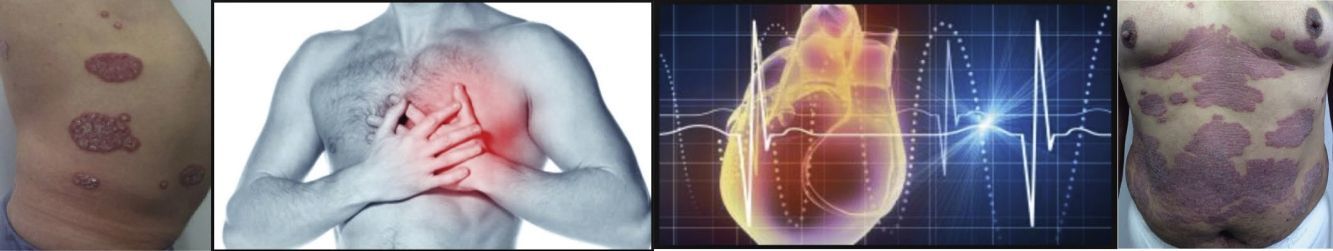
Psoriasis is now known to have a clear association with metabolic syndrome and its components. The aim of our study was to determine the prevalence of cardiovascular risk factors (CVRFs) and increased carotid intima-media thickness in psoriasis patients seen in the dermatology department of a quaternary hospital.
Material and methodsThis was a descriptive cross-sectional study of psoriasis patients aged over 18 years seen in the dermatology department of Hospital de San José in Bogota, Colombia, between March and August, 2015. Directed medical history and physical examination were performed to detect CVRFs, laboratory studies to exclude metabolic syndrome, and ultrasound examination to measure carotid intima-media thickness.
ResultsForty patients with psoriasis were included in the study. The prevalence of the distinct CVRFs was 35% for systemic hypertension, 17.5% for dyslipidemia, 17.5% for smoking, and 10% for type 2 diabetes mellitus. A history of acute myocardial infarction was detected in 12.5% of patients. Metabolic syndrome was found in 20 patients (50%), and blood biochemistry revealed dyslipidemia in 32 patients (80%). Based on the Framingham score, the cardiovascular risk was low in 11 patients (31.4%), intermediate in 22 (62.8%), and high in 2 (5.7%). Mean (SD) carotid intima-media thickness was 0.7 (0.12) mm, with thickening observed in 6 patients (15%).
ConclusionsThis study provides evidence of the high prevalence of CVRFs in psoriasis patients and indicates the need for strict clinical control to monitor cardiovascular risk in this population.
En la actualidad, se ha demostrado que la psoriasis presenta una importante asociación con síndrome metabólico y sus componentes. El objetivo de este estudio es determinar la prevalencia de los factores de riesgo cardiovascular y el engrosamiento de la íntima media carotídea en pacientes con psoriasis que consultan al servicio de dermatología de un hospital de 4.° nivel.
Material y métodosSe realizó un estudio descriptivo de corte transversal en pacientes mayores de 18 años con diagnóstico de psoriasis, atendidos en la consulta de dermatología en el Hospital de San José, en Bogotá, Colombia.
Entre marzo y agosto del 2015, se realizó un interrogatorio y un examen físico dirigido a la identificación de factores de riesgo cardiovascular, pruebas de laboratorio para determinar la presencia de síndrome metabólico y se practicó medición del grosor de la íntima media carotídea por ecografía.
ResultadosFueron incluidos 40 pacientes con psoriasis. La prevalencia de factores de riesgo cardiovascular en este grupo de pacientes fue del 35% para hipertensión arterial, el 17,5% para dislipidemia, el 17,5% para tabaquismo y el 10% para diabetes mellitus tipo 2. El 12,5% de los sujetos tenía antecedente de infarto agudo de miocardio.
Se encontró síndrome metabólico en 20 (50%) pacientes. La dislipidemia se reportó por bioquímica sanguínea en 32 (80%) pacientes. Según el score de Framingham, 11 pacientes (31,4%) tenían riesgo latente, 22 (62,8%) riesgo intermedio y 2 (5,7%) riesgo alto. En la evaluación de la carótida, se encontró una media del espesor intimal de 0,7 (DE 0,12) mm y engrosamiento en 6 pacientes (15,0%).
