characterized by absence of the epidermis, dermis, and, occasionally, bone or dura mater. It is mostly observed on the scalp, especially on the vertex or parietal scalp. The defects are usually small (typically 1−2 cm), although large lesions have been described. ACC has been linked to a number of causes, including use of certain medications or drugs during pregnancy and embryologic malformations. The hair collar sign, a potential marker of neural tube defects, may be observed.3 Transfontanellar ultrasound is recommended to rule out underlying bone or brain defects.
Because the lesions are so small, as occurred in our case, they can go unnoticed during the neonatal period, making clinical diagnosis even more challenging. Dermoscopy can be very useful for ruling out trauma or infectious (herpes virus, mycosis, impetigo), inflammatory (alopecia areata), or tumoral (sebaceous nevus) causes.4 The translucency sign is a characteristic dermoscopic feature of membranous ACC. It consists of the presence of a shiny surface, thin arborizing vessels, and blue globules corresponding to hair bulbs.1,5,6 Other possible features are an absence of follicular openings on the alopecic plaque and the hair collar sign (hair follicles distributed around the edge of the plaque). These features are quite specific to ACC and help establish a clinical diagnosis.1,2 Findings for sebaceous nevi include yellow lobules or dots not related to hair follicles. In tinea capitis, findings include corkscrew hairs, comma hairs, zigzag hairs, pigtail hairs, and Morse code–like hairs. Features of alopecia areata, which is very uncommon in neonates and infants, are yellow and black dots, exclamation mark hairs, and vellus hair. Triangular alopecia, in turn, is characterized by short, upright regrowing hairs, vellus hairs, and pigtail hairs.4 The dermoscopic features of diseases with focal alopecia in neonates and infants are summarized in Table 1.
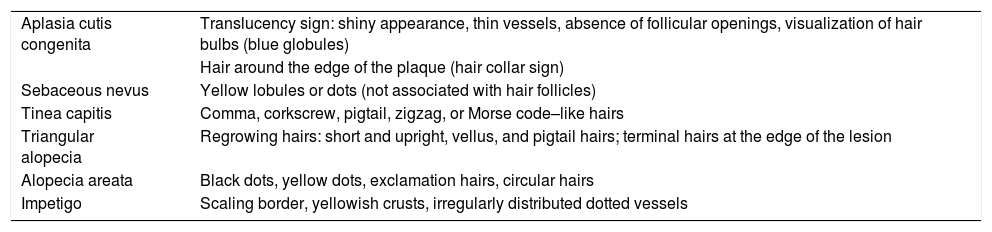
Dermoscopic Features of Diseases That Manifest With Alopecic Plaques in Neonates or Infants.
| Aplasia cutis congenita | Translucency sign: shiny appearance, thin vessels, absence of follicular openings, visualization of hair bulbs (blue globules) |
| Hair around the edge of the plaque (hair collar sign) | |
| Sebaceous nevus | Yellow lobules or dots (not associated with hair follicles) |
| Tinea capitis | Comma, corkscrew, pigtail, zigzag, or Morse code–like hairs |
| Triangular alopecia | Regrowing hairs: short and upright, vellus, and pigtail hairs; terminal hairs at the edge of the lesion |
| Alopecia areata | Black dots, yellow dots, exclamation hairs, circular hairs |
| Impetigo | Scaling border, yellowish crusts, irregularly distributed dotted vessels |
High-frequency ultrasound can also be useful in membranous ACC, as it shows a thin or concave hyperechogenic line corresponding to the epidermis and absence of the dermis or subcutaneous tissue; it can also be used to assess bone status.7.
Dermoscopy may be a useful diagnostic tool for membranous ACC as it helps rule out trauma, infections, inflammatory disorders, and tumors and may avoid the need for invasive diagnostic tests.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Morgado-Carrasco D, Fustà-Novell X. Hallazgos dermatoscópicos en la aplasia cutis membranosa. Diagnóstico diferencial con otras formas de alopecia focal en lactantes. Actas Dermosifiliogr. 2021;112:275–277.