Several cutaneous manifestations are occasionally observed in patients with inflammatory bowel disease (IBD); however, isolated cutaneous vasculitis is rare among those skin lesions. Both cutaneous small-vessel vasculitis and cutaneous polyarteritis nodosa (cPAN) are uncommon skin manifestations of IBD.1 We present herein a case of cPAN in a patient with ulcerative colitis (UC).
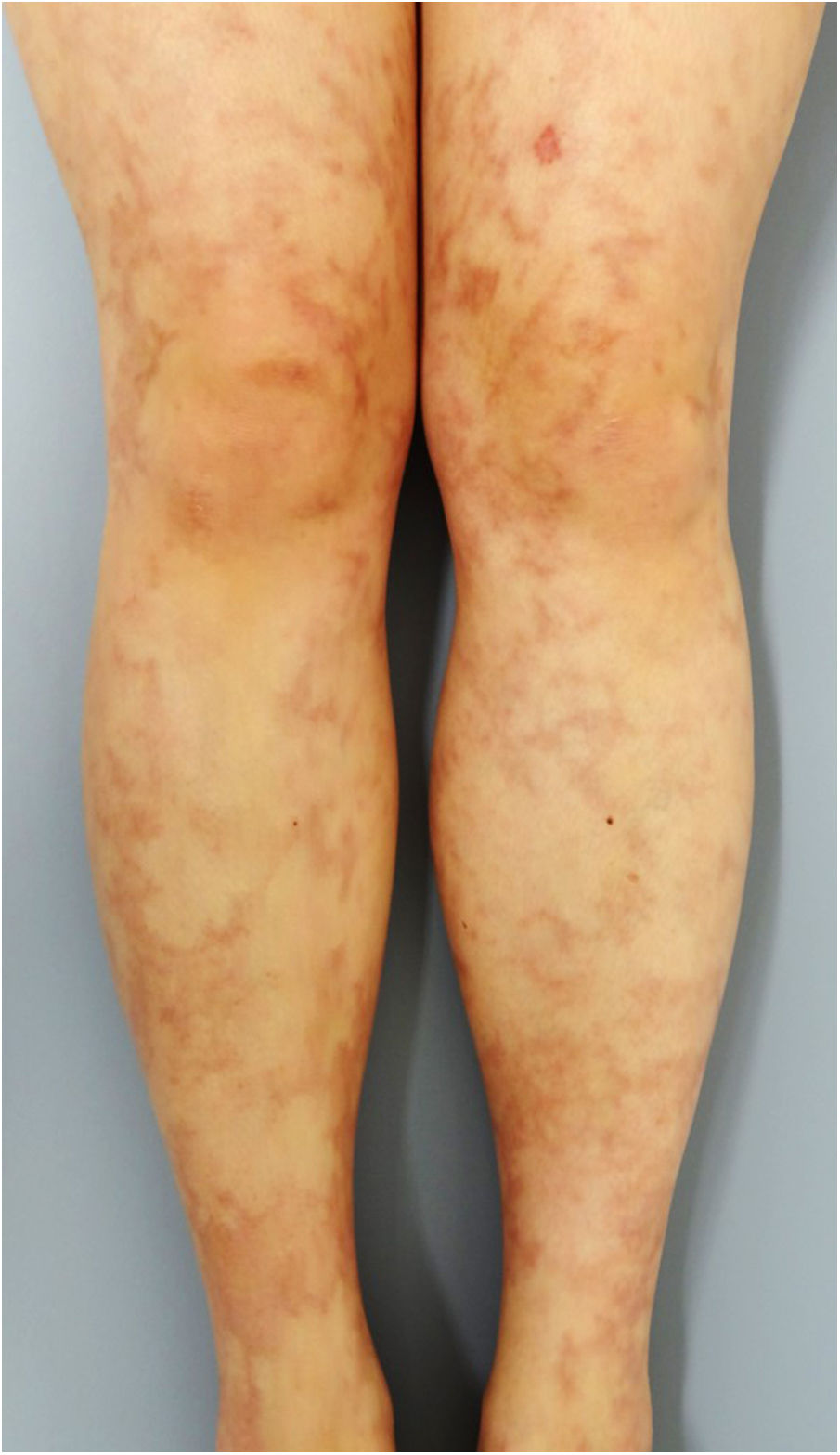
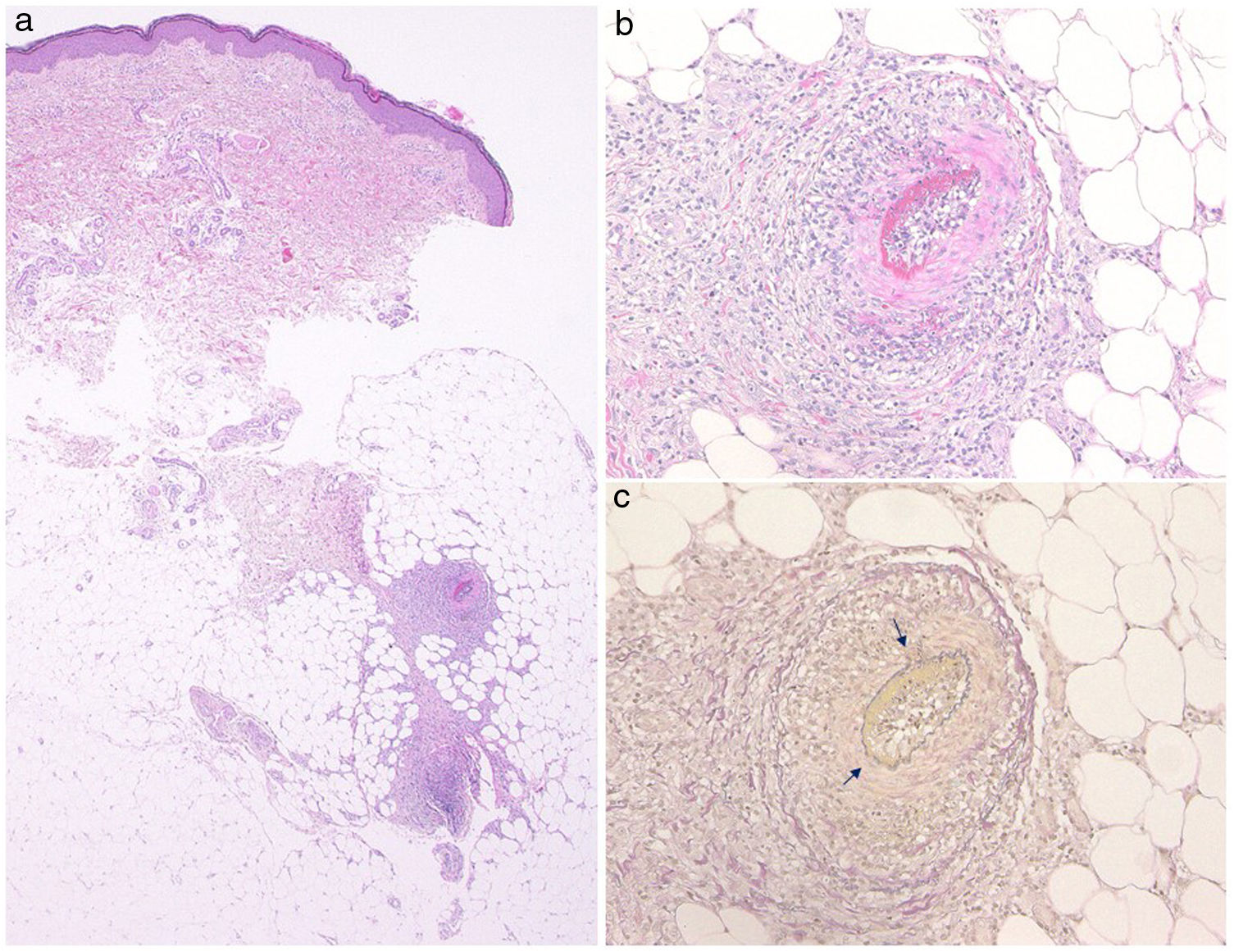
A 33-year-old woman visited the dermatology clinic complaining of erythemas with tenderness on the bilateral lower extremities with numbness, which had appeared three months previously. She had been suffering from UC (pancolitis type) for 2.5 years, and had been treated with mesalazine (5-aminosalicylic acid). Intestinal conditions were well-controlled. Physical examination showed livedo racemosa with tender nodules involving the anterior and posterior aspects of both legs, abdomen, and forearms (Fig. 1). Laboratory data showed normal liver and renal function, and urinalysis was normal. Serum levels of C-reactive protein, complements, IgG, and rheumatoid factor were all within normal ranges, and antinuclear antibody, antineutrophil cytoplasmic autoantibodies (MPO-ANCA, PR3-ANCA), anticardiolipin, and anti-β2-glycoprotein 1 IgG antibody were all negative. Cryoglobulin was not detected. A biopsy specimen showed necrotizing vasculitis in the lower dermis without affecting neighboring tissues (Fig. 2a). Higher magnification revealed a crescent fibrinoid deposition in the vessel lumen infiltrated by neutrophils and lymphocytes (Fig. 2b). Perivascular inflammation was localized at the dermal-subcutis junction. Elastica van Gieson stain revealed partially disrupted internal elastic lamina (Fig. 2c). The patient was treated with low-dose prednisolone (up to 30 mg/day (0.6 mg/kg)), sarpogrelate hydrochloride (300 mg/day), and tocopherol nicotinate (300 mg/day); however, the numbness was resistant to therapy. Mini-pulse therapy (methylprednisolone 500 mg/day for 3 consecutive days) was effective for her numbness, which, however, relapsed after the discontinuation of medication because of pregnancy. Antiplatelet agents and vitamin E were re-started after delivery; however, she refused oral steroid therapy. Her numbness still remains.