ConclusionesEste estudio aporta información sobre la prevalencia alta de factores de riesgo cardiovascular en pacientes con psoriasis y orienta a un estricto abordaje clínico para el control del riesgo cardiovascular en esta población.
Psoriasis is a chronic inflammatory disease that affects 2% to 3% of the world's population and occurs across all geographic zones.1 Prevalence rates range from 0.6% to 6.5%; higher rates are found in Nordic countries and lower ones nearer the Equator.2 Three percent of dermatology visits in Colombia concern psoriasis.2 This disease is currently considered to be a systemic process, not exclusively a skin condition, and its association with metabolic syndrome and its components has been demonstrated.3
Inflammatory molecules and hormones produced under conditions such as obesity, diabetes, and atherosclerosis are also known to promote the development of psoriasis or to increase severity if the disease is already present.4
Few studies have evaluated cardiovascular risk in patients with psoriasis in Colombia,2,5 and carotid intima-media thickness (CIMT) has not been measured in this population. We aimed to determine the prevalence of cardiovascular risk factors (CVRFs) and increased CIMT in psoriasis patients treated in the dermatology department of a quaternary hospital.
MethodsA descriptive cross-sectional study was carried out between March and August 2015. Patients older than 18 years of age with a confirmed diagnosis of psoriasis were invited to participate by the dermatology department at Hospital de San José in Bogotá, Colombia.
We excluded patients with rheumatoid arthritis, systemic lupus erythematosus, or any other autoimmune disease.
Candidates with records in the hospital's electronic database who were classified in category 10 (psoriasis) of the International Classification of Diseases and who attended the dermatology clinic between 2007 and March 2015 were identified.
The patients were then telephoned, and if they accepted the invitation to participate they were scheduled to see a physician and undergo tests.
Information about CVRFs (high blood pressure, diabetes mellitus, smoking, dyslipidemia, and family history of cardiovascular disease) was obtained from medical records, an interview with the treating physician, and a physical examination. Time since onset of psoriasis, type (vulgar, pustular, erythrodermic, or inverse), nail involvement, and current treatment were also recorded.
The Psoriasis Area and Severity Index (PASI) was calculated to classify severity as mild (score <10) or moderate (≥10).6 Total body surface area affected was also estimated to reflect disease severity, classified as mild (≤10%) or moderate to severe (>10%). The impact of psoriasis on quality of life was measured with the Dermatology Life Quality Index and categorized according to the following score ranges: 0–1, no effect; 2–5, small effect,; 6–10, moderate effect; 11–20, very large effect; and 21–30, extremely large effect.7
Blood pressure, weight, and height were measured during the visit. Body mass index was calculated with the Quetelet formula (kg/m2),8 and patients were classified according to the World Health Organization's weight cutoffs as normal if the index was between 18.5 and 24.9, overweight if between 25 and 29.9, and obese if 30 or higher.
Waist girth was measured at the point halfway between the iliac crest and the last rib at end-expiration with the patient standing. The cutoffs for abdominal obesity were ≥90cm for men and ≥80cm for women, following the recommendations of the International Diabetes Federation for Central and South America.9,10
Patients were asked about CVRFs among first-degree relatives (men aged <55 years and women <65 years). Arterial hypertension was noted if the patient was taking an antihypertensive medication or if systolic or diastolic pressures exceeded 140mmHg and 90mmHg, respectively, in measurements taken after 5minutes of rest. The presence of diabetes mellitus was defined by a fasting blood sugar level higher than 126mg/dL or the use of oral antidiabetic medication or insulin. The presence of dyslipidemia was defined according to current use of statins or abnormal lipid findings on blood chemistry. The cutoffs in patients on secondary prevention therapy were as follows: low density lipoprotein (LDL), ≥70mg/dL; high density lipoprotein (HDL) ≤50mg/dL in women and ≤40mg/dL in men; or triglycerides ≥150mg/dL.11 In patients on primary prevention therapy the cutoffs were as follows: LDL, ≥160mg/dL; and HDL or triglycerides as described above.11
