Acral lentiginous melanomas—the melanomas most commonly found on the distal portions of the limbs—have usually reached more advanced stages than other types of melanoma when diagnosed. Our aim was to describe the clinical presentation of these tumors.
Materials and methodsRetrospective, descriptive, observational study of cases recorded in the database of the Instituto Valenciano de Oncología. In telephone interviews the patients answered a questionnaire on the presenting features of the lesion, on the presence of signs and symptoms included in the Glasgow 7-point checklist and the ABCDEs of melanoma, and on diagnostic delay attributable to patient or physician.
ResultsIn the interviews with the 23 patients who responded to the questionnaire, we detected a diagnostic delay of more than 1 year attributable to the patient (delay in seeking care) in 30.4% of the cases. Diagnostic delay of more than 1 year attributable to the physician (failure to suspect the diagnosis) was identified in 20%. The most frequent reasons for consulting a physician about a lesion were changes in size, changes in color, bleeding, or failure to heal. In 20% of the cases the evaluating physician did not order histology for over a year.
ConclusionsDiagnostic delay is a significant problem in acral lentiginous melanoma and may be attributable either to patients or to physicians’ failure to recognize warning signs. Melanoma prevention campaigns should place more emphasis on the possibility of melanomas appearing on the palms and, particularly, on the soles.
El melanoma lentiginoso acral (MLA) es el tipo de melanoma de localización acral más frecuente y suele diagnosticarse en estadios más avanzados que el resto de tipos de melanoma.
El objetivo de nuestro estudio fue conocer las características de presentación clínica del MLA.
Material y métodosse realizó un estudio descriptivo observacional restrospectivo a partir de los pacientes recogidos en la base de datos del Instituto Valenciano de Oncología (IVO). Mediante encuestas telefónicas a los pacientes se recogieron las características de presentación de la lesión, en particular la presencia de los signos y síntomas incluidos en las reglas del ABCDE y de los siete puntos de Glasgow, así como el retraso en el diagnóstico atribuible al paciente o al médico.
Resultadosen una muestra final de 23 pacientes que pudieron responder finalmente a la encuesta se constató que el diagnóstico se demoró más de un año por un retraso en la consulta por parte del paciente en un 30,4%. Por otra parte, hubo una demora de más de un año atribuible al médico que no sospechó el diagnóstico en un 20% de los casos. Respecto a los motivos más frecuentes de consulta estos fueron: cambios en el tamaño, en el color, sangrado y herida que no cura. En un 20% de los casos que fueron evaluados por un médico la decisión de realizar el estudio histológico se demoró más de un año.
ConclusionesExiste un importante retraso en el diagnóstico del MLA debido tanto al paciente como al médico debido en parte a una falta de reconocimiento de los signos de alarma por parte del paciente y del personal sanitario.Las campañas preventivas del melanoma deberían hacer más énfasis en la posible afectación de las palmas y sobre todo de las plantas por parte del melanoma.
Cutaneous melanoma is a significant public health problem. The incidence of malignant melanoma has risen between 3% and 8% each year in Europe since the 1960s,1 and 18.6 years of potential life are lost on average for every death from this disease in the United States.2
The 4 main subtypes of melanoma are superficial spreading melanoma, lentigo maligna melanoma, nodular melanoma, and acral lentiginous melanoma (ALM). Some authors have found that 7% of all cutaneous melanomas are found at acral sites,1 and while all 4 subtypes are known to occur there, ALM is the most prevalent subtype in these locations. ALMs are found on the dorsal surfaces of hands and feet, on the palms and soles, on the wrists and heels, and under nails.3
Although the incidence of ALM seems to be similar in different racial groups, non-Caucasians seem to have proportionally more of this subtype and fewer of the others.4
The onset of ALM generally occurs later in life in comparison with other types: the literature describes these tumors as usually developing between 59 and 63 years of age, with peak incidence rates in the seventh decade of life.5
ALMs and nodular melanomas are usually diagnosed at later stages than lentigo maligna melanoma or superficial spreading melanoma. The various theories that have been put forward to explain this tendency are not mutually exclusive. They include the relatively more aggressive biological behavior of ALMs, lack of patient awareness that tumors can grow under the nail or on palms and soles, differences in the clinical presentation of ALMs, the difficulty of seeing lesions at sites that are usually covered, and less attention given to health in the age bracket in which ALM presents.
