Chlamydia trachomatis genital infection is common in our setting and early treatment can prevent complications. The aim of this study was to report on patients diagnosed with C trachomatis genital infection in a sexually transmitted disease (STD) clinic.
Material and methodsThis was a descriptive, cross-sectional, observational study of patients diagnosed with C trachomatis infection between 2010 and 2011. We recorded demographic data and information on sexual habits, concomitant sexually transmitted infections (STIs), and various aspects of treatment.
ResultsIn total, 12.3% of the samples analyzed were positive for C trachomatis genital infection. Sixty-two patients (43 men) with a mean age of 31 years were studied; 75% were heterosexual and 87% had had a sexual partner in the previous 2 months. Condom use was inconsistent in 81%, 79%, and 65% of patients who practiced vaginal, oral, and anal sex, respectively. Thirteen percent of the patients had symptoms and anogenital warts were the most common associated STI. The most widely used treatment was doxycycline.
ConclusionsA high prevalence of genital C trachomatis infection was detected in our STD clinic, and the majority of cases were found in young men. We observed a high rate of asymptomatic infection in patients who do not engage in high-risk sexual behavior and who had come to the clinic for another reason. Systematic screening of C trachomatis infection should be implemented in STD units to enable the early treatment of patients and their recent sexual partners.
La infección genital por Chlamydia trachomatis (CT) tiene una alta incidencia en nuestro medio y su tratamiento precoz puede evitar complicaciones. Describimos la población de pacientes diagnosticados en una consulta de enfermedades de transmisión sexual.
Material y métodosEstudio observacional descriptivo de corte transversal de la población diagnosticada de infección por CT entre 2010 y 2011. Se recogieron datos demográficos, hábitos sexuales, asociación con otras infecciones de transmisión sexual (ITS) y diversos aspectos del tratamiento.
ResultadosEncontramos positividad para CT en el 12,3% de las muestras. Se incluyeron 62 pacientes con una media de edad de 31 años. De estos 43 eran hombres y el 75% era heterosexual. El 87% de los pacientes había tenido una pareja sexual en los últimos 2 meses. El uso del preservativo se consideró deficiente en el 81, 79 y 65% de los pacientes en el sexo vaginal, oral y anal respectivamente. Aparecieron síntomas en el 13% y la ITS asociada con más frecuencia fueron las verrugas anogenitales. El tratamiento más usado fue la doxiciclina.
ConclusionesLa detección de CT en nuestra consulta es elevada, procediendo en su mayoría las muestras de varones jóvenes. Demostramos una alta incidencia de infección genital asintomática por CT en pacientes sin prácticas sexuales de alto riesgo y que acudieron a la consulta por otros motivos. Es necesario el despistaje sistemático de CT en la consulta de ITS para tratar de forma precoz al paciente y a sus parejas recientes.
Genital chlamydia, which is caused by Chlamydia trachomatis, is the most common sexually transmitted infection (STI) in Europe. In 2009, 343958 cases were reported in 23 member countries of the European Union, including Spain.1C trachomatis infection is also the main notifiable STI in our health district (unpublished data). Because most infections are mild and asymptomatic, patients do not generally seek medical attention. Spanish groups have been warning about the need for a standardized screening program for C trachomatis infection in STI clinics for years.2 Persistent infections in women can cause pelvic inflammatory disease, infertility, and ectopic pregnancies.3 Early detection of cervical infections in women have proven to be effective in reducing complications.4 In men, chlamydia mainly affects the urethra and while it is associated with few complications, there is a high risk of the infection being spread to female partners.5 The true prevalence of C trachomatis infection and associated risk factors is unknown in Spain and has been investigated in just a few studies.6 The aim of this study was to determine the prevalence of C trachomatis infection in patients seen at an STI clinic run by the dermatology department of a public hospital in the south of Spain (Costa del Sol Occidental) and to describe the risk profile of patients diagnosed with this infection.
Material and MethodsThis was a descriptive, observational, cross-sectional study of patients diagnosed with chlamydia at an STI clinic between January 2010 and December 2011. The clinic forms part of Hospital Costa del Sol in Malaga, Spain, which serves a population of 387 036 inhabitants according to the municipal census of the Spanish National Statistics Institute. All patients seen at the clinic were evaluated and those who tested positive for urethral, cervical, or rectal C trachomatis at any time during follow-up were included in the study. Patients who did not consent to their data being collected were excluded. We recorded information on sexual preferences and habits using a questionnaire that is completed as part of the routine sexual history taken at the clinic. Diagnosis was established using the artus polymerase chain reaction kit (C. trachomatis Plus RG PCR Kit for use with QIAsymphony SP/AS and Rotor-Gene Q Instrument, QIAGEN). Urethral and cervical samples were tested in men and women respectively, and rectal samples were tested in men and women with a recent history of anal sex. We also recorded the clinical characteristics of infection, the presence of other sexually transmitted diseases, and different aspects of treatment. We performed a descriptive analysis using measures of central tendency and dispersion for quantitative variables and distribution of frequencies for qualitative variables.