Smoking was evaluated with 2 questions on the National Health Interview Survey: Have you smoked fewer than 100 cigarettes in your life? and Do you currently smoke a cigarette every day, some days, or never? Patients who reported smoking fewer than 100 cigarettes over a lifetime but who currently smoked—whether every day or on some days—were classified as smokers. Patients who reported having smoked fewer than 100 cigarettes in their life and who never smoked at the time of the interview were defined as former smokers.12
Blood was extracted to determine fasting blood sugar level, lipid profile, serum creatinine level, and the results of high-sensitivity C-reactive protein (hs-CRP) testing. The hs-CRP test cutoff was ≥2.0mg/L.13
A diagnosis of metabolic syndrome was based on the presence of 3 or more of the following components: insulin resistance (fasting blood sugar ≥100mg/dL or on current treatment), low HDL level (≤40mg/dL in men and ≤50mg/dL in women or on current treatment), elevated triglyceride level (≥150mg/dL), arterial hypertension (systolic pressure ≥130mmHg or diastolic pressure ≥85mmHg, or on current antihypertensive treatment); and abdominal obesity.14
The Framingham risk score to predict the likelihood of a fatal or nonfatal coronary event in the next 10 years was also calculated. The results were expressed as a percentage in 3 ranges: low risk, <10%; intermediate risk, ≥10% to 20%; and high risk, >20%.15
An expert radiologist undertook mode-B ultrasound imaging to measure CIMT (Toshiba Xario SSA-660A equipped with a PLT-1204AX linear array, 7.2–14 Mhz) following the protocol described by the American Society of Echocardiography.16 Six CIMT measurements were recorded on each side and averaged to identify the presence of thickening. A cutoff of ≥0.8mm was used based on the findings of Groot et al.17
The results were given to patients during a medical visit, and lifestyle and related strategies for managing cardiovascular risk were explained. Patients were referred to appropriate specialists if required.
Statistical AnalysisDescriptive statistics for continuous variables were expressed as means (SD). Results for categorical variables were expressed as absolute frequencies and percentages. We also calculated the prevalence rates of CVRFs, metabolic syndrome, and increased CIMT. The correlation between CIMT and the Framingham score expressed as an absolute number was estimated with the Spearman correlation coefficient (ρ).
ResultsEighty-four of the 197 candidates found in the database were contacted; 42 agreed to participate. The researchers in charge of data collection were unable to reach the remaining 113 patients by telephone. The 42 patients who declined to participate said they lacked time to come to the hospital and schedule tests.
Of the 42 patients who agreed to participate, 2 did not attend for blood extraction. Thus, we studied 40 patients. The mean age was 54 (11.8) years (female-to-male ratio, 0.53:1). All were diagnosed with plaque psoriasis, and 15 (37.5%) had nail involvement. The median time since onset of psoriasis was 12.5 years (interquartile range, 7–23 years). PASI scoring indicated that 80% (32/40) had mild disease, and 20% had moderate to severe disease. Dermatology Quality of Life Index results indicated that over 40% experienced moderate to extremely large effects on their quality of life (Table 1).
Sociodemographic and Clinical Characteristics of the Patients With Psoriasis.
| Age, y, mean (SD) | 54 | (11.8) |
| Male sex, n (%) | 26 | (65.0) |
| Place of origin, n (%) | ||
| Bogotá | 29 | (72.5) |
| Cundinamarca | 9 | (22.5) |
| Boyacá | 1 | (2.5) |
| Huila | 1 | (2.5) |
| Type of psoriasis, n (%) | ||
| Plaque psoriasis | 40 | (100.0) |
| Nail involvement | 15 | (37.5) |
| Time since onset, y, median (IQR) | 12.5 | (7–23) |
| Psoriasis Area and Severity Index, n (%) | ||
| Mild disease | 32 | (80.0) |
| Moderate-severe disease | 8 | (20.0) |
| Body surface area, n (%) | ||
| Mild disease | 15 | (37.5) |
| Moderate disease | 14 | (35.0) |
| Severe disease | 11 | (27.5) |
| Dermatology Quality of Life Index, n (%) | ||
| No effect on quality of life | 6 | (15.0) |
| Small effect | 10 | (25.0) |
| Moderate effect | 13 | (32.5) |
| Very large effect | 9 | (22.5) |
| Extremely large effect | 2 | (2.5) |
| Topical treatments used, n (%)a | ||
| Corticosteroids | 27 | (67.5) |
| Acetylsalicylic acid | 9 | (22.5) |
| Vitamin D analogs | 7 | (17.5) |
| Calcineurin inhibitors | 1 | (2.5) |
| Coal tar | 3 | (7.5) |
| Anthralin | 1 | (2.5) |
| Emollients | 21 | (52.5) |
| Systemic treatments, n (%) | ||
| Methotrexate | 7 | (17.5) |
| Ciclosporin | 1 | (2.5) |
| Adalimumab | 4 | (10.0) |
| Phototherapy, n (%)b | 2 | (5.0) |
| UV-B | 1 | (2.5) |
| Narrowband UV-B | 1 | (2.5) |
| Psoralen plus UV-A | 1 | (2.5) |
| Treatment interruptions in last 6 mo, n (%)c | 13 | (32.5) |
| Family history of psoriasis, n (%) | 7 | (17.5) |
Abbreviation: IQR, interquartile range.