The ABCDE criteria6—referring to asymmetry, border (irregular), color (variegated), diameter (>6mm), and evolving over time—offer a way to detect malignant melanomas early. Another tool that serves the same purpose is the Glasgow 7-point checklist: change in size, shape or color; diameter over 6mm; oozing (or bleeding) or crusting; inflammation; or changes in sensation (such as itching). Because ALMs develop in sites that are harder to inspect and because this subtype has an appearance that can be unlike melanomas in other locations and so is less familiar to the general population, these tumors may be noticed late by both patients and health care professionals.
The aim of this study was to describe the clinical presentation of ALM, the ways in which these tumors are usually detected, and the prevalence of the signs and symptoms of the ABCDEs and the 7-point Glasgow checklist.
Patients and MethodsThis retrospective observational study was based on cases registered in the cutaneous melanoma database of the Instituto Valenciano de Oncología (IVO), Valencia, Spain.7 Patients diagnosed with ALM were telephoned to collect patient and lesion data. The lesion as described was later compared to preoperative photographs when they were available.
All surviving patients with an ALM who received curative treatment from the dermatology department of the IVO between January 1999 and December 2006 were included if they were able to complete the telephone survey in the first half of 2007.
We recorded the following data for each patient: sex, age when clinical signs were noticed, age on excision of the tumor, and education. The education variable was categorized by the age when the patient's formal schooling ended (≤14 years, ≤18 years, ≤21 years, >21 years); these categories were considered as the equivalents of little or no education, elementary education, mid-level secondary education, and higher education, respectively.
The telephone questionnaire covered the clinical course of the lesion, the patient's reason for seeking care, diagnostic delay, and signs and symptoms.
Data relevant to the clinical course of the lesion included site, whether or not there had been a previous lesion at the same site (none, congenital, lifelong, years present), and whether the patient had had burns or other injuries at the site (none, minor, serious).
Variables related to the reason for seeking care included the first person who noticed the lesion (patient, physician, other), whether or not the lesion was the reason the patient consulted the physician, who suggested the consultation, number of health care professionals consulted and their specialties, and previous diagnoses.
Patient delay was defined as time between first notice of the lesion and first visit to a physician about it. Medical delay was defined as time between first visit to a physician and the biopsy procedure. Both types of delay were classified into the following intervals: ≤1 month, >1 month but ≤3 months, >3 months but ≤6 months, >6 months but ≤1 year, and > 1 year.
Items referring to the signs and symptoms listed in the ABCDEs of skin tumors and the 7-point Glasgow checklist were also included in the telephone questionnaire about presenting symptoms.
ResultsFrom 1999 to 2006, the dermatology department of the IVO followed 1017 patients with cutaneous melanoma. Of the 85 patients (8.36%) who had a melanoma in an acral location, 46 were diagnosed with ALM (4.52% of all melanomas, and 54.1% of melanomas in acral locations). The remaining tumors in an acral location were distributed as follows: 23 superficial spreading melanomas, 15 nodular melanomas, and 1 lentigo maligna melanoma. Only 34 of the 46 patients with ALMs were still alive at the time of this study. Eight of the survivors could not be located for the telephone interview and 3 were unable to participate (1 had had a stroke, 1 had dementia, and 1 was experiencing adverse effects of interferon treatment). Thus, only 23 patients responded to the telephone questionnaire.
Six were men and 17 women. Eighteen had left formal education by the age of 14 years, 1 studied until the age of 17 years, and 2 until 21 years; 2 had higher education.
The median age when these patients first noticed the lesion was 64 years (range, 39–85 years). The median age on excision was 66 years (range, 39–86 years). The mean (SD) tumor thickness was 3.07 (2.23)mm. The median thickness was 2.90mm (range, 0.8–9mm).
Most patients could not recall whether any other lesion had been diagnosed at the site of the melanoma. Only 13.4% provided such information: 1 patient reported that the tumor had appeared over a congenital lesion, 1 remembered an underlying lifelong lesion, and 1 a lesion of 10 years’ duration. Five (21.7%) recalled a significant injury at the site of the tumor, but none remembered burns.
