Chromomycosis or chromoblastomycosis is a chronic deep skin mycosis that affects the skin and subcutaneous tissue and is caused by fungi from the Dematiaceae family, which are imperfect fungi that produce pigments similar to melanin. Several species are known to cause chromoblastomycosis; all have low virulence and produce similar clinical manifestations. The most common species is Fonsecaea pedrosoi, followed by Phialophora verrucosa and Cladophialophora carrionii.1,2 Soil and plant debris are natural reservoirs for these fungi, and the common mode of transmission is traumatic inoculation whereby contaminated organic matter enters the skin through a wound.3 There is no established treatment for chromoblastomycosis but various treatment options have been attempted given the refractory nature of the condition. The choice of treatment is generally guided by clinical, mycologic, and histopathologic criteria. We describe a case of imported chromoblastomycosis, a disease rarely seen in Spain, that had been present for many years and was resolved with combination therapy.
The patient was a 50-year-old construction worker from Brazil who had been living in Catalonia, Spain for a year. He had a history of hypertension and presented with mildly pruritic and occasionally painful lesions on the arm and elbow that had been present for 20 years. The lesions had grown progressively and centrifugally and had never completely healed. The patient recalled having been injured with a nail before the lesions appeared. He had attempted treatment with several topical antifungal drugs, with no improvement. He was not on any regular medication.
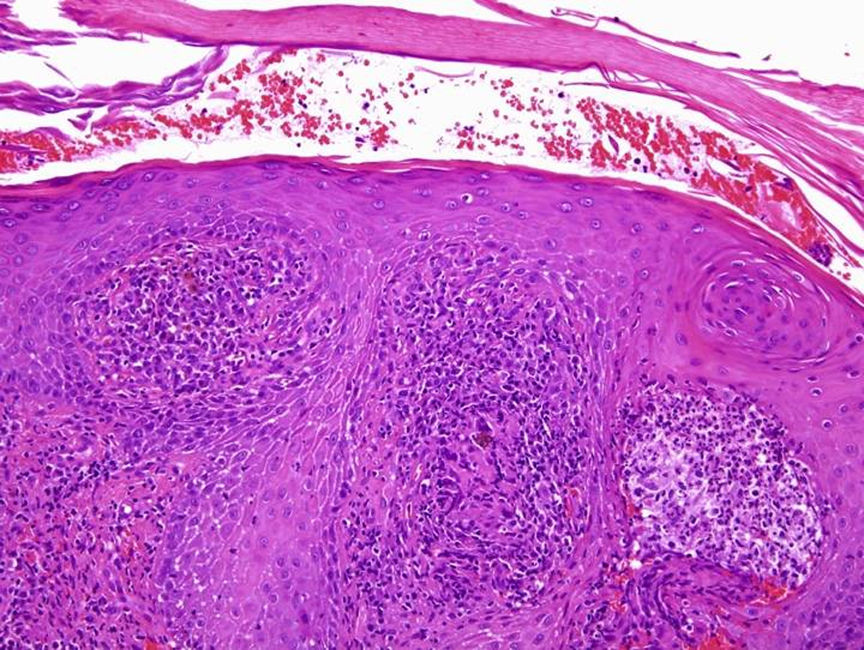
Physical examination revealed indurated, erythematous, contiguous plaques with warty, crusted areas; adjacent to these plaques was a larger whitish area with a scar-like appearance (Fig. 1). The regional lymph nodes were not palpable.
