Capillaroscopy produces in vivo images of skin microcirculation. It is a simple, noninvasive tool for analyzing microvascular abnormalities and, as such, can be used in both adults and children. Capillaroscopy has proven to be useful in many diseases, but it is of particular value in Raynaud phenomenon and other autoimmune diseases.
The test is used to analyze capillaroscopic patterns in the nailfold bed of the second to fifth fingers of each hand. A normal capillaroscopic pattern is characterized by the presence of 7 to 11 capillaries in a hairpin shape. Pathologic patterns are characterized by morphologic and structural alterations, such as ectasias, giant capillaries, pathologic hemorrhages, avascular areas, and neoangiogenesis.
In this article, we review the fundamentals of capillaroscopy, with an emphasis on the technique and its indications, diagnostic value, and use as a prognostic tool for rheumatologic disorders.
La capilaroscopia es una técnica de estudio que permite obtener imágenes directas in vivo de la microcirculación cutánea. Constituye un método accesible y no invasivo para analizar las anormalidades microvasculares, por lo que puede utilizarse en niños y adultos. En la actualidad se ha demostrado su utilidad en múltiples dolencias, principalmente en el fenómeno de Raynaud y otras enfermedades autoinmunes.
La capilaroscopia se realiza en el lecho ungueal del segundo al quinto dedo de ambas manos con la finalidad de encontrar un patrón capilaroscópico específico. El patrón de normalidad se caracteriza por la presencia de 7-11 capilares por milímetro dispuestos en forma de «U» invertida. Los patrones patológicos muestran alteraciones morfológicas y estructurales como: ectasias, capilares gigantes, hemorragias patológicas, áreas avasculares y neoangiogénesis.
En este artículo se presentan las bases de la capilaroscopia, incluyendo la técnica, las indicaciones, así como la utilidad diagnóstica y como factor pronóstico en enfermedades reumatológicas.
Capillaroscopy is a technique based on direct, in vivo imaging of skin microcirculation.1 It provides an accessible, noninvasive means of analyzing microvascular abnormalities in patients with rheumatic conditions.2 Capillaroscopy has proven useful in diseases such as systemic sclerosis, Sjögren syndrome, rheumatoid arthritis, dermatomyositis, systemic lupus erythematosus, and, in particular, Raynaud phenomenon.1
Microcirculation can be studied using several methods, the most common of which today is capillaroscopy.3 Capillaroscopy has been used an imaging technique in medicine since 1823, when Purkinje described capillaries after observing the nailbed with a magnifying glass.2 In 1911, Lombard observed the capillaries of the nailbed using immersion oil and a microscope.2 In 1973, Maricq and LeRoy reported the advantages of this technique, as well as a series of morphological details that are currently known as the capillaroscopic patterns found in systemic sclerosis.4
Principles of MicrocirculationThe main function of microcirculation is to exchange oxygen and nutrients for delivery to the tissues, as well as to eliminate carbon dioxide and waste products.5
The vasculature and microcirculation consist of the smallest vessels in the body, namely, arterioles, capillaries, and venules. The capillaries are composed of an arterial branch, a capillary loop, and a venous branch.5 The arterial branch is narrower than the venous branch by a ratio of 1:1.2-1.5.2 This pattern is found in all the organs of the body except the liver, the spleen, and the bone marrow.