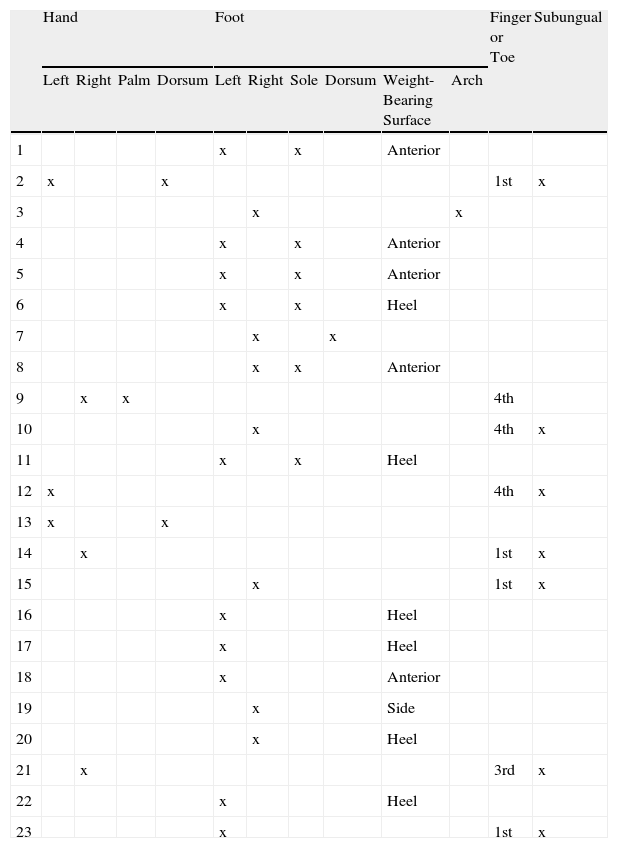
The sites of the ALMs are listed in Table 1. Seventeen were on the foot (73.9%) and 6 (26.1%) on the hand. Four of the hand ALMs were under the nail; there was no clear predominance of one hand over another. Most of the foot ALMs were located on the sole (12 cases). Of those not found on a weight-bearing surface, 1 was on the arch, 1 on the dorsum, and 2 were under a nail (1 on the first toe and 1 on the fourth).
Sites of Acral Lentiginous Melanomas in the Series.
| Hand | Foot | Finger or Toe | Subungual | |||||||||
| Left | Right | Palm | Dorsum | Left | Right | Sole | Dorsum | Weight-Bearing Surface | Arch | |||
| 1 | x | x | Anterior | |||||||||
| 2 | x | x | 1st | x | ||||||||
| 3 | x | x | ||||||||||
| 4 | x | x | Anterior | |||||||||
| 5 | x | x | Anterior | |||||||||
| 6 | x | x | Heel | |||||||||
| 7 | x | x | ||||||||||
| 8 | x | x | Anterior | |||||||||
| 9 | x | x | 4th | |||||||||
| 10 | x | 4th | x | |||||||||
| 11 | x | x | Heel | |||||||||
| 12 | x | 4th | x | |||||||||
| 13 | x | x | ||||||||||
| 14 | x | 1st | x | |||||||||
| 15 | x | 1st | x | |||||||||
| 16 | x | Heel | ||||||||||
| 17 | x | Heel | ||||||||||
| 18 | x | Anterior | ||||||||||
| 19 | x | Side | ||||||||||
| 20 | x | Heel | ||||||||||
| 21 | x | 3rd | x | |||||||||
| 22 | x | Heel | ||||||||||
| 23 | x | 1st | x | |||||||||
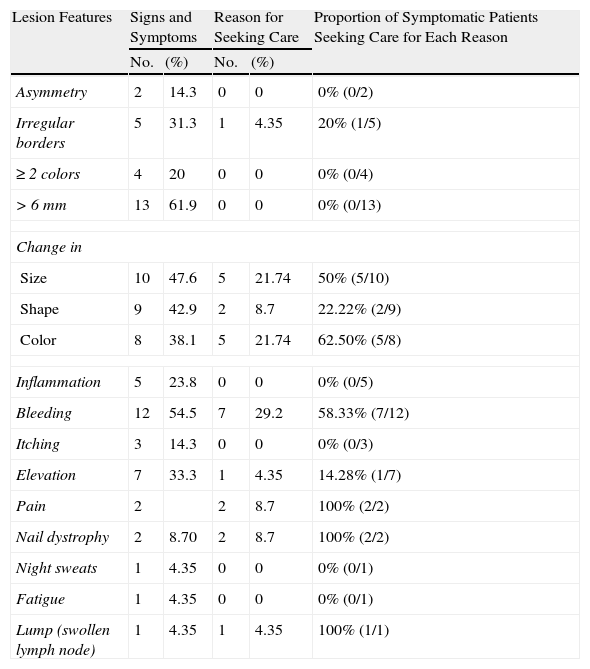
The signs and symptoms reported by the 23 patients (Table 2), in order of frequency, were size greater than 6mm by 13 patients (61.9%), bleeding by 12 (54.5%), change in size by 10 (47.6%), change in shape by 9 (42.9%), change in color by 8 (38.1%), and elevation above the surface of the skin by 7 (33.3%). Other mentioned signs and symptoms that were outside the scope of either the ABCDE criteria or the Glasgow 7-point checklist were nail dystrophy (2 cases), night sweats of several months’ duration (1 case), fatigue (1 case), and a lump in the groin (1 case). Signs or symptoms that were reasons for seeking care, in order of frequency, were bleeding in 7 cases (29.2%), change in color in 5 (21.7%), change in size in 5 (21.7%), change in shape in 2 (8.7%), pain in 2 (8.7%), and nail dystrophy in 2 (8.7%). The following reasons were given by 1 patient (4.4%) each: elevation above the surface of the skin, observation of irregular borders, and lump in the groin.
