To date, reports on alopecia in patