Cutaneous collagenous vasculopathy (CCV) is an idiopathic microangiopathy affecting blood vessels of the superficial dermal vascular plexus.1,2 It is a rare condition characterized by the appearance of multiple cutaneous telangiectasias with a variable distribution on the trunk and limbs, but it does not affect the mucosas or nail bed and has not been associated with systemic repercussions in the cases reported in the literature.3–5 CCV shows marked clinical similarities with generalized essential telangiectasia, which is the main clinical differential diagnosis to be considered.1,4 Since its first description in the year 2000 by Salama and Rosenthal1 and up to the year 2015, we have found reports of 28 new cases of CCV (Table 1). We present a patient recently diagnosed with CCV in our department.
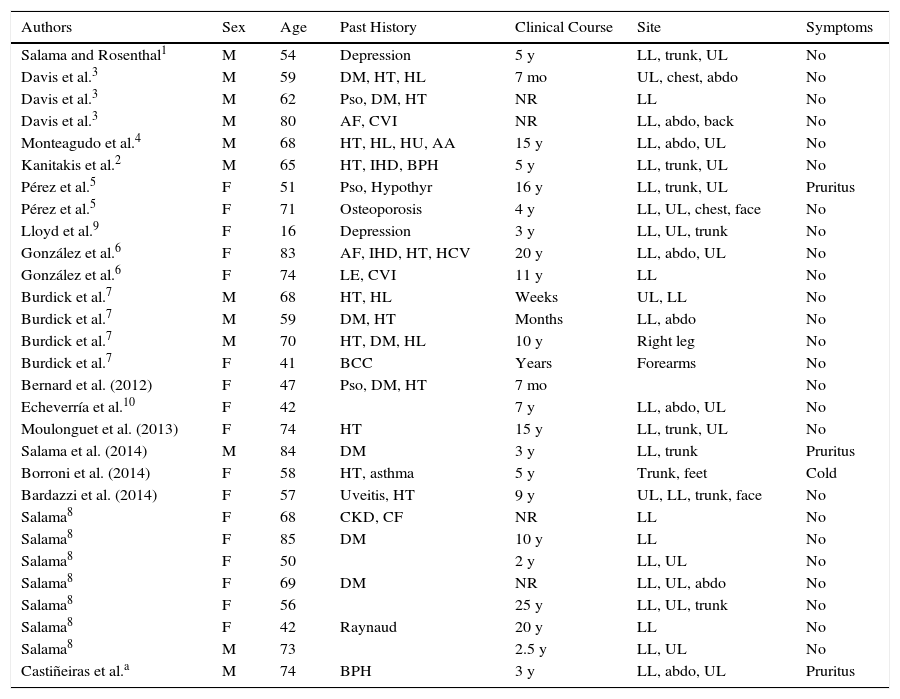
Cases of Cutaneous Collagenous Vasculopathy.
| Authors | Sex | Age | Past History | Clinical Course | Site | Symptoms |
|---|---|---|---|---|---|---|
| Salama and Rosenthal1 | M | 54 | Depression | 5 y | LL, trunk, UL | No |
| Davis et al.3 | M | 59 | DM, HT, HL | 7 mo | UL, chest, abdo | No |
| Davis et al.3 | M | 62 | Pso, DM, HT | NR | LL | No |
| Davis et al.3 | M | 80 | AF, CVI | NR | LL, abdo, back | No |
| Monteagudo et al.4 | M | 68 | HT, HL, HU, AA | 15 y | LL, abdo, UL | No |
| Kanitakis et al.2 | M | 65 | HT, IHD, BPH | 5 y | LL, trunk, UL | No |
| Pérez et al.5 | F | 51 | Pso, Hypothyr | 16 y | LL, trunk, UL | Pruritus |
| Pérez et al.5 | F | 71 | Osteoporosis | 4 y | LL, UL, chest, face | No |
| Lloyd et al.9 | F | 16 | Depression | 3 y | LL, UL, trunk | No |
| González et al.6 | F | 83 | AF, IHD, HT, HCV | 20 y | LL, abdo, UL | No |
| González et al.6 | F | 74 | LE, CVI | 11 y | LL | No |
| Burdick et al.7 | M | 68 | HT, HL | Weeks | UL, LL | No |
| Burdick et al.7 | M | 59 | DM, HT | Months | LL, abdo | No |
| Burdick et al.7 | M | 70 | HT, DM, HL | 10 y | Right leg | No |
| Burdick et al.7 | F | 41 | BCC | Years | Forearms | No |
| Bernard et al. (2012) | F | 47 | Pso, DM, HT | 7 mo | No | |
| Echeverría et al.10 | F | 42 | 7 y | LL, abdo, UL | No | |
| Moulonguet et al. (2013) | F | 74 | HT | 15 y | LL, trunk, UL | No |
| Salama et al. (2014) | M | 84 | DM | 3 y | LL, trunk | Pruritus |
| Borroni et al. (2014) | F | 58 | HT, asthma | 5 y | Trunk, feet | Cold |