Signs and Symptoms Reported by Patients, ABCDE Criteria According to Photographs on Record, and Reasons Given for Seeking Care.
| Lesion Features | Signs and Symptoms | Reason for Seeking Care | Proportion of Symptomatic Patients Seeking Care for Each Reason | ||
| No. | (%) | No. | (%) | ||
| Asymmetry | 2 | 14.3 | 0 | 0 | 0% (0/2) |
| Irregular borders | 5 | 31.3 | 1 | 4.35 | 20% (1/5) |
| ≥2 colors | 4 | 20 | 0 | 0 | 0% (0/4) |
| >6mm | 13 | 61.9 | 0 | 0 | 0% (0/13) |
| Change in | |||||
| Size | 10 | 47.6 | 5 | 21.74 | 50% (5/10) |
| Shape | 9 | 42.9 | 2 | 8.7 | 22.22% (2/9) |
| Color | 8 | 38.1 | 5 | 21.74 | 62.50% (5/8) |
| Inflammation | 5 | 23.8 | 0 | 0 | 0% (0/5) |
| Bleeding | 12 | 54.5 | 7 | 29.2 | 58.33% (7/12) |
| Itching | 3 | 14.3 | 0 | 0 | 0% (0/3) |
| Elevation | 7 | 33.3 | 1 | 4.35 | 14.28% (1/7) |
| Pain | 2 | 2 | 8.7 | 100% (2/2) | |
| Nail dystrophy | 2 | 8.70 | 2 | 8.7 | 100% (2/2) |
| Night sweats | 1 | 4.35 | 0 | 0 | 0% (0/1) |
| Fatigue | 1 | 4.35 | 0 | 0 | 0% (0/1) |
| Lump (swollen lymph node) | 1 | 4.35 | 1 | 4.35 | 100% (1/1) |
Two patients (8.7%) reported visiting a podologist for evaluation of a different lesion; the podologist made the diagnosis and referred the patient to a dermatologist. The lesion was detected by the patient in 17 cases (73.9%), but the idea of consulting a specialist came from a friend or relative in 6 of those cases (35.3%). One of the tumors was detected by a family practitioner who was being consulted for another complaint; the patient was referred to a dermatologist. One was detected casually by a dermatologist who was being asked to evaluate another lesion. In 4 of the 5 cases in which the patient consulted after being encouraged to do so by another person (relative or friend), the advisor was female. Five patients (21.7%) consulted about a problem other than the ALM.
Thirteen of the 17 women detected their own tumor, 10 of them (76.9%) made their own decision to consult a specialist, and 3 (23.1%) were advised to do so by someone else. Four of the 6 men detected their own lesion; 1 decided on his own to consult a specialist, and 3 were advised by someone else to do so.