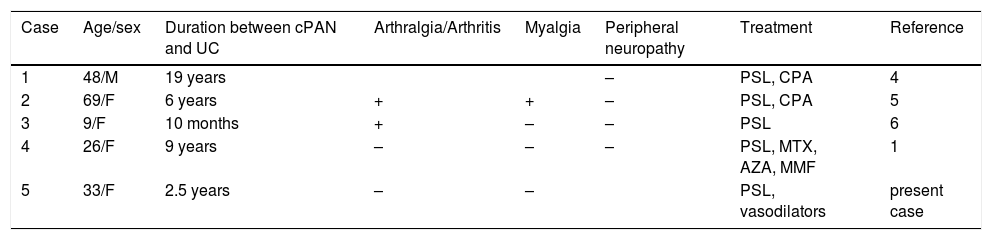
The presented case developed small-sized arteritis (150 μm in diameter) at the dermo-subcutaneous junction. Elastica van Gieson stain revealed the arteritis, and vasculitis did not involve venous vessels. ANCA was negative, and detailed examination of the nose, respiratory tract, kidney and lung denied granulomatosis with polyangiitis and microscopic polyangiitis. Several triggers such as viral infection and drugs, or systemic diseases are occasionally associated with cPAN. Leukocytoclastic vasculitis associated with IBD is suggested to be caused by circulating immune complex.2,3 Only several cases of cPAN associated with IBD have been reported to date; however, as compared with Crohn’s disease, cases of UC are rarely reported. The reason why cases of UC are significantly fewer as compared with those of Crohn’s disease is currently unknown. To our knowledge, only five cases of UC have been reported to coexist with cPAN including the present case1,4–6 (Table 1). The patients consisted of one male and four females. All of the patients except one were diagnosed with UC prior to the onset of cPAN, and the interval between the diagnoses of UC and cPAN varied between 10 months and 19 years. Cutaneous manifestations presented with macular rash, erythematous nodules, and livedo racemosa. Other systemic symptoms were arthritis/arthralgia (n = 3), myalgia (n = 2), and peripheral neuropathy (n = 1). By contrast, cPAN did not develop in parallel with worsening of intestinal conditions. The patients were treated with methylprednisolone pulse therapy, oral prednisolone, immunosuppressant (cyclophosphamide, methotrexate, azathioprine, mycophenolate mofetil), vasodilators, and antiplatelet agents. During the follow-up period, one case relapsed.4 In the present case, we could follow our patient for over four years, and her numbness did not perfectly disappear. The shared pathogenesis of both disorders has been speculated such as abnormal immune response to some specific pathogen, an immune complex etiology, or hypercoagulable states; however, the precise mechanism remains uncertain because the number of reported cases of the association of cPAN and UC is limited. Nevertheless, it should be kept in mind that IBD is a rare systemic disease in patients with cPAN. Moreover, clinicians should become aware of cutaneous vasculitis in patients with IBD, in addition to pyoderma gangrenosum or erythema nodosum.
Cases of coexistence with cPAN and UC.
| Case | Age/sex | Duration between cPAN and UC | Arthralgia/Arthritis | Myalgia | Peripheral neuropathy | Treatment | Reference |
|---|---|---|---|---|---|---|---|
| 1 | 48/M | 19 years | + | + | – | PSL, CPA | 4 |
| 2 | 69/F | 6 years | + | + | – | PSL, CPA | 5 |
| 3 | 9/F | 10 months | + | – | – | PSL | 6 |
| 4 | 26/F | 9 years | – | – | – | PSL, MTX, AZA, MMF | 1 |
| 5 | 33/F | 2.5 years | – | – | + | PSL, vasodilators | present case |
PSL: prednisolone, CPA; cyclophosphamide, MTX; methotrexate, AZA azathioprine, MMF; mycophenolate mofetil.
Please cite this article as: Hiraiwa T, Yamamoto T. Poliarteritis nudosa cutánea en un paciente con colitis ulcerosa. Actas Dermosifiliogr. 2020. https://doi.org/10.1016/j.ad.2019.02.023