The CVRF prevalences most commonly reported were high blood pressure (35%), dyslipidemia (17.5%), smoking (17.5%), and type 2 diabetes (10%). An acute myocardial infarction was reported by 5 patients (12.5%). The prevalence rates of CVRFs and metabolic abnormalities are summarized in Table 2. The mean CIMT measurement for the study sample was 0.7(0.12)mm and increased CIMT was identified in 6 patients (15.0%), 2 of whom had had a myocardial infarction. We observed moderately linear correlations between CIMT and 10-year risk of a cardiovascular event predicted by the Framingham score: (ρ=0.55, P=.002) and blood sugar levels (ρ=0.46; P=.002). No correlation between hs-CRP results and CIMT (P=.48) was found.
CVRFs in 40 Patients With Psoriasis.
| Variable | Women | Men | Total | |||
|---|---|---|---|---|---|---|
| n=14 | n=26 | n=40 | ||||
| Age, y, mean (SD) | 52.6 | (10.1) | 54.8 | (12.7) | 54.0 | (11.8) |
| Patient medical history, n (%) | ||||||
| Hypertension | 5 | (35.7) | 9 | (34.6) | 14 | (35.0) |
| Diabetes mellitus, type 2 | 0 | 0 | 4 | (15.2) | 4 | (10.0) |
| Dyslipidemia | 2 | (14.2) | 5 | (19.2) | 7 | (17.5) |
| Chronic kidney disease | 0 | 0 | 0 | 0 | 0 | 0 |
| Autoimmune disease | 0 | 0 | 0 | 0 | 0 | 0 |
| Acute myocardial infarction | 2 | (14.2) | 3 | (11.5) | 5 | (12.5) |
| Myocardial revascularization | 1 | (7.1) | 1 | (3.8) | 2 | (5.0) |
| Angioplasty | 1 | (7.1) | 3 | (11.5) | 4 | (10.0) |
| Coronary stent | 0 | 0 | 3 | (11.5) | 3 | (7.5) |
| Carotid artery disease | 0 | 0 | 0 | 0 | 0 | 0 |
| Stroke | 0 | 0 | 0 | 0 | 0 | 0 |
| Peripheral artery disease | 0 | 0 | 0 | 0 | 0 | 0 |
| Smoking | 1 | (7.1) | 6 | (23.1) | 7 | (17.5) |
| Ex-smoker | 1 | (7.1) | 7 | (26.9) | 8 | (20.0) |
| Use of acetylsalicylic acid | 2 | (14.2) | 6 | (23.0) | 8 | (20.0) |
| Use of statins | 2 | (14.2) | 6 | (23.0) | 8 | (20.0) |
| Use of antihypertensive medication | 5 | (35.7) | 9 | (34.6) | 14 | (35.0) |
| Use of oral antidiabetic drugs | 0 | 0 | 3 | (11.5) | 3 | (7.5) |
| Other | 5 | (35.7) | 2 | (7.6) | 7 | (17.5) |
| Family history of cardiovascular disease, n (%)a | 3 | (21.4) | 2 | (7.6) | 5 | (12.5) |
| Systolic arterial pressure, mm Hg, mean (SD) | 120.3 | (14.7) | 122.9 | (14.6) | 122.05 | (14.5) |
| Minimum and Maximum | 90 | 160 | 90 | 158 | 90 | 160 |
| Diastolic arterial pressure, mm Hg, mean (SD) | 75.7 | (7.5) | 73.8 | (8.9) | 74.5 | (8.4) |
| Minimum and Maximum | 60 | 90 | 60 | 90 | 60 | 90 |
| Body mass index, kg/m,2mean (SD) | 30.4 | (5.4) | 28.3 | (4.9) | 29.0 | (5.1) |
| Normal | 3 | (21.4) | 8 | (30.8) | 11 | (27.5) |
| Overweight | 4 | (28.6) | 9 | (34.6) | 13 | (32.5) |
| Obese | 7 | (50.0) | 9 | (34.6) | 16 | (40.0) |
| Waist girth, cm, mean (SD) | 98.1 | (9.4) | 100.8 | (13.0) | 99.8 | (11.8) |
| Abdominal obesity, n (%) | 14 | (100.0) | 21 | (80.77) | 35 | (87.5) |
| Elevated triglycerides, n (%) | 6 | (42.9) | 11 | (42.3) | 17 | (42.5) |