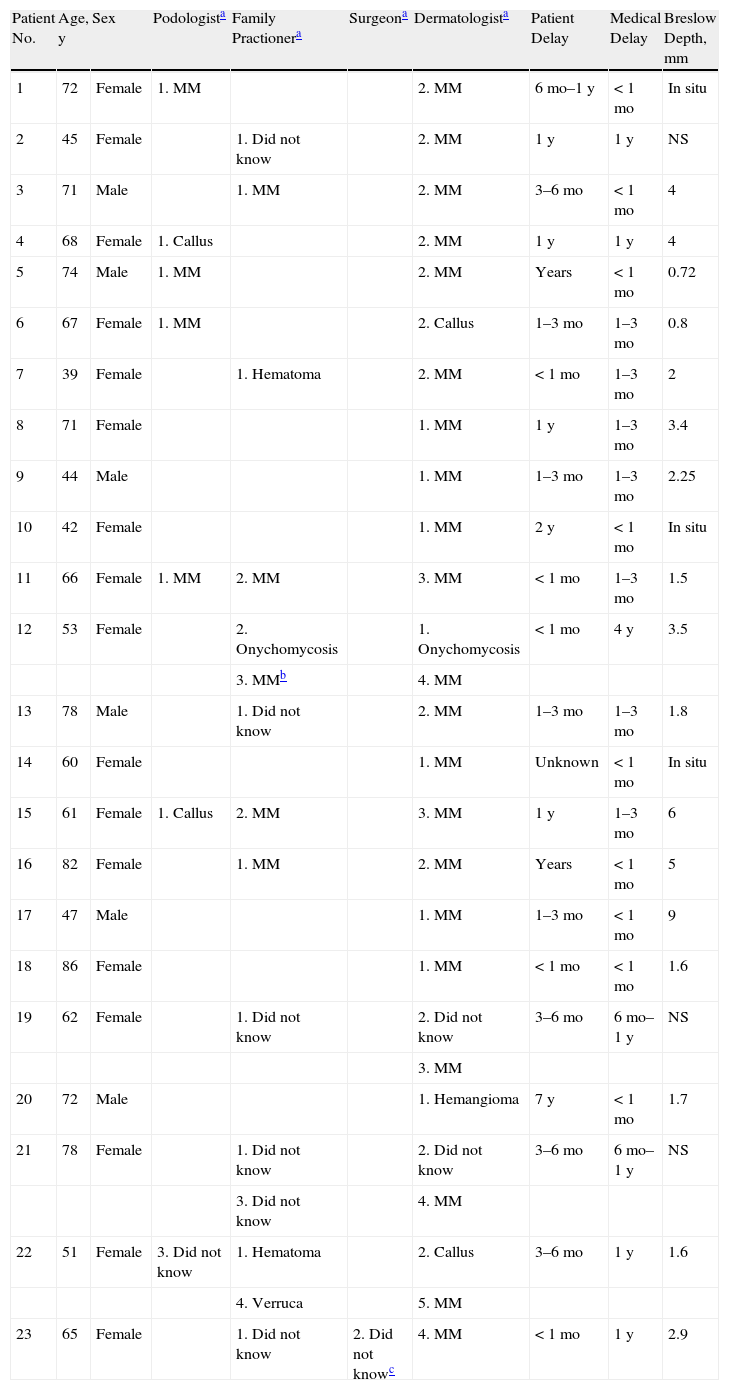
Time elapsed before a health care professional was consulted and time until biopsy are summarized in Table 3. By order of frequency, the first health care professional consulted was a family practitioner in 9 cases (34.8%), a dermatologist in 8 (39.1%), and a podologist in 6 (26.1%). Four of the 6 podologists (66.7%) suspected from the start that the lesion would have to be biopsied; 5 of the 10 family practitioners (50%) and 21 of the 27 dermatologists (77.8%) made the same assessment. Regarding the clinical course of the lesion, the patient was advised that a biopsy would be necessary by the first physician consulted in only 13 cases (56.5%), by the second in 5 cases (21.7%), by the third in 1 (4.4%), by the fourth in 3 (13.0%), and by the fifth in 1 case (4.4%).