| Bardazzi et al. (2014) | F | 57 | Uveitis, HT | 9 y | UL, LL, trunk, face | No |
| Salama8 | F | 68 | CKD, CF | NR | LL | No |
| Salama8 | F | 85 | DM | 10 y | LL | No |
| Salama8 | F | 50 | 2 y | LL, UL | No | |
| Salama8 | F | 69 | DM | NR | LL, UL, abdo | No |
| Salama8 | F | 56 | 25 y | LL, UL, trunk | No | |
| Salama8 | F | 42 | Raynaud | 20 y | LL | No |
| Salama8 | M | 73 | 2.5 y | LL, UL | No | |
| Castiñeiras et al.a | M | 74 | BPH | 3 y | LL, abdo, UL | Pruritus |
Abbreviations: AA, alopecia areata; abdo, abdomen; AF, atrial fibrillation; BCC, basal cell carcinoma; BPH, benign prostatic hyperplasia; CF, cryofibrinogenemia; CKD, chronic kidney disease; CVI, chronic venous insufficiency; DM, diabetes mellitus; F, female; HCV, Hepatitis C virus infection; HL, hyperlipidemia; HT, hypertension; HU, hyperuricemia; Hypothyr, hypothyroidism; IHD, ischemic heart disease; LE, lupus erythematosus; LL, lower limbs; M, male; NR, not reported; PH, past history; Pso, psoriasis; UL, upper limbs.
The patient was a 74-year-old man with a past history of adenoma of the prostate. He was on no long-term treatment. He was seen in our department for evaluation of reddish skin lesions that had developed progressively over the previous 3 years. The telangiectasias had first appeared on the lower limbs and, over the course of a few years, had spread to the abdomen and to the forearms. The patient reported occasional pruritus. There was no personal or family history of widespread cutaneous telangiectasias or of mucosal bleeding. Physical examination revealed erythematous plaques formed of multiple telangiectatic vessels; the plaques were distributed symmetrically over the forearms (Fig. 1A), lower abdomen, thighs (Fig. 1B), and lower legs (Fig. 1C). There were no mucosal or nail bed alterations.
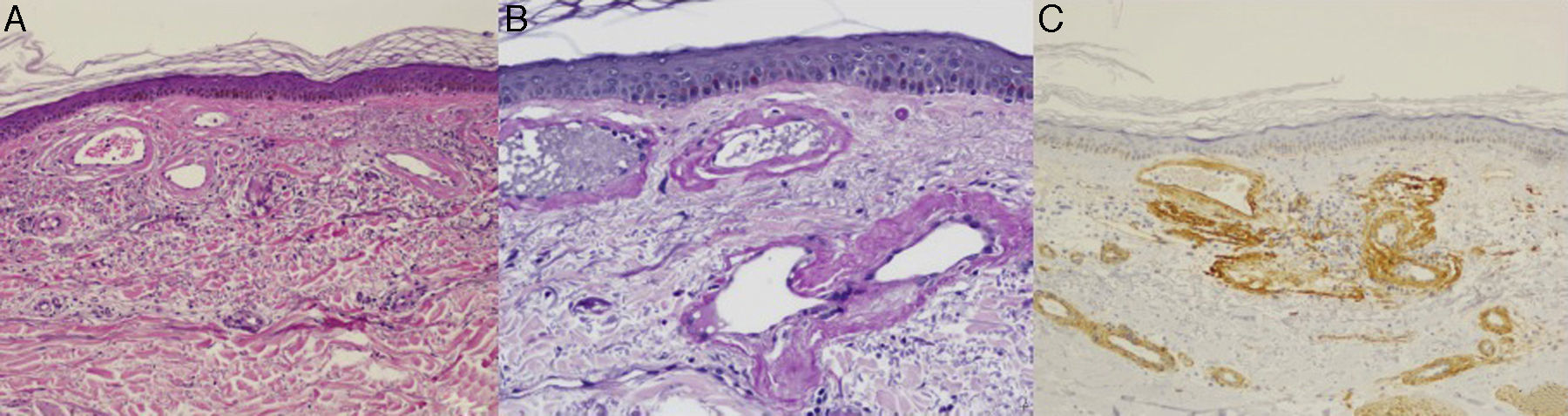
On a suspicion of generalized essential telangiectasia or CCV, a biopsy was taken from a lesion on the abdomen. Histopathology showed dilated small-caliber vascular lumina in the papillary dermis (Fig. 2A) with walls thickened by perivascular deposits of an amorphous hyaline material that stained positive with periodic acid Schiff-diastase (Fig. 2B) but negative with Congo red; immune staining was positive for type iv collagen (Fig. 2C).