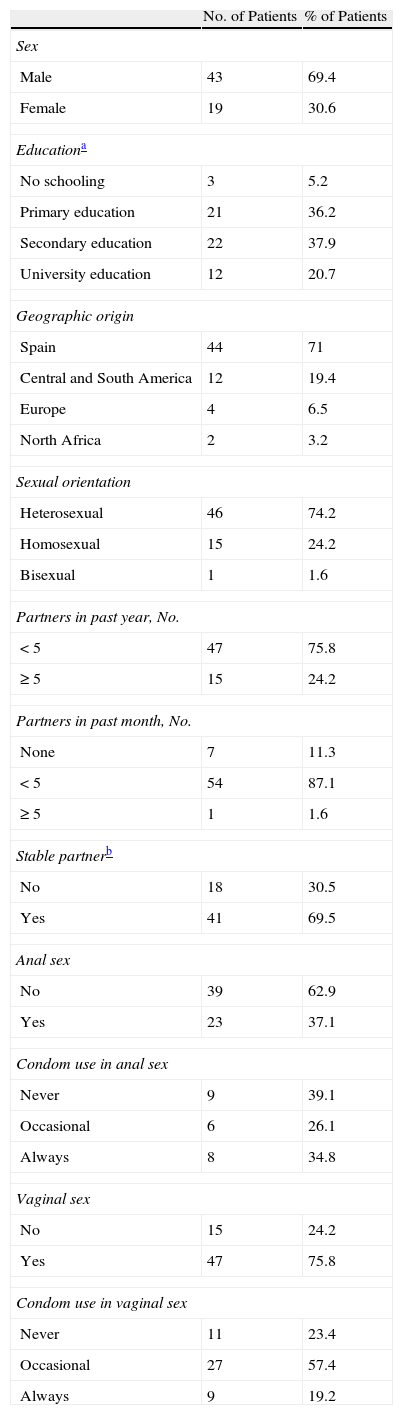
ResultsIn total, 729 samples (388 urethral, 181 cervical, and 160 rectal) were collected from 560 patients during the study period; 90 samples (12.3%) were positive for C trachomatis infection in 78 patients. Of these patients, 62 (43 men and 19 women) correctly completed the questionnaire and were included in the study. Their mean age was 30.8 years (95% CI, 28.4-33.3) and most of the patients were of Spanish origin (71%) and white (82.3%). Ninety-five percent of patients had completed some level of education (lower than university level in 79.3% of cases) (Table 1). The most common professions were in the hotel, restaurant, and catering industry.
Sociodemographic Characteristics and Sexual Behavior.
| No. of Patients | % of Patients | |
| Sex | ||
| Male | 43 | 69.4 |
| Female | 19 | 30.6 |
| Educationa | ||
| No schooling | 3 | 5.2 |
| Primary education | 21 | 36.2 |
| Secondary education | 22 | 37.9 |
| University education | 12 | 20.7 |
| Geographic origin | ||
| Spain | 44 | 71 |
| Central and South America | 12 | 19.4 |
| Europe | 4 | 6.5 |
| North Africa | 2 | 3.2 |
| Sexual orientation | ||
| Heterosexual | 46 | 74.2 |
| Homosexual | 15 | 24.2 |
| Bisexual | 1 | 1.6 |
| Partners in past year, No. | ||
| <5 | 47 | 75.8 |
| ≥5 | 15 | 24.2 |
| Partners in past month, No. | ||
| None | 7 | 11.3 |
| <5 | 54 | 87.1 |
| ≥5 | 1 | 1.6 |
| Stable partnerb | ||
| No | 18 | 30.5 |
| Yes | 41 | 69.5 |
| Anal sex | ||
| No | 39 | 62.9 |
| Yes | 23 | 37.1 |
| Condom use in anal sex | ||
| Never | 9 | 39.1 |
| Occasional | 6 | 26.1 |
| Always | 8 | 34.8 |
| Vaginal sex | ||
| No | 15 | 24.2 |
| Yes | 47 | 75.8 |
| Condom use in vaginal sex | ||
| Never | 11 | 23.4 |
| Occasional | 27 | 57.4 |
| Always | 9 | 19.2 |
Seventy-five percent of the patients were heterosexual and 25% reported having had more than 5 sexual partners in the past year. Eighty-seven percent of those evaluated had had at least 1 sexual partner in the past 2 months, and 70% had a stable partner at the time of diagnosis. Condom use was inconsistent in 81% of those who engaged in vaginal sex, 79% of those who engaged in oral sex, and 65% of those who engaged in anal sex (Table 1).
