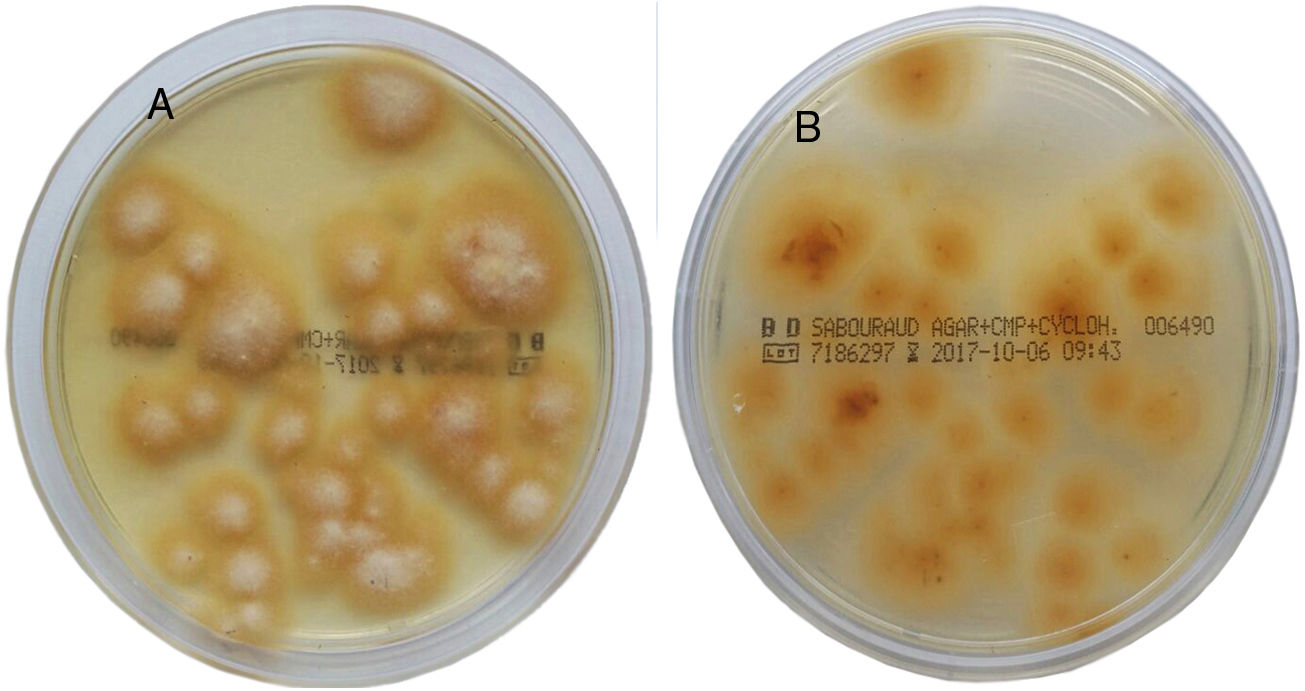
A 9-year-old boy was assessed because of an erythematous plaque next to the left eye, with micropustules and peripheral scaling (Fig. 1). The lesion had been present for 2 months. A sample was taken for direct examination and another sample for fungal culture by scraping the edge of the lesion with a scalpel and wad of sterile cotton wool. In direct microscopic examination of the sample, with potassium hydroxide 20% and dimethyl sulfoxide 40%, mycelia consistent with a dermatophytic fungus were observed. Scales from the lesion were cultured on Sabouraud chloramphenicol actidione agar plates. After 7 days, flat colonies with a starburst-like pattern at the edge had grown, with a bright yellow color on the front and reverse side of the colony (Fig. 2A and B). A powdery white superficial mycelium developed with light radial folds at the center of the colonies (Fig. 2A). The fungus hydrolyzed urea (Christensen and Maslen urea broth) after 7 days and sporulation did not present on the dextrose potato agar plate after 21 days of incubation. With a VITEK MS (matrix-assisted laser desorption/ionization time-of-flight mass spectrometry [MALDI-TOF MS], BioMérieux), Arthroderma benhamiae (99.9%) was identified after 7 days of incubation on the potato dextrose agar. Molecular identification of the microorganism was performed in the Mycology Unit of the Spanish Microbiology Center in Majadahonda.
Scale culture on Sabouraud chloramphenicol actidione agar plates for 15 days (28 °C). Flat colonies with starburst-like pattern at the edge can be observed, with a bright yellow color on the front (A) and reverse (B) side of the colony. In the middle of the colonies, a powdery white superficial mycelium developed with light radial folds.
