Subcutaneous lesions may be detected during follow-up of patients with melanoma. The main entities that should be contemplated in the differential diagnosis in such cases are in-transit and regional lymph node metastases. We describe 2 cases of women with breast implants who developed palpable subcutaneous lesions in the axillary region during follow-up of melanoma. In both cases, the ultrasound study showed diffuse hyperechoic signals forming the characteristic snowstorm sign in the subcutaneous tissue. Ultrasound proved to be a key diagnostic tool for ruling out melanoma-related disease, such as in-transit metastases and regional lymph node metastases.
Durante el seguimiento de pacientes con melanoma podemos detectar lesiones subcutáneas cuyo principal diagnóstico diferencial son las metástasis en tránsito o las adenopatías metastásicas. Se describen 2 mujeres con melanoma portadoras de prótesis mamarias que presentaron durante su seguimiento lesiones subcutáneas palpables en la región axilar. El estudio ecográfico puso de manifiesto en ambos casos la existencia de imágenes hiperecogénicas difusas en «tormenta de nieve» localizadas en el tejido subcutáneo. En estos casos la ecografía se posiciona como herramienta diagnóstica fundamental para el despistaje de procesos relacionados con el melanoma, como las metástasis en tránsito o las adenopatías metastásicas.
Nodules or subcutaneous masses may be detected during follow-up of patients with melanoma. In such cases, in-transit and regional lymph node metastases tend to be the first suspected diagnoses. Although a series of clinical and histologic risk factors that support this likely diagnosis have been identified,1,2 in many cases further tests must be carried out, leading to a longer diagnostic delay and greater anxiety in the patient. In such cases, ultrasound can play an important role in helping to establish a diagnosis.