Health Care Professionals Consulted by the 23 Patients Interviewed, Diagnostic Delays, and Breslow Thickness.
| Patient No. | Age, y | Sex | Podologista | Family Practionera | Surgeona | Dermatologista | Patient Delay | Medical Delay | Breslow Depth, mm |
| 1 | 72 | Female | 1. MM | 2. MM | 6mo–1y | <1mo | In situ | ||
| 2 | 45 | Female | 1. Did not know | 2. MM | 1y | 1y | NS | ||
| 3 | 71 | Male | 1. MM | 2. MM | 3–6mo | <1mo | 4 | ||
| 4 | 68 | Female | 1. Callus | 2. MM | 1y | 1y | 4 | ||
| 5 | 74 | Male | 1. MM | 2. MM | Years | <1mo | 0.72 | ||
| 6 | 67 | Female | 1. MM | 2. Callus | 1–3mo | 1–3mo | 0.8 | ||
| 7 | 39 | Female | 1. Hematoma | 2. MM | <1mo | 1–3mo | 2 | ||
| 8 | 71 | Female | 1. MM | 1y | 1–3mo | 3.4 | |||
| 9 | 44 | Male | 1. MM | 1–3mo | 1–3mo | 2.25 | |||
| 10 | 42 | Female | 1. MM | 2y | <1mo | In situ | |||
| 11 | 66 | Female | 1. MM | 2. MM | 3. MM | <1mo | 1–3mo | 1.5 | |
| 12 | 53 | Female | 2. Onychomycosis | 1. Onychomycosis | <1mo | 4y | 3.5 | ||
| 3. MMb | 4. MM | ||||||||
| 13 | 78 | Male | 1. Did not know | 2. MM | 1–3mo | 1–3mo | 1.8 | ||
| 14 | 60 | Female | 1. MM | Unknown | <1mo | In situ | |||
| 15 | 61 | Female | 1. Callus | 2. MM | 3. MM | 1y | 1–3mo | 6 | |
| 16 | 82 | Female | 1. MM | 2. MM | Years | <1mo | 5 | ||
| 17 | 47 | Male | 1. MM | 1–3mo | <1mo | 9 | |||
| 18 | 86 | Female | 1. MM | <1mo | <1mo | 1.6 | |||
| 19 | 62 | Female | 1. Did not know | 2. Did not know | 3–6mo | 6mo–1y | NS | ||
| 3. MM | |||||||||
| 20 | 72 | Male | 1. Hemangioma | 7y | <1mo | 1.7 | |||
| 21 | 78 | Female | 1. Did not know | 2. Did not know | 3–6mo | 6mo–1y | NS | ||
| 3. Did not know | 4. MM | ||||||||
| 22 | 51 | Female | 3. Did not know | 1. Hematoma | 2. Callus | 3–6mo | 1y | 1.6 | |
| 4. Verruca | 5. MM | ||||||||
| 23 | 65 | Female | 1. Did not know | 2. Did not knowc | 4. MM | <1mo | 1y | 2.9 |
ABBREVIATIONS: MM, malignant melanoma; NS, not specified
The patient waited less than a month before consulting in 6 of the 23 cases (26.1%), from 1 to 3 months in 4 cases (17.4%), from 3 to 6 months in 3 (13.0%), from 6 months to 1 year in 3 (13.0%), and more than a year in 7 (30.4%). Thus, 43.4% of the patients delayed longer than 6 months before having the lesion evaluated.
Medical system delay was less than a month in 9 of the 23 cases (39.1%), from 1 to 3 months in 7 cases (30.4%), from 3 to 6 months in 1 (4.4%), from 6 months to a year in 2 (8.7%), and over a year in 5 (21.7%) Thus, diagnostic delay of more than 6 months was attributable to health care personnel in nearly a third of the cases.
DiscussionCertain limitations must be taken into consideration before drawing conclusions from this descriptive study. First, data were collected retrospectively from a small sample by telephone survey, during which patients had to remember past events. This method also introduced the possibility that interviewed survivors had had a better prognosis. Nonetheless, the data on ALMs are interesting and generally consistent with those described in the literature.