None of the patients reported working as sex workers injecting drugs, or exchanging sex for drugs. Two men stated that they had paid for sex in the past year.
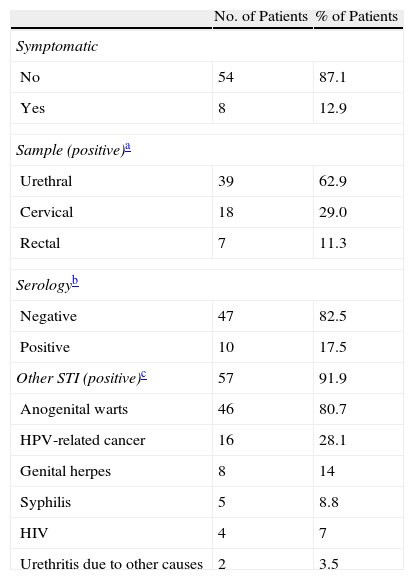
Thirteen percent of patients had chlamydia-related symptoms. Thirty-nine (90.7%) of the 43 men had a positive urethral sample and 6 of these (15.4%) had symptoms of dysuria and urethral discharge. One of the 18 women with a positive cervical sample had symptomatic cervical discharge. Genetic material of C trachomatis was isolated in the rectum of 4 men who have sex with men (MSM) and 3 heterosexual women, all of whom were asymptomatic. Ten (17.5%) of the 57 patients who tested positive for chlamydia and underwent serology had antibodies to C trachomatis; in 80% of cases, the antibodies were immunoglobulin M. None of the patients developed complications during the study period (Table 2).
Clinical Results.
| No. of Patients | % of Patients | |
| Symptomatic | ||
| No | 54 | 87.1 |
| Yes | 8 | 12.9 |
| Sample (positive)a | ||
| Urethral | 39 | 62.9 |
| Cervical | 18 | 29.0 |
| Rectal | 7 | 11.3 |
| Serologyb | ||
| Negative | 47 | 82.5 |
| Positive | 10 | 17.5 |
| Other STI (positive)c | 57 | 91.9 |
| Anogenital warts | 46 | 80.7 |
| HPV-related cancer | 16 | 28.1 |
| Genital herpes | 8 | 14 |
| Syphilis | 5 | 8.8 |
| HIV | 4 | 7 |
| Urethritis due to other causes | 2 | 3.5 |
Abbreviations: HIV, human immunodeficiency virus; HPV, human papillomavirus; STI, sexually transmitted infection.
Eighty-one STIs were identified in the patients studied, and 92% of patients had at least 1 other STI: 46 (80.7%) had anogenital warts, 16 (28.1%) had human papillomavirus (HPV)–related cancers, 8 (14%) had genital herpes, 5 (8.8%) had syphilis, and 2 (men) (3.5%) had urethritis caused by other pathogens. Five patients (7%) were positive for human immunodeficiency virus (HIV) infection (Table 2).
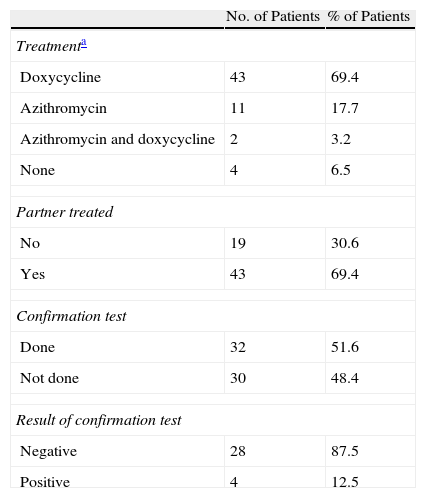
The most common treatment (used in 69.4% of cases) was doxycycline 100mg every 12hours for a week. Treatment was not administered in 4 patients for different reasons. Following the protocol at our clinic, all the patients were provided with information and medication for recent identifiable sexual partners. We determined that in 43 cases (69.4%), at least 1 partner received the information and was treated. Of the 32 patients who were retested after 3 months, 4 were still positive for C trachomatis infection (Table 3).