TechniqueCapillaroscopy can be performed using a low-magnification lens (×20) or a high-magnification lens (×200). Low-magnification lenses provide a panoramic image of the microcirculation, whereas high-magnification lenses enable better visualization of the capillaries and their morphological characteristics.6 The main low-magnification optical instruments are the stereomicroscope, the dermatoscope, and the ophthalmoscope. Videocapillaroscopy provides a panoramic image and enables active visualization and magnifications of up to ×100, ×200, and ×600.6 The development of computerized systems, specifically nailfold videocapillaroscopy, makes it possible to visualize and analyze a single capillary, and to subsequently analyze the same capillary at different time points, with high reproducibility. Furthermore, it can digitally store images of excellent quality and provide printed reports with the Images.7 Another advantage of the videocapillaroscope is its optical probe, which can be placed in direct contact with the nailfold, thus enabling the study of patients with severe joint contractions.5,6 Capillaroscopy only enables visualization of capillary structure, whereas with videocapillaroscopy, we can observe functional and morphological changes and hemorheological dynamics.8
The patient must be relaxed and remain seated at a temperature of 20-22°C for the 15minutes preceding the study.9 In addition, patients must refrain from smoking for 24hours before the examination 9and must not undergo cosmetic procedures (manicure, gel or acrylic nails) during the 3 weeks before the examination.5 The nailfolds must be clean, without perionyxis or nail polish.9
The patient is placed with his/her hands on a surface at the level of the heart. A drop of immersion oil is applied on the nailfold to increase the transparency of the skin. All the fingers except the thumbs are examined. Each finger must be observed at ×50 to examine the architecture and then at ×200-300 to observe the morphological characteristics.5 Visualization is optimal for the folds of the fourth and fifth fingers thanks to the transparency of the skin.9
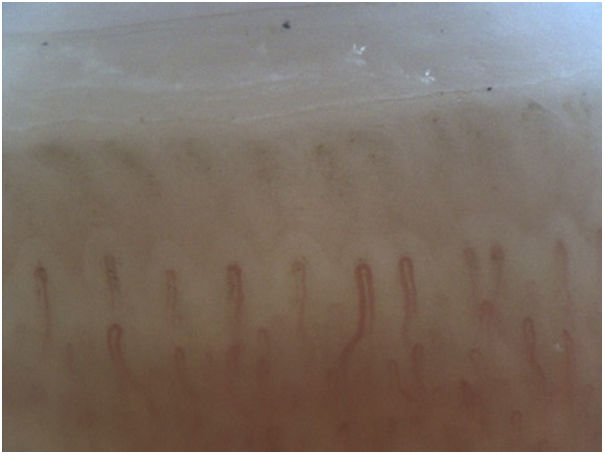
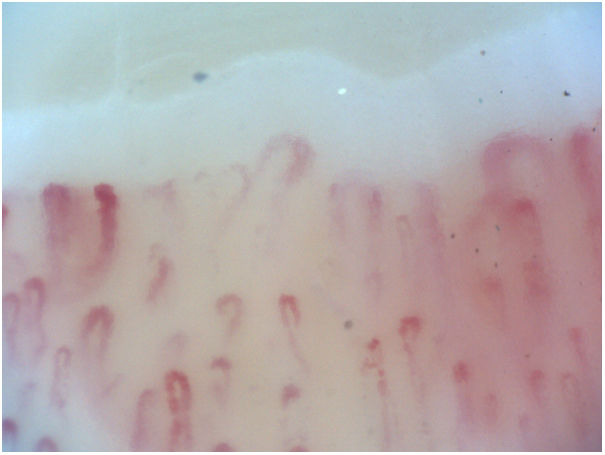
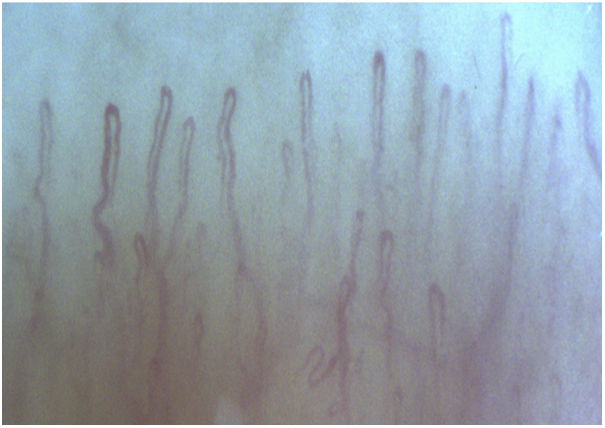
Normal Capillaroscopy PatternThe periungual capillaries in a healthy person have a regular architecture in the shape of in inverted U or hairpin with a uniform distribution and diameter.1 They form a semicircle that accompanies the nail matrix with a red color over a clearer base, which is known as conserved polarity.8 Between 7 and 17 capillaries per linear millimeter is considered normal. The capillaries have 2 branches—an afferent branch (arteriole) and an efferent branch (venule)—and a transitional zone. The branches are parallel to each other, without crossing over or overlapping 8(Figure 1). The subpapillary venous plexus can be observed in 10%-30% of healthy persons.
Preserved microvascular function consists of the following: absence of bleeding and exudates, clear visualization of structures without interference, and preserved perfusion, that is, uninterrupted flow that is uniformly red in color in the blood column.8 There should be no megacapillaries or diffuse loss of capillaries in healthy persons.
