Wheat flour proteins are composed of a complex mix of soluble proteins (albumin and globulin) and insoluble structural proteins. The latter are divided into gliadins, which are monomeric, and glutenins, which are polymeric. Gluten is composed of both these types of protein and is widely used in both modified and unmodified forms in industry. The most important modification of gluten is hydrolysis.1
Hydrolyzed wheat protein is used in cosmetic products for its hydrating properties.2 Cosmetics containing this protein can lead to infrequent—but occasionally severe—allergic reactions, and both urticaria1,3–7 and allergic contact eczema2,8–10 have been reported.
Cutaneous contact reactions to proteins are clinically relevant disorders of which the dermatologist should be aware, since, in some cases, they can indicate occupational disease, especially in individuals who handle food.11
A 23-year-old man with no history of atopy was referred from the allergology department with a rash that started immediately after application of Contrôle-Jeunesse face cream (Kiotis). The rash involved highly pruritic wheals affecting the face and neck accompanied by bilateral palpebral edema (Fig. 1). Labial edema and systemic symptoms did not develop. He attended the emergency department, where he was prescribed oral cetirizine (10mg); symptoms resolved completely in 24hours. The patient reported having experienced a similar reaction the previous summer after using a house brand sunscreen, although he did not consult for it. He did not report food-induced symptoms or intolerance.
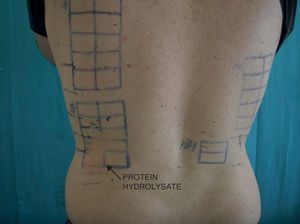
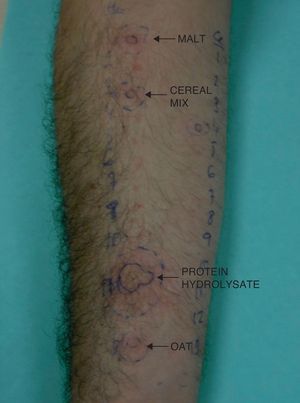
The result of a nonblinded skin test with his cream was negative. Patch testing was then performed with the True Test panel, a cosmetics panel (Chemotechnique Diagnostics), and the patient's own products. Readings were positive (++) to the patient's own Contrôle-Jeunesse cream at 48hours and 96hours; all other readings were negative. The results of patch testing with the individual components of the cream (supplied by the manufacturer) were positive (++) for hydrolyzed wheat protein at 1% in water at 48 and 96hours (Fig. 2). We performed 10 tests on controls using hydrolyzed protein at 1%; all the results were negative. The patient was referred back to the allergology department, where he underwent prick tests with flours and cereals (Leti, Diater, Stallergènes, and Aristegui). The results were as follows: malt, positive (5×4mm); cereal mix, positive (7×5mm); oats, positive (5×5mm); hydrolyzed wheat extract (18×14mm) (Fig. 3). Total immunoglobulin (Ig) E was 136U/mL (reference range, 1-100 U/mL); the results of specific IgE testing with buckwheat, rice, oats, barley, rye, corn, common millet, soy, and wheat were negative.
Hydrolyzed proteins are added to cosmetic products for their emollient properties. After the bovine spongiform encephalopathy epidemic, animal proteins such as collagen, keratin, and elastin began to be replaced by vegetable proteins such as almond, wheat, and soy.4
Contact urticaria induced by cosmetics is uncommon, although reports of cases caused by the proteins contained in cosmetics are increasing in frequency. The first cases were reported in 1998 and involved hairdressers affected by contact urticaria induced by hair conditioners. The culprit allergen was hydrolyzed collagen protein.6 These reports were followed by new cases involving reactions to hydrolyzed wheat protein, presenting as dermatitis2,8–10 or contact urticaria.1,3,5–7 The mechanism by which the same agent can cause one type of reaction or another is unknown. Contact urticaria is usually localized, although some cases involve more severe symptoms such as angioedema, generalized urticaria, bronchospasm, or even anaphylaxis.1,6 It should be noted that most of these patients were able to tolerate wheat-derived foods, as in our case, although some patients reacted to foods containing the hydrolyzed protein. The reason for this finding seems to be that hydrolysis entails the appearance of new epitopes, which are responsible for the allergic reaction.1
We present a new case in order to make this disease more widely known and to help direct the patient towards appropriate diagnostic tests.
We stress the importance of performing patch tests using the patient's own products, since in cases such as ours, tests using standard panels could yield false-negative results. Diagnostic testing in patients with contact urticaria should be performed with the utmost caution and in a specialized center with full resuscitation facilities. The product should be applied first in an open test; if the result is negative, a prick test should be performed before the closed patch tests. Ours is the first reported case in which both patch tests and the prick test were positive, indicating that the same agent could cause both immediate and delayed hypersensitivity, thus explaining the occurrence of eczema and contact urticaria in the same patient.
Collaboration with the allergology department is important in order to detect sensitization or cross-reactivity with other cereals and thus prevent reactions to foods.
Please cite this article as: Barrientos N, Vázquez S, Domínguez JD. Urticaria de contacto a protein hidrolizada de trigo contenida en crema cosmética. Actas Dermosifiliogr.2012;103:750-752.