Treatment.
| No. of Patients | % of Patients | |
| Treatmenta | ||
| Doxycycline | 43 | 69.4 |
| Azithromycin | 11 | 17.7 |
| Azithromycin and doxycycline | 2 | 3.2 |
| None | 4 | 6.5 |
| Partner treated | ||
| No | 19 | 30.6 |
| Yes | 43 | 69.4 |
| Confirmation test | ||
| Done | 32 | 51.6 |
| Not done | 30 | 48.4 |
| Result of confirmation test | ||
| Negative | 28 | 87.5 |
| Positive | 4 | 12.5 |
We detected a high rate of C trachomatis infection at our STI clinic; those infected were largely young, white adult men of Spanish origin. Our assessment of risk factors for infection revealed that while a high percentage of patients were heterosexual and had had just 1 sexual partner (generally a stable one) in the previous month, condom use was low. In most cases, patients were tested for C trachomatis infection as part of routine testing of asymptomatic patients who came to the clinic for another STI (primarily anogenital warts).
Genital C trachomatis infection is the main STI reported in our health district, with 238 notifications in 2 years. This is approximately twice the number of reported cases for syphilis and 5 times that for gonococcal infections. C trachomatis infection was the most common notifiable disease reported in the United States in 2008.7 Additionally, it was detected in 7% of women aged between 15 and 24 years seen at family planning clinics between 2004 and 20088 and in 8.3% of women in the same age group in their first term of pregnancy seen at prenatal clinics.9 The prevalence of chlamydia in sexually active men and women has been estimated at around 4% in some Spanish regions.6 International clinical guidelines recommend testing for C trachomatis in sexually active women under 25 years of age,10 women in their first term of pregnancy,11 and men under 25 years of age.12 Efficient screening programs in young women have proven successful in preventing complications due to C trachomatis.3,4,13 Testing for chlamydia in STI clinics is justified due to the high prevalence of the infection and the fact that treatment can reduce complications.
We did not identify any particular risk groups related to race, educational level, or former residence in a developing country in our series. Studies in Europe14 and the United States15 have shown C trachomatis infection to be more common in black women, women from poor countries, and women with a lower level of education. The risk of chlamydia in young adults has been linked to inconsistent condom use6,16 and an increased number of sexual partners in the preceding 3 months.16 In our study, we did not find a high number of recent partners, and we assume that the infection was picked up from the patient's current partner, indicating low condom use.
In line with the findings of most studies,17 the majority of patients with C trachomatis infection in our series were asymptomatic. The most common associated STIs in our series were HPV infections. Genital HPV infections are the main reason for referral to our clinic and do not necessarily indicate high-risk sexual behavior.
Rectal samples were positive for C trachomatis infection in 4 MSM and 3 women who engaged in anal sex. A high prevalence of rectal C trachomatis infection in patients who have had recent receptive anal intercourse has been reported in both women18 and men.19 Diagnosis and treatment is crucial in such cases to control the spread of infection and reduce the risk of HIV infection in MSM.20
Both doxycycline and azithromycin have proven effective in treating chlamydia, but the former is considered superior for the treatment of rectal infections.21 Risk of reinfection in the year after diagnosis can be as high as 20%,22 and repeat testing is therefore recommended 3 to 12 months after diagnosis.23 Patient-delivered partner treatment is an effective measure for reducing risk of reinfection.24 The reinfection rate in our series is similar to reports in the literature, even though appropriate treatment was delivered and partner notification was high.
While nucleic acid amplification tests have high specificity and sensitivity, bacterial culture is the most reliable method for identifying genital C trachomatis infection. It is, however, expensive and only available at certain reference hospitals. It should be noted that most of the patients we analyzed came to our STI clinic with another infection (mostly genital warts), and this is an obvious source of selection bias.
We detected a high rate of C trachomatis infection in the population seen at our STI clinic. Considering the high prevalence and asymptomatic nature of C trachomatis infection, routine screening for chlamydia should be performed in all patients who consult for an STI at such clinics, regardless of their risk profile, which is generally low. We believe that routine C trachomatis testing should be extended to all at-risk individuals seen at health centers and gynecological clinics.
Further studies of the general population are needed to determine the true prevalence of C trachomatis infection. The identification of infection and treatment of both patients and their partners is key to preventing complications and transmission.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purpose of this study.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Repiso-Jiménez JB, Fernandez-Morano T, Rivas-Ruiz F, de Troya-Martin M. Análisis de la población con infección genital por Chlamydia trachomatis en una consulta de enfermedades de transmisión sexual. Actas Dermosifiliogr. 2014;105:774–779.