Abnormal capillaroscopy findings are observed in up to 10% of healthy persons; therefore, isolated abnormalities do not indicate disease.9 Capillaroscopy reveals moderate heterogeneous morphological changes in primary Raynaud phenomenon, although these are not clinically signficant.3
The 3 morphologically “normal” capillaroscopy patterns in healthy persons are as follows: (1) the normal pattern, with 2-5 U-shaped loops/mm and<2 tortuous loops/mm; (2) the perfect normal pattern, with >5 U-shaped loops/mm; and (3) the unusual normal pattern, with at least 1 meandering or bushy loop or at least 1 microhemorrhage or with >4 crossed loops/mm10.
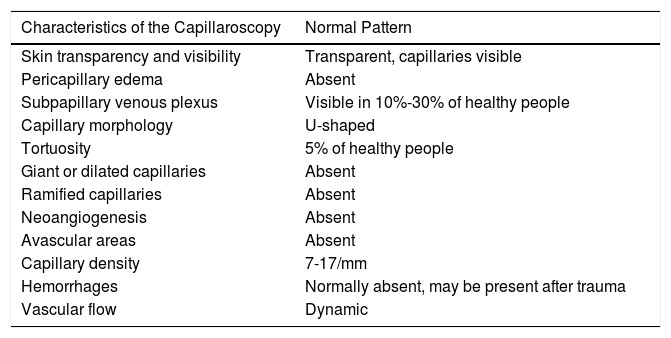
Table 1 summarizes the characteristics of a normal capillaroscopy pattern.
Characteristics of a Normal Capillaroscopy Pattern.
| Characteristics of the Capillaroscopy | Normal Pattern |
|---|---|
| Skin transparency and visibility | Transparent, capillaries visible |
| Pericapillary edema | Absent |
| Subpapillary venous plexus | Visible in 10%-30% of healthy people |
| Capillary morphology | U-shaped |
| Tortuosity | 5% of healthy people |
| Giant or dilated capillaries | Absent |
| Ramified capillaries | Absent |
| Neoangiogenesis | Absent |
| Avascular areas | Absent |
| Capillary density | 7-17/mm |
| Hemorrhages | Normally absent, may be present after trauma |
| Vascular flow | Dynamic |
Modified from Chojnowski et al.5
Capillary abnormalities are characterized by an increase in morphological or structural variations, with an increase in the size of the capillaries and a gradual decrease in their density.3
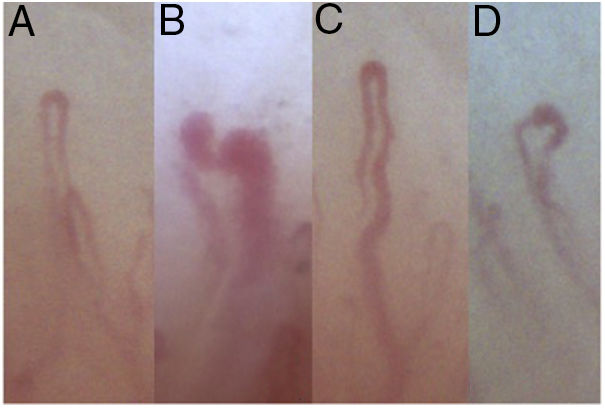
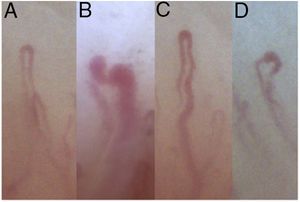
We can identify a diverse range of individual capillary abnormalities within abnormal capillaroscopy patterns or those that are nonspecific and not associated with a specific disease. Abnormalities of this type were described by Cutolo et al.11 The most common are presented below (Figure 2).