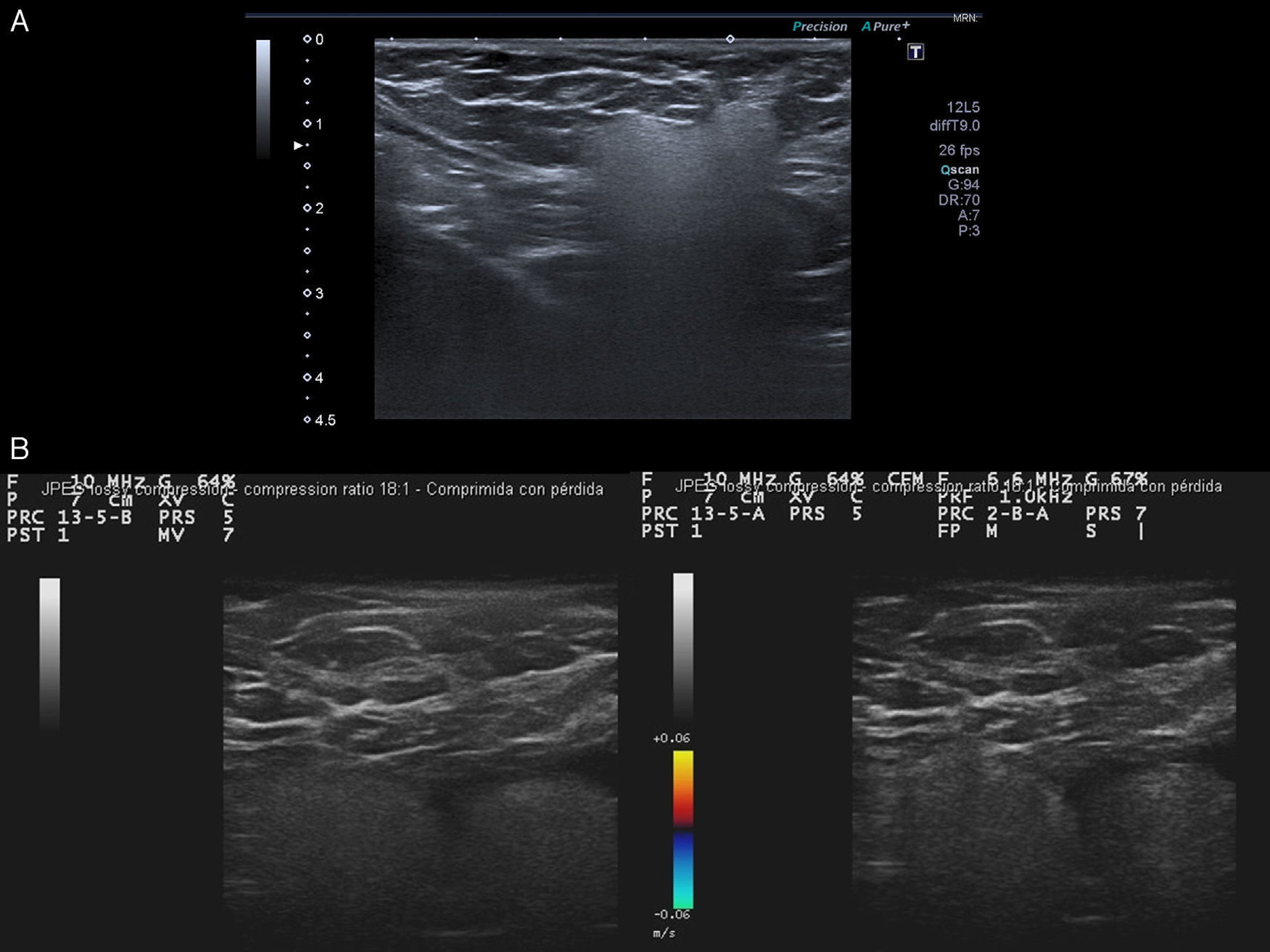
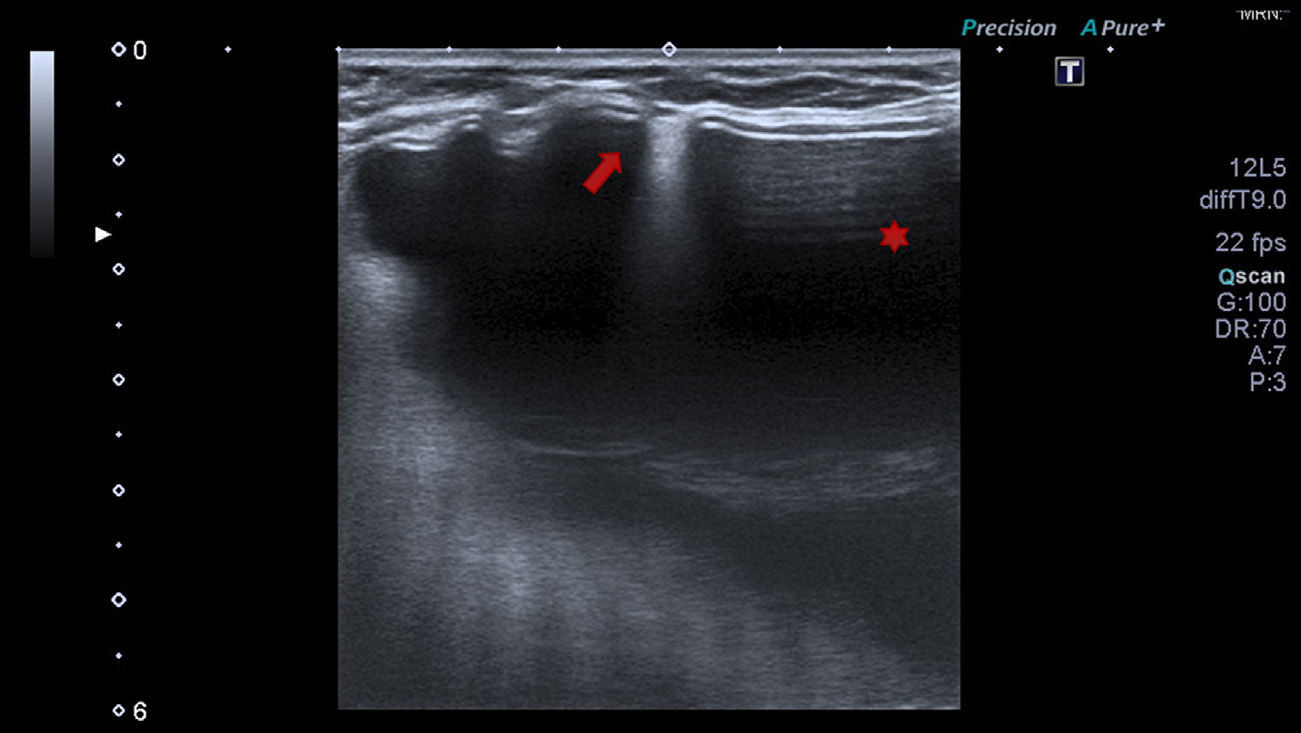
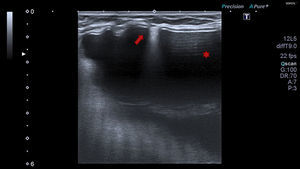
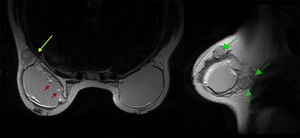
Case Description 1The patient was a 49-year-old woman with a history of dorsal melanoma on the left side in stage IA, according to the classification of the American Joint Committee on Cancer (AJCC), in 2006. In January 2014, she reported finding a palpable mass in the left axilla. Physical examination revealed a firm, subcutaneous, nodular lesion approximately 2cm in diameter that was not attached to the underlying tissue. On the basis of a suspicion of regional lymph node metastasis, the patient was referred to the diagnostic radiology department for an ultrasound study (Toshiba Aplio 500, multifrequency 7-11MHz linear probe). The ultrasound showed diffuse hyperechoic images in the subcutaneous tissue with a maximum diameter of 2cm and poor sound transmission (Fig. 1A). This ultrasound image has been described as a “snowstorm” pattern and is highly suggestive of silicone granuloma caused by breast implant rupture. As the image was very striking, a breast ultrasound was carried out immediately. The ultrasound revealed extravasated gel in the space between the fold of the outer shell of the implant and the fibrous capsule surrounding the implant. This finding confirmed the capsular rupture of the left breast implant (Fig. 2). The patient's medical history confirmed that she had received Poly Implant Prothèse (PIP) implants in 2008.