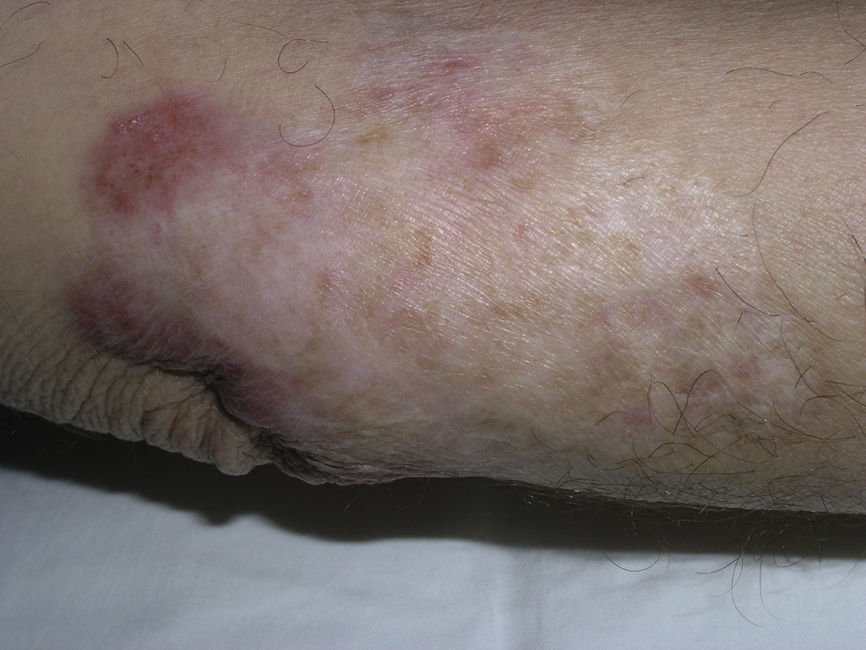
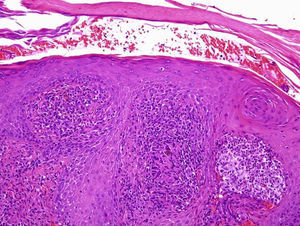
Laboratory tests, including a complete blood count with white blood cell count, basic biochemical tests, liver function tests, and coagulation tests, showed no abnormalities. The erythrocyte sedimentation rate was normal. Histology showed pseudoepitheliomatous epidermal hyperplasia and an intense inflammatory granulomatous reaction throughout the dermis with epithelioid cells, giant multinucleated cells, plasma cells, neutrophils, and occasional microabscesses. The dermis and microabscesses contained small (5-15μm) pigmented spores with a thick wall and in some cases central septation (Fig. 2). Periodic-acid Schiff and methenamine silver stains were positive.
Bacterial and fungal cultures of biopsy specimens yielded several colonies of Stenotrophomonas maltophilia and F pedrosoi, respectively. The mycobacterial culture was negative.
Based on the above results, we established a definitive diagnosis of cutaneous chromoblastomycosis. Topical antibiotics were administered to treat the secondary bacterial infection and the lesions were treated by curettage. The patient was also prescribed terbinafine (500mg/12h) and 1 month later underwent the first of 2 cryotherapy sessions separated by an interval of 2 months. Treatment with terbinafine was maintained for 6 months, with a progressive reduction in doses. The lesions healed, leaving residual scarring (Fig. 3), and no recurrences were observed during the 24-month follow-up period.
Chromoblastomycosis is difficult to treat because of differences in antifungal sensitivity patterns and responses among the species isolated and also because of the refractory nature of the condition, particularly in more serious clinical forms.The different treatment modalities available have not been compared in clinical settings. Recurrence is common, hence the recommendation for long-term treatments, lasting between 3 and 18 months, depending on the study.4 Possible complications include secondary bacterial infection with lymphadenitis and, less frequently, the development of squamous carcinoma in lesions that have been present for a very long time.5 In our case, the only complication was secondary impetiginization, which was resolved with topical antibiotics.
Treatments can be divided into 3 broad modalities: physical treatments,6 pharmacologic treatments, and combined therapies. Surgery may be the best choice in the early stages of disease, but systemic antifungals are necessary in more advanced cases.
A variety of treatment regimens have been attempted, but it is impossible to determine the best option due to a lack of comparative clinical studies using objective criteria. The best systemic antifungals seem to be itraconazole and terbinafine because of their spectrum of action and safety in long-term regimens. However, tissue fibrosis secondary to infection can reduce drug tissue levels. Terbinafine may have antifibrotic properties that would favor the healing of chromoblastomycosis lesions.7,8
Terbinafine combined with cryotherapy has emerged as a possible treatment option in recent years. Of all the physical treatments described in the literature, cryotherapy is associated with the best outcomes, with a cure rate of 40.9% when used as monotherapy.6 Moreover, it appears to be particularly useful when combined with systemic antifungals to treat long-standing lesions that are not candidates for surgery. In such cases the antifungal treatment should be administered a month before cryotherapy to prevent the spread of infection described in patients treated with cryotherapy alone.9,10
In our patient, 2 cycles of cryotherapy combined with oral terbinafine for 6 months achieved cure and caused minimal local adverse effects (hyperpigmentation and mild residual fibrosis). Recent publications confirm that combined therapies offer better results in patients with chronic chromoblastomycosis that is not amenable to surgical treatment.
Please cite this article as: Bassas-Vila J, Fuente M, Guinovart R, Ferrándiz C. Cromomicosis. Respuesta al tratamiento combinado con crioterapia y terbinafina. Actas Dermosifiliogr. 2014;105:196–198.