Skin manifestations of lupus erythematosus are varied. Some of them are atypical and may imitate benign skin diseases. Acneiform lesions are a rare, atypical form of presentation.
A 48-year-old woman visited our department with a lesion on the chin that had appeared 2 months earlier. The patient had initially been diagnosed with lupus erythematosus discoides and a subacute cutaneous lupus erythematosus that had appeared 16 years earlier and had been treated with hydroxychloroquine. Treatment was suspended due to maculopathy. Four years after diagnosis of the cutaneous lupus, the patient was finally diagnosed with systemic lupus erythematosus (SLE), as she met clinical and laboratory criteria (lupus discoides, synovitis, lupus nephritis, positive antinuclear antibody titer).
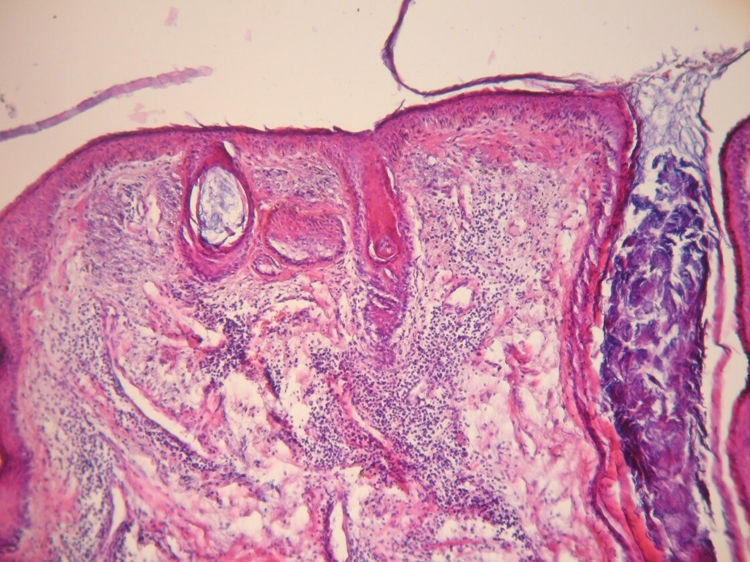
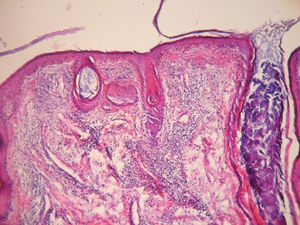
The physical examination revealed an infiltrated erythematous plaque with edematous edges, with some open comedones and milium cysts on the surface (Fig. 1). An incisional biopsy of the lesion was performed, and histology revealed a flattened epidermis with foci of vacuolization in the basement layer and thickening of the basement membrane, follicular dilations with keratotic plugs, and comedones. A perivascular and periadnexal inflammatory infiltrate was visible in the dermis (Fig. 2B).
Hematoxylin–eosin staining. Note the flattened epidermis with foci of vacuolization in the basement layer and thickening of the basement membrane, follicular dilations with keratotic plugs, and comedones. Perivascular and periadnexal inflammatory infiltrate in the dermis. With kind permission of Dr. A.C. Innocenti.
Given these findings and the patient’s history, the lesion was diagnosed as comedonic lupus. The patient initially underwent treatment with hydrocortisone, 0.1%, with little response, followed by minocycline (100 mg/d for 3 months) in association with tretinoin cream, 0.005%, with good results, showing clear improvement of the lesion and residual scarring.
Comedonic or comedonal lupus is a rare entity and a rare variant of chronic cutaneous lupus erythematosus. It is similar to other clinical entities such as acne, which can sometimes make diagnosis difficult.1,2 Very few cases have been reported in the medical literature and this disease is therefore thought to be underdiagnosed.1,3 Clinically, it is characterized by comedones on an erythematous plaque, mainly on seborrheic regions.4 The etiology is unknown.1,2 It has been suggested that exposure to sunlight may be involved in the formation of comedones. The solar damage may produce changes in the collagen of the normal skin, altering its structure and promoting retention of sebum, concluding in the formation of comedones, as occurs in Favre-Racouchot syndrome. The other theory put forward is that follicular plugs act as a factor that promotes the formation of comedones.5
Presentation typically occurs between the ages of 25 and 35 years, or even younger.1–3 The differential diagnosis should include inflammatory acne, Favre-Racouchot syndrome, milium cysts, inflammatory tinea, and nevus comedonicus.1
When comedones are absent, this disease may be called lupus with an acneiform scarring pattern. In this entity, the lesions are characterized by pitting, resulting from the destruction of the hair follicle and the sebaceous glands due to the inflammatory infiltrate.3,5–7
The diagnosis is confirmed by means of the histopathology study, which shows a predominant interphase pattern with hydropic degeneration of the basement layer and thickening of the basement membrane, accompanied by keratotic plugs and comedones, as reported in our patient.1–3 When histology findings are not conclusive, immunofluorescence may contribute to the diagnosis, revealing a deposit of IgM, IgG, and C3 at the dermal-epidermal junction.1,6
Several therapeutic options exist, although the treatment of choice is oral hydroxychloroquine (200 mg/12 h).1,7 In our case, hydroxychloroquine could not be administered due to the patient’s ophthalmologic history. Oral and topical retinoids may be used as an alternative and may be supplemented with topical or intralesional corticosteroids.1 It should be noted that these treatments presented little therapeutic efficacy in our patient and minocycline (100 mg/d for 3 months) and topical tretinoin, together with strict photoprotection, was indicated, with good results; we therefore propose this regimen as another alternative treatment. The outcome of comedonic lupus is uncertain and, while few patients have been described in the literature, a risk of progression to SLE has been observed in half of cases.1–3 It should be noted that our patient already presented systemic lupus when the comedonic lupus lesion appeared.
Comedonic lupus thus represents a rare presentation of chronic cutaneous lupus erythematous. Early diagnosis and long-term follow-up are very important due to the risk of systemic progression of the disease.
FundingThe authors state that they have received no external funding for this study.
Conflicts of InterestThe authors declares that they have no conflicts of interest.
Please cite this article as: Chessé C, Fernández-Tapia MJ, Borzotta F. Lupus comedónico: presentación inusual de lupus cutáneo. Actas Dermosifiliogr. 2021;112:370–371.