The number of capillaries and their morphological characteristics make it possible to describe specific capillaroscopy patterns that can help classify disease and provide information on prognosis and outcome.3
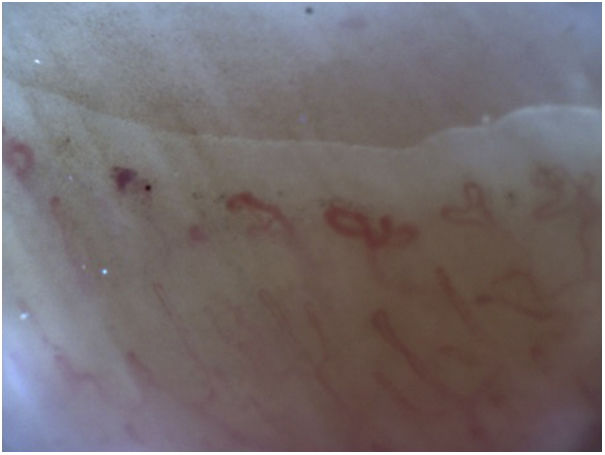
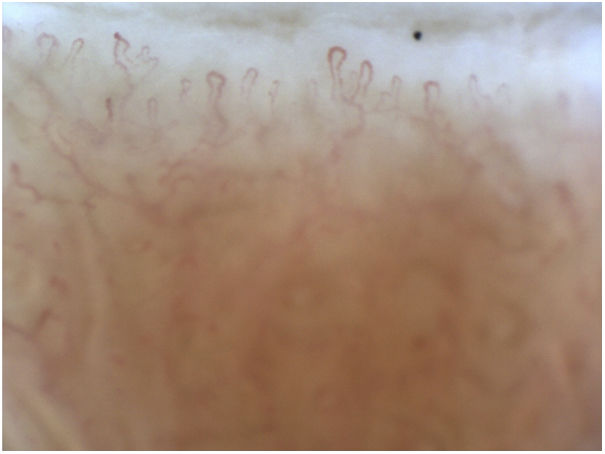
Tortuous PatternThe tortuous pattern is characterized by meandering, tortuous, or corkscrew capillaries.12 In tortuous capillaries, the afferent and efferent loops intersect at ≥2 points.13 The pattern is confirmed when the abnormality is present in at least 10% of all vessels observed. The superficial venous plexus is usually visible in this pattern.
This abnormality is found mainly in rheumatoid arthritis, psoriasis,12 and systemic lupus erythematosus, where it is more characteristic 9,12(Figure 3).
Scleroderma PatternThe scleroderma pattern is the best-defined and most specific pattern.3 It is found in systemic sclerosis (80%-100% of patients), in dermatomyositis (55%-100%), and in mixed connective tissue disease (54%-63%).9,12
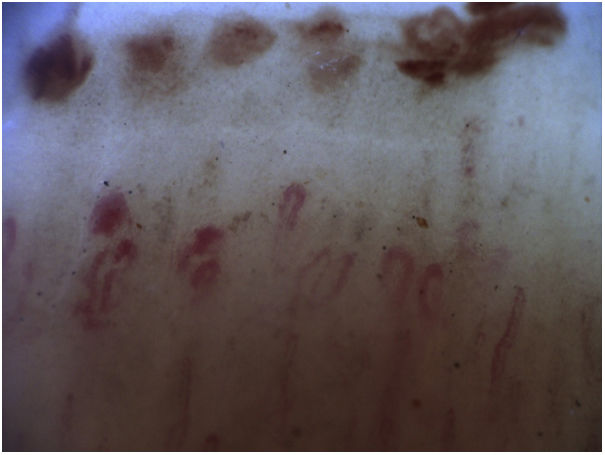
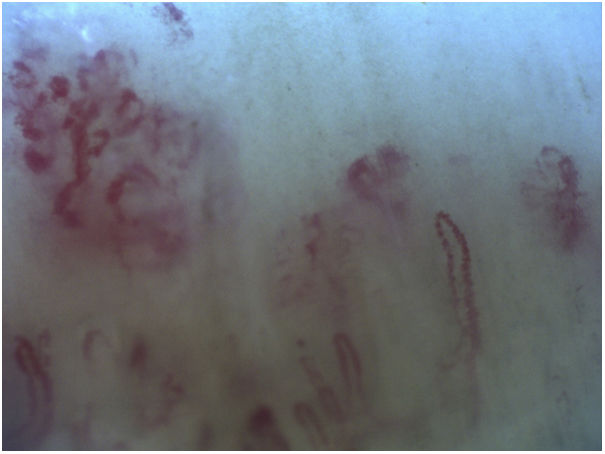
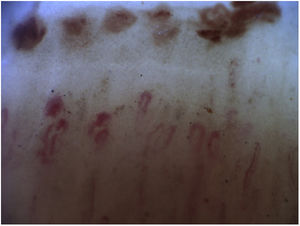
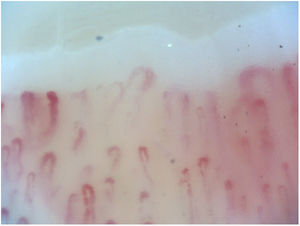
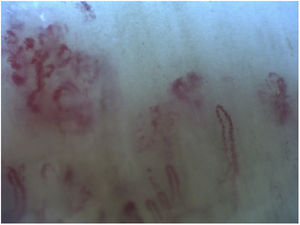
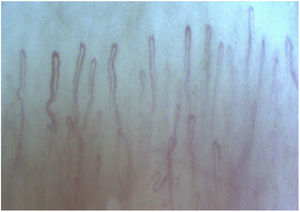
The microvascular abnormalities of systemic sclerosis were classified by Cutolo et al.11 into 3 different patterns: the early pattern (few giant capillaries, few capillary hemorrhages with no evident loss of capillaries, and well-preserved capillary distribution) (Figure 4); the active pattern (frequent giant capillaries, frequent capillary hemorrhages, and moderate loss of capillaries, as well as few/absent ramified capillaries, with some disorganization of the capillary architecture) (Figure 5); and the late pattern (few/absent giant capillaries and microhemorrhages with severe loss of capillaries with extensive avascular areas, ramified capillaries, and intense disorganization) (Figure 6).