A, Kidney-shaped hyperechoic image in the subcutaneous cellular tissue with a homogeneous echostructure, a sharp upper border and sides, and a loss of the lower border due to the “snowstorm” artifact. B, Two adjacent hyperechoic images pseudoencapsulated in a “snowstorm” pattern in the subcutaneous tissue. Color Doppler imaging shows no vascularization.
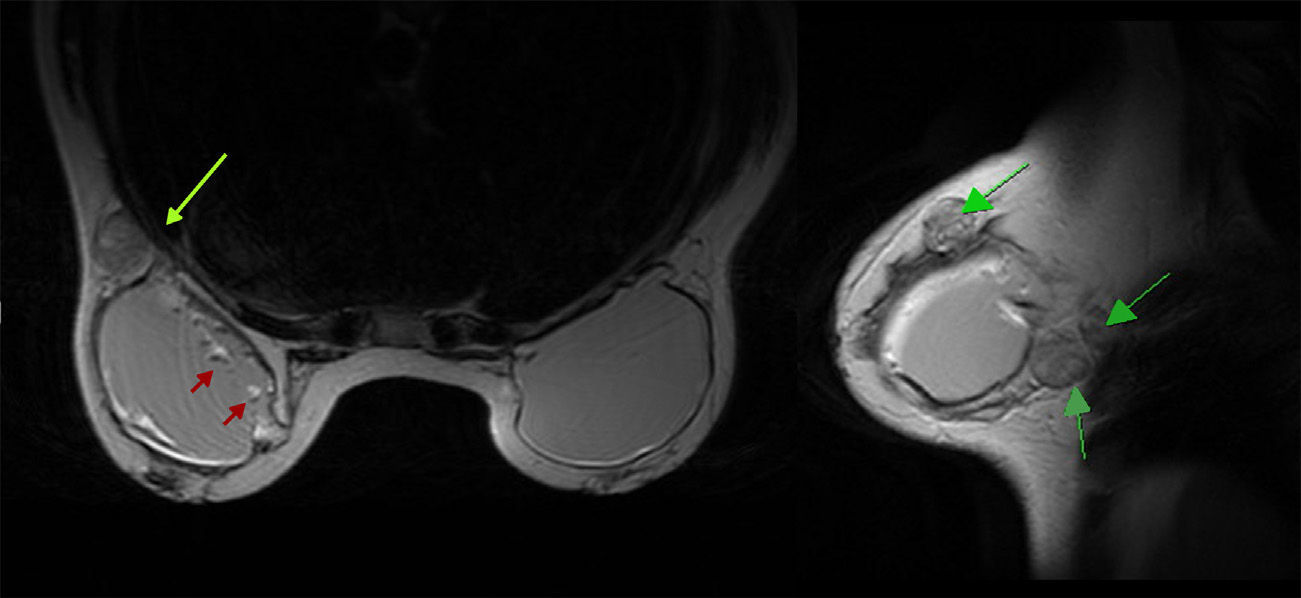
The patient was a 46-year-old woman with a history of AJCC stage IB dorsal melanoma on the left side in 2013. A palpable subcutaneous mass of elastic consistency, approximately 4cm in diameter, was detected in the left axillar region during follow-up. On the basis of a suspicion of lipoma, an ultrasound was carried out (Esaote MyLab 25, 10MHz linear probe). The ultrasound revealed a diffuse hyperechoic image with a “snowstorm” pattern in the subcutaneous tissue, with a maximum diameter of 5cm (Fig. 1B). The patient confirmed having received PIP implants in 2002. She underwent a magnetic resonance imaging (MRI) study of the breast, which revealed a capsular rupture of the left breast implant and silicone granulomas in the axilla and around the implant (Fig. 3).