A, Dilated blood vessels with an irregular outline and thickened walls in the papillary dermis. Hematoxylin-eosin, original magnification ×40). B, Deposits of a homogeneous, eosinophilic, periodic acid-Schiff (PAS)-positive material around the vessel lumina. PAS-diastase, original magnification ×100).C, Immune staining of these same deposits was positive for type iv collagen.
Additional tests including complete blood count, biochemistry, rheumatoid factor, C-reactive protein, erythrocyte sedimentation rate, coagulation studies, antinuclear antibodies, complement fractions C3 and C4, and thyroid function were normal or negative. Protein electrophoresis detected a k-type immunoglobulin G monoclonal gammopathy of undetermined significance, for which the patient was referred to the hematology department for study and follow-up.
A diagnosis of CCV was made. The patient rejected laser treatment.
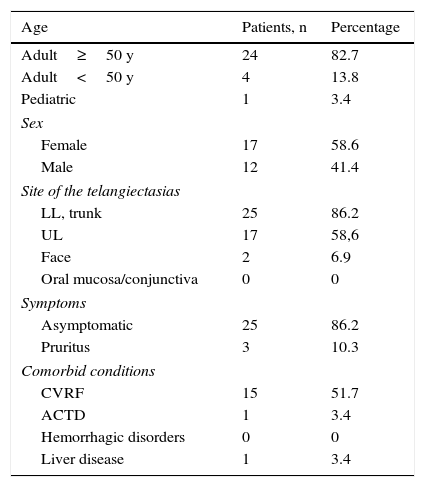
CCV is a rare disease characterized by the appearance of widespread cutaneous telangiectasias that often first arise on the lower limbs and progressively spread to the rest of the body.6 Cases reported in the literature did not show involvement of the oral mucosa or conjunctiva.7,8 The disease affects adults, with no difference between the sexes, with a mean age at onset of 62 years (range, 41-85 years); a single case has been reported in a pediatric patient aged 16 years.9 Some patients report occasional pruritus, but the condition is usually asymptomatic. No familial cases have been reported to date, nor associated hemorrhagic disturbances (Table 2). Diagnosis relies on a good medical history, paying special attention to the distribution of the telangiectasias, age at onset, family history, symptoms, associated systemic disorders, and the drug history in patients on polypharmacy.8 The diagnosis is confirmed by histopathology, which shows the presence in the superficial dermis of dilated blood vessels with walls thickened by perivascular deposits of an eosinophilic hyaline material that shows type iv collagen immunoreactivity.7,8 The etiology and pathogenesis of CCV are unknown. It has been suggested that CCV may be a primary disease due to a genetic defect that alters collagen synthesis in the cutaneous microvasculature, or that the perivascular fibrosis is a repair process in response to damage to the cutaneous microvasculature.6,8
Clinical Characteristics of Patients With Cutaneous Collagenous Vasculopathy.
| Age | Patients, n | Percentage |
|---|---|---|
| Adult≥50 y | 24 | 82.7 |
| Adult<50 y | 4 | 13.8 |
| Pediatric | 1 | 3.4 |
| Sex | ||
| Female | 17 | 58.6 |
| Male | 12 | 41.4 |
| Site of the telangiectasias | ||
| LL, trunk | 25 | 86.2 |
| UL | 17 | 58,6 |
| Face | 2 | 6.9 |
| Oral mucosa/conjunctiva | 0 | 0 |
| Symptoms | ||
| Asymptomatic | 25 | 86.2 |
| Pruritus | 3 | 10.3 |
| Comorbid conditions | ||
| CVRF | 15 | 51.7 |
| ACTD | 1 | 3.4 |
| Hemorrhagic disorders | 0 | 0 |
| Liver disease | 1 | 3.4 |
Abbreviations: ACTD, autoimmune connective tissue disease; CVRF, cardiovascular risk factors; LL, lower limbs; UL, upper limbs.
In the majority of reported cases of CCV, patients were not treated or this was not specified. Although this is an asymptomatic condition and is not associated with other diseases or complications, it can have important cosmetic and psychologic repercussions. As with other diseases that cause telangiectasias, laser systems can be an effective therapeutic option; pulsed dye laser can achieve a marked improvement in the lesions.10
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Castiñeiras-Mato I, Rodríguez-Lojo R, Fernández-Díaz ML, Bal-Nieves F. Cutaneous Collagenous Vasculopathy: A Case Report and Review of the Literature. Actas Dermosifiliogr. 2016;107:444–447.