In patients with dermatomyositis and mixed connective tissue disease, an additional finding is the presence of bushy capillaries, which are ramified capillaries that are typical of neoangiogenesis.12
Capillaroscopy in Rheumatic DiseaseThe main indications for capillaroscopy are primary Raynaud phenomenon and Raynaud phenomenon secondary to rheumatic disease, early detection of systemic scleroderma or sclerodermatous syndromes, dermatomyositis, systemic lupus erythematosus, Sjögren syndrome, vascular syndromes, and mixed connective tissue disease. The study should be performed annually. In the case of rapidly progressing systemic scleroderma, the study should be performed every 4-6 months.9
Raynaud Phenomenon and Systemic SclerosisRaynaud phenomenon is thought to be an exaggerated vasospastic response to cold or emotions. The classic response comprises blanching of the fingers (ischemic phase), bluish color (deoxygenation), and erythema (reperfusion).14
Raynaud phenomenon is the first clinical sign of abnormal systemic vascular tone. Capillaroscopy makes it possible to monitor the progression of microangiopathy, study severity, and establish the risk of an aggressive outcome.15 It has proven effective, enabling us to distinguish between the primary form and the form that is secondary to a connective tissue disease with involvement of the microcirculation.16
Secondary Raynaud phenomenon usually appears at an older age, with intense, asymmetric, and painful episodes leading to ischemic lesions of the skin. It is associated with positive specific antibody titers and capillaroscopy abnormalities, revealing the presence of connective tissue diseases.15,17
The observation of an early scleroderma pattern in association with the presence of specific antibodies (anticentromere and antitopoisomerase) and Raynaud phenomenon guides the diagnosis of systemic sclerosis in the early phase. An association has been observed between peripheral vascular compromise in systemic sclerosis and the active scleroderma pattern with digital ulcers. The late scleroderma pattern with frequent avascular areas has been identified as a prognostic factor for mortality in patients with systemic scleroderma.8
The importance and use of capillaroscopy has increased over time. For example, abnormal capillaroscopy findings were included in the diagnostic criteria for systemic sclerosis in 2013.18
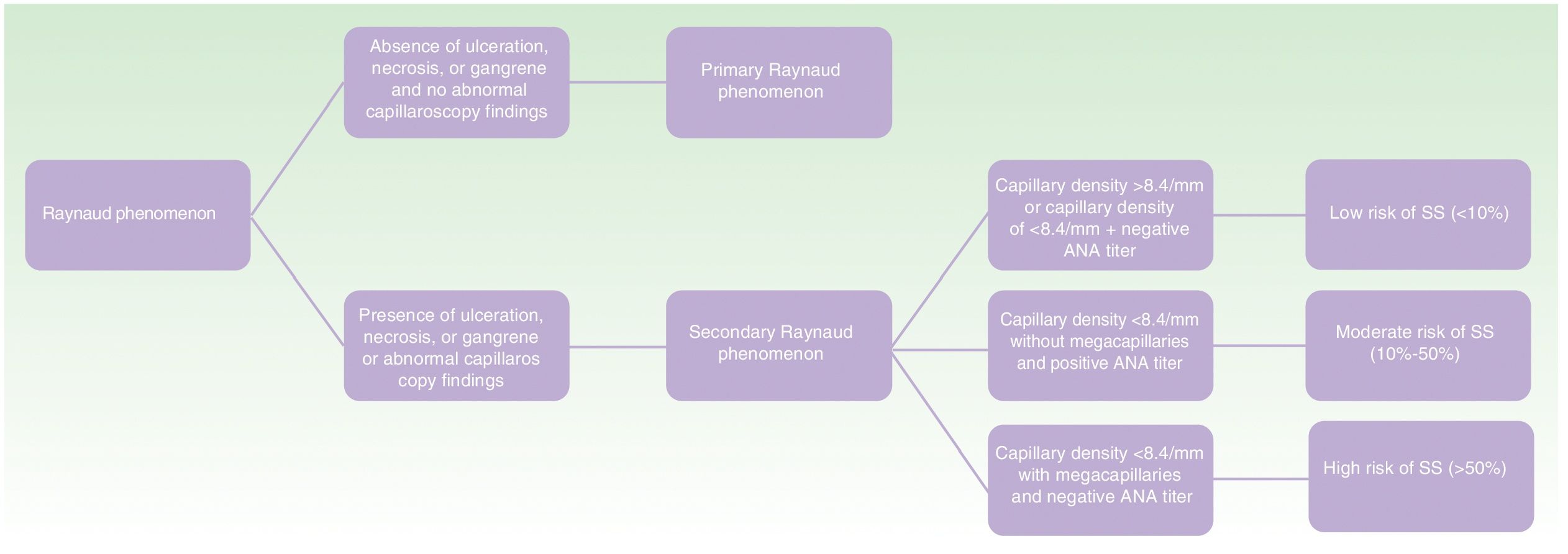
Ingegnoli et al.10 developed an algorithm summarizing the risk of developing systemic sclerosis in patients with abnormal capillaroscopy findings and positive specific antibody titers 13(Figure 7).
Mixed Connective Tissue DiseaseMixed connective tissue disease affects a group of patients who present characteristics of a combination of systemic autoimmune diseases, mainly lupus, scleroderma, and dermatomyositis. The most frequent symptom is Raynaud phenomenon.2