The lesion was treated for 1 month with terbinafine cream, but follicular involvement still persisted. Finally, the infection resolved with oral terbinafine 125 mg/d for 4 weeks.
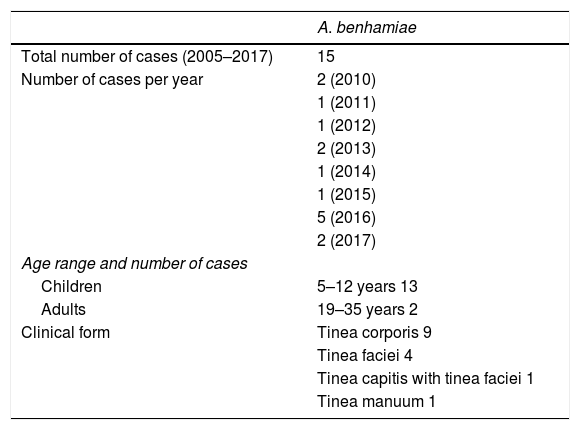
The microbiology department of our hospital has recorded 15 cases of ringworm caused by A. benhamiae between 2005 and 2017, mainly in children with transmission by guinea pigs; the first case was in 2010 (Table 1). As in cases reported in the literature, all were cases of inflammatory ringworm.
Summary of demographic and clinical data of ringworm caused by A. benhamiae in our center between 2005 and 2017.
| A. benhamiae | |
|---|---|
| Total number of cases (2005–2017) | 15 |
| Number of cases per year | 2 (2010) |
| 1 (2011) | |
| 1 (2012) | |
| 2 (2013) | |
| 1 (2014) | |
| 1 (2015) | |
| 5 (2016) | |
| 2 (2017) | |
| Age range and number of cases | |
| Children | 5–12 years 13 |
| Adults | 19–35 years 2 |
| Clinical form | Tinea corporis 9 |
| Tinea faciei 4 | |
| Tinea capitis with tinea faciei 1 | |
| Tinea manuum 1 | |
Dermatophytic fungi are usually identified using conventional techniques based on macroscopic and microscopic morphology, although in some cases, absence of sporulation and morphological similarities between species requires identification using molecular techniques or the use of MALDI-TOF MS. In the present case, MALDI-TOF MS was used for identification due to the absence of fungal sporulation in the culture media. MALDI-TOF MS is a widely used technique in the field of bacteriology. The technique is based on obtaining a protein profile of the isolate and comparing this with a database. The use of this technique has expanded to mycology, with results equivalent to DNA sequence analyses, provided that the reference spectra for the species to be identified are included in the library used.1A. benhamiae is represented in the commercial library (V3) of the VITEK MS, which enabled its identification with a concordance of 99.9%.
A. benhamiae, basionym (or previously denominated) Trichophyton benhamiae, is an emerging dermatophytic fungus that causes zoonotic epidemics from infected pets.2–5 Since 2002, there have been reports of inflammatory ringworm such as tinea corporis and faciei (more frequently), and tinea capitis and Kerion celsi. Onychomycoses are rare. In Japan, where the first cases were reported, contagion occurs through rabbits, rodents, and white-bellied hedgehogs, all of which are popular pets in that country. In Germany, guinea pigs are the main source of contagion.5 The fungus has also been isolated from dogs and cats. Children and adolescents are the individuals most often affected, and cases in immunosuppressed individuals may also occur. The fungus can be confused macroscopically with Microsporum canis (yellow colonies) and microscopically with Trichophyton mentagrophytes/Trichophyton interdigitale (rounded conidia and urea hydrolysis), and so its incidence may be underestimated if not correctly identified. Even so, in some regions of Germany, it may already be the most widespread zoophilic dermatophyte.5 In tinea capitis caused by A. benhamiae or extensive infections, oral terbinafin is the treatment of choice, followed by fluconazole or itraconazole,5 although few studies are available. Griseofulvin has also been used. The minimum duration of treatment is usually 4–6 weeks. For other types of lesions, topical antimycotic agents used in other dermatophytoses can be used, such as terbinafine, imidazoles, and ciclopirox.
It is likely that the incidence of this dermatophytic fungus will increase, and so dermatologists should bring themselves up to date regarding relevant clinical and epidemiological aspects, methods of identification, and potential diagnostic errors.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Lozano-Masdemont B, et al. Arthroderma benhamiae, un dermatofito causante de una tiña emergente. Actas Dermosifiliogr. 2020;111:167–168.