The site of the ALM was the foot in most of the 23 patients, but subungual tumors were more often found on the hand. The first toe or finger were the ones most often involved. Foot tumors were usually found on weight-bearing surfaces, suggesting that pressure may play a pathogenic role, perhaps in relation to heat or repeated trauma. The recent finding of overexpression of the NUAK2 oncogene in ALM might support this theory.8 The foot was involved in 82% of ALMs in a previously described series,9 but the hand is more often the location of subungual tumors3,10,11 (55% on the hand and 45% on the foot10). Plantar melanomas have been found to account for 2.8%12 of all malignant melanomas, and hand melanomas between 1% and 2%13; others have also found the first finger or toe to be more common sites than other digits.
Even though ABCDE and 7-point Glasgow signs and symptoms often refer to the palms and soles, diagnostic delay is common because of the clinical heterogeneity of ALM tumors. In a series of 112 plantar ALMs, Soon and coworkers9 found that 33.96% had previously been incorrectly diagnosed; 60% of the misdiagnoses were amelanotic and 39% resembled benign hyperkeratotic lesions.
In our series of 23 patients, 61.9% reported that tumor size exceeded 6mm, 54.5% observed bleeding, 47.6% a change in size, and 42.9% a change in shape. For at least half of these patients, however, only pain or bleeding were important enough reasons to consult a specialist. In any case bleeding and color and size changes were the main reasons patients sought a specialist's opinion.
Interestingly, only 39.1% of the patients consulted a dermatologist first; 37.8% first saw a family practitioner, and 26.1% a podologist. As might be expected, dermatologists suspected a malignant lesion more often (77.8%) than podologists (66.7%) or family practitioners (50%). This finding underlines the important role that some health professionals—particularly podologists—can potentially play in detecting ALMs early in the disease process.
Diagnostic delays were considerable in our series, whether because of patient decisions (52.2% waited over 3 months to seek a medical opinion and 34.8% waited a year or more) or medical factors (only 56.5% of the lesions were thought to require biopsy in the first visit, and the biopsy procedure was delayed more than 3 months in 56.5%). In the series described by Richard and coworkers,14 no excision plan was proposed by 14.2% of the physicians visited first. Delays were longer in atypical presentations, such as amelanotic malignant melanomas, lesions not forming on a previous nevus, and in ALMs in that series. However, the percentages we report are considerably higher (43.5% in the series overall and 22.2% among dermatologists in our series).
An important observation was that even though a large number of patients (73.9%) detected the lesion themselves, 35.3% of them decided to consult a specialist only after a relative or friend advised them to. Also interesting, the idea to seek care came mostly from women (whether patients or relatives), an observation that is consistent with the literature. Richard and coworkers14,15 have found that in about two-thirds of malignant melanoma cases, the lesion is detected by the patient or a relative, and that the relative both detected the lesion and encouraged seeking of a medical opinion in half the cases. In those series, as in ours, women detected malignant melanoma more frequently than men, who also usually required a friend or another physician to suggest consulting a specialist. The median time between the patient's discovery of a lesion and suspicion of malignancy was 25 months, and the median delay between suspicion and consulting a physician was 2 months. Significantly, the studies of Richards and coworkers found that in spite of media campaigns to promote prevention, 25% of the patients thought that excising a melanocytic lesion was risky, only 24.8% were aware of the seriousness of melanoma, and others continued to believe that a lesion could not be cancerous if they experienced no bleeding, pain, or fatigue. The signs and symptoms that led to rapid consultation of a health professional were thus late ones, such as bleeding, whereas noticing the ABCDE signs led to delay in seeking care.
In conclusion, both patient-related and physician-related diagnostic delays are considerable. Our findings suggest that campaigns to inform the population about malignant melanoma are failing for a number of reasons: knowledge of the ABCDEs and Glasgow 7-point criteria is still poor, acral areas are not understood to be possible sites of malignant melanoma, information about subungual melanoma is not reaching the public, family physicians and podologists need further training with respect to melanoma, and insufficient attention is being directed toward men.
Ethical DisclosuresProtection of Human and Animal SubjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that they followed their hospital's regulations regarding the publication of patient information and that written informed consent for voluntary participation was obtained for all patients.
Right to Privacy and Informed ConsentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pereda C, et al. Estudio descriptivo de la presentación clínica del melanoma lentiginoso acral. Actas Dermosifiliogr. 2013;104:220–6.