Abnormal capillaroscopy findings in mixed connective tissue disease are similar to those of scleroderma in 50% of cases, with frequent tortuous, bushy capillaries (Figure 8). Capillaroscopy has been proposed as a useful marker of activity and prognosis.3
DermatomyositisAbnormal nailfold capillaroscopy findings are recorded in 70% of patients with dermatomyositis.9 In more than 60%-80% of cases, the abnormal findings are similar to those of systemic sclerosis.19 Microvascular findings are similar in classic and in paraneoplastic, amyopathic, and juvenile dermatomyositis.8
The diagnosis of dermatomyositis is based on at least 2 of the following characteristics: megacapillaries, capillary loss, disorganization of the capillary array, bushy capillaries, tortuous capillaries, and hemorrhages 1(Figure 9).
There is a positive correlation between the scleroderma pattern and interstitial lung disease. Microthrombosis is associated with poor prognosis.8
Systemic Lupus ErythematosusSystemic lupus erythematosus does not involve specific microvascular alterations. In fact, the capillaroscopy pattern is normal in 30% of cases; therefore, normal findings do not rule out disease.8 Abnormal capillaroscopy findings are more frequent in patients with systemic lupus erythematosus associated with Raynaud phenomenon, anti–U1 ribonucleoprotein antibodies,20 or anticardiolipin antibodies.9
The most typical capillaroscopy abnormalities include the presence of a tortuous pattern (corkscrew capillaries). Other abnormalities, such as capillary dilation and prominent subpapillary venous plexus, have also been reported 9(Figure 10). The presence of major capillary abnormalities points to a severe clinical course.11
Rheumatoid ArthritisThe presence of an extensively visible subpapillary venous plexus with capillary hemorrhages has been reported in rheumatoid arthritis. The loops are usually filiform and increased in length 3,5(Figure 11).
The most noticeable abnormalities are in patients whose condition co-occurs with Raynaud phenomenon, multiple joint involvement, or antinuclear antibodies with positive rheumatoid factor.8
It is important to remember that many diseases involve microvascular abnormalities; these range from rheumatic diseases such as Sjögren syndrome and antiphospholipid syndrome to psoriasis, diabetes, and hypertension. The capillaroscopy patterns of each of these conditions are currently under study.8
ConclusionNailfold capillaroscopy is a rapid, noninvasive, safe, and inexpensive technique that enables us to assess the skin microcirculation. It has proven useful in the timely detection and prognosis of rheumatic diseases.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ocampo-Garza SS, Villarreal-Alarcón MA, Villarreal-Treviño AV, Ocampo-Candiani J. Capilaroscopia: una herramienta diagnóstica valiosa. Actas Dermosifiliogr. 2019;110:347–352.