| Low HDL, n (%) | 3 | (21.4) | 23 | (88.5) | 26 | (65.0) |
| Elevated triglycerides+low HDL, n (%) | 1 | (7.1) | 11 | (42.3) | 12 | (30.0) |
| Metabolic syndrome, n (%)b | 6 | (42.9) | 14 | (53.8) | 20 | (50.0) |
| Framingham 10-y risk score, n (%)c | ||||||
| Low risk | 5/12 | (41.6) | 6/23 | (26.0) | 11/35 | (31.4) |
| Intermediate risk | 7/12 | (58.3) | 15/23 | (65.2) | 22/35 | (62.8) |
| High risk | 0 | 0 | 2/23 | (8.7) | 2/35 | (5.7) |
| High-sensitivity CRP, mg/L, median (IQR) | 3.8 | (1.3–8.0) | 2.51 | (0.6–5.0) | 3.01 | (0.6–6.5) |
| Elevated CRP level, n (%) | 9 | (64.3) | 15 | (57.7) | 21 | (52.5) |
| CIMT, mm, mean (SD) | 0.655 | 0.102 | 0.72 | 0.129 | 0.702 | 0.124 |
| 90th percentile | 0.78 | 0.91 | 0.85 | |||
| 75th percentile | 0.75 | 0.78 | 0.755 | |||
| 50th percentile | 0.68 | 0.71 | 0.68 | |||
| 25th percentile | 0.57 | 0.66 | 0.635 | |||
| Increased CIMT, n (%)d | – | – | 6 | (23.1) | 6 | (15.0) |
Abbreviations: CIMT, carotid intima-media thickness; CRP, C-reactive protein; CVRF, cardiovascular risk factor; HDL, high-density lipoproteins; IQR, interquartile range.
Presence of premature cardiovascular disease in a first-degree relative (for men, <55 y; for women, <65 y.
Presence of 3 or more of the following components: fasting blood sugar ≥100mg/dL, HDL ≤40mg/dL in men and ≤50mg/dL in women or currently in treatment, triglycerides ≥150mg/dL or under treatment, blood pressure ≥130/85mmHg or on antihypertensive treatment, abdominal obesity (waist girth ≥90cm for men and ≥80cm for women).
Psoriasis has been shown to be an independent CVRF.15,18 We found that the prevalence of metabolic syndrome in our psoriasis patients was around 50%, near the figures of 56.5%2 and 59.6%5 reported in other Colombian studies. These prevalence rates are higher than those found in other Latin American or European countries where metabolic syndrome has been detected in 45.1%19 and in around 25% in several studies.3,15,20
Higher rates of metabolic syndrome have been found in Hispanic populations than in Caucasian, Asian, or African-American cohorts.21 Metabolic syndrome is 2.26-fold higher in patients with psoriasis (95% CI, 1.7–3.01) than in the general population according to a meta-analysis of data for 1.4 million individuals.22
The prevalence of high blood pressure in our study was consistent, at around 35%, with the findings of another Colombian study.2 That figure stands in contrast with the prevalence of 13.4% reported by the CARMELA study for the general population of Bogotá.23 The prevalence of diabetes mellitus type 2 in our study (10%) was consistent with the findings of Jiménez et al.2 (10.9%) but contrasts with the report of a 36.5% prevalence by Rojas et al.5 However, those authors grouped patients with a history of diabetes together with those with fasting plasma glucose levels exceeding 100mg/dL.