In both cases, the implants were removed and replaced with new ones, and the silicone granulomas were excised. The procedures were performed in private hospitals because Spain's national health system only covers implant removal, not replacement.
DiscussionPalpable nodules and subcutaneous masses detected during follow-up in patients with melanoma are a major diagnostic challenge because of their prognostic implications. Histopathologic analysis of the lesions is usually necessary in order to establish a diagnosis. In such cases, ultrasound is a noninvasive diagnostic tool that provides information in real time that can aid in decision-making. In the case of melanoma, the main suspected diagnoses of subcutaneous lesions are in-transit and regional lymph node metastases. In ultrasonography, in-transit metastases appear as round, oval, or lobular hyperechoic images in the subcutaneous tissue with well-defined borders, and color Doppler imaging reveals a variable degree of vascularization.3 Although there are no consensus criteria for radiologic diagnosis of regional lymph node metastases in melanoma, most studies have applied the Berlin criteria: peripheral perfusion as an early sign of metastasis; loss of central echoes accompanied by, or subsequent to, peripheral perfusion, which displaces the cancerous growths from the center to the periphery; and balloon-shaped lymph nodes with total loss of central echoes, which is a major sign of lymph node involvement and, consequently, a late sign of metastasis.4
In our patients, the ultrasound showed diffuse hyperechoic images with a “snowstorm” appearance in the subcutaneous tissue. These ultrasound findings are characteristic of silicone granulomas. Silicone granulomas consist of a foreign body granulomatous infiltrate in the lymph nodes caused by silicone migration following the rupture of a breast implant.5,6 Although complications associated with breast implants are rare, in 2011 the French Health Safety Agency prohibited the sale and use of PIP implants7 on the grounds that they contained industrial silicone unsuitable for use in humans and had lower levels of biocompatibility and biodurability than conventional implants.8 In fact, the rupture prevalence rate after 10 years is 24% for PIP implants, compared with 10% for conventional implants.9 In 2012, the Spanish Ministry of Health estimated that 18 500 women in Spain had PIP prostheses a that a total of 37 000 devices had been implanted. In 40% of cases, women received the implants between the ages of 30 and 44 years—a range that overlaps with the age of highest melanoma incidence in Spanish women. Therefore, the biggest problem associated with silicone granuloma is differentiating between this condition and breast cancer and axillary metastases.
The US Food and Drug Administration recommends that all women with implants should undergo MRI screening for silent rupture 3 years after implantation and every 2 years after that.10 Chung et al.11 compared MRI screening to ultrasound screening. The authors found that the sensitivity and specificity of ultrasound for detecting rupture were, respectively, 82% and 81% in symptomatic women and 64% and 77% in asymptomatic women, whereas the sensitivity and specificity of MRI were, respectively, 85% and 90% in symptomatic women and 78% and 71% in asymptomatic women. From a clinical and economic point of view, the optimal strategy is to use ultrasound screening in symptomatic women—because the procedure is diagnostic in most cases—and also in asymptomatic women, and to limit the use of MRI to doubtful cases.
Ultrasound diagnosis of implant rupture is an operator-dependent technique that requires experience, and therefore it is not an objective of the dermatologist. However, the dermatologist should be able to identify ultrasound findings characteristic of silicone granulomas. The presence of diffuse hyperechoic nodules with a “snowstorm” pattern is highly suggestive of silicone granuloma and completely different from the appearance of subcutaneous or regional lymph node metastases.
In the event of PIP implant rupture, removal and replacement is the consensus treatment recommendation, according to the website of the Spanish Ministry of Health, Social Services and Equality. Although the Ministry's website does not directly mention silicone granulomas, it does indicate that, in the event of signs of failure of a PIP implant, the implant should be removed and replaced and any resulting complications should be treated.12
Given the recent increase in the number of women with breast implants—as well as the total number of devices implanted—an increase in the prevalence of silicone granulomas is to be expected. Therefore, subcutaneous lesions in melanoma patients with breast implants should prompt a high index of suspicion. In such cases, cutaneous ultrasound is a noninvasive diagnostic tool that can help to rule out other lesions—such as cutaneous or regional lymph node metastases—in real time.
Ethical DisclosuresProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for the purpose of this study.
Data confidentialityThe authors declare that they followed their hospitals’ regulations regarding the publication of patient information.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández Canedo MI, Blázquez Sánchez N, Valdés Solís P, de Troya Martín M. Siliconomas axilares en pacientes con melanoma. Actas Dermosifiliogr. 2016;107:e23–e26.