Others have reported high prevalences of dyslipidemia, but the definitions used have varied greatly. We found that 80% had abnormal lipid metabolism evident in low HDL levels or elevated LDL or triglyceride levels. Jiménez et al.2 reported that 43.5% of psoriasis patients had a history of dyslipidemia, and Rojas et al.5 measured elevated triglycerides and low HDL levels in 61.5%.5 An association between elevated triglycerides and low HDL levels was reported in 62.8% of patients in a European study24; the rate we found was lower, at 30%.
The Framingham scores calculated for our patients with psoriasis who had not yet experienced a coronary event showed that their absolute risk of such an event within 10 years was higher than the general population's, consistent with the findings of Gisondi et al.,15 who calculated the risk to be 11.2% for psoriasis patients and 7.3% for others (P<0.01). Our patients’ scores indicated that 62.8% were at intermediate risk of an event and 5.7% were at high risk. It is important to remember that we calculated the Framingham score only for patients who had never had a coronary event. If we add to these risk levels the fact that 12.5% of our patients had already had such an event, we can estimate that 18.2% of these patients are at high risk. That figure points to the need for physicians to direct their efforts toward strictly controlling cardiovascular risk. Furthermore, although these figures are high, some studies have found that the Framingham score in fact underestimates cardiovascular risk in psoriasis because the proatherosclerotic effects of long-term inflammation are not taken into account. Nor does the score take into account the nontraditional risk factors that are found more often in patients with severe psoriasis.15,25 The actual risk of our patients, therefore, could be even higher than our findings suggest.
We saw a moderate correlation between CIMT and risk of a coronary event within 10 years (Framingham score) (ρ=0.55, P=.002). The average CIMT of 0.70mm in our patients was consistent with the findings of Bussoetal.26 in a Latin American study (0.70mm in patients with psoriasis and 0.63mm in a control group). When Schargrodskyet al.23 studied 10826 patients between the ages of 25 and 64 years in 7 Latin American cities, including Bogotá, they found that CIMT measurements varied greatly between individuals, ranging from 0.60mm to 0.74mm. In Bogotá, the average was 0.61mm, but the mean for our patients with psoriasis was higher.
Large studies have shown that psoriasis is associated with increased CIMT, contributing to atherosclerotic processes and the development of cardiovascular events.27 Risk is greater for patients with a CIMT of more than 0.8mm.28 Of our 6 patients with measurements over that cutoff, 2 had already experienced myocardial infarction, 2 had metabolic syndrome, and 2 did not, suggesting that CIMT is an important subclinical predictor of cardiovascular risk that could be useful for guiding decisions about systemic treatments.29 Psoriasis patients have higher circulating CRP levels than healthy individuals, and their CRP elevations correlate with severity of disease.30 However, we found no correlation between CIMT and PASI or disease severity in our study, even though more than half our patients had high CRP levels consistent with the literature on patients with psoriasis.30
To the best of our knowledge, this is the first study to use standardized measurements to describe a group of patients with psoriasis in Bogotá. We have provided information on traditional CVRFs, Framingham scores, CIMT, and hs-CRP results for this patient cohort. A limitation of the study was the small number of patients included. The fact that all were recruited from a single center and the nonresponse rate was 50% were also limitations. Selection bias must therefore be recognized given that our data only reflect patients who agreed to participate.
In conclusion, this study has provided information on the high prevalence of CVRFs in Colombian patients with psoriasis, consistent with the international literature. Furthermore, half the patients studied had elevated hs-CRP test results and on average their CIMT was also greater than measurements in individuals without psoriasis.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that the procedures followed adhered to the ethical guidelines of the responsible committee on human experimentation and comply with the Declaration of Helsinki of the World Medical Association.
Data confidentialityThe authors declare that they followed their hospitals’ regulations regarding the publication of patient information and that written informed consent for voluntary participation was obtained for all patients.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in this article. The signed forms are in the possession of the corresponding author.
FundingThe study was funded through an internal grant program from the University Foundation for Health Sciences (Fundación Universitaria de Ciencias de la Salud), Bogotá, Colombia (grant number 112-52157-3).
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Argote A, Mora-Hernández O, Milena Aponte L, Barrera-Chaparro DI, Muñoz-Ruiz LM, Giraldo-Mordecay L, et al. Factores de riesgo cardiovascular y grosor de la íntima media carotídea en una población colombiana con psoriasis. Actas Dermosifiliogr. 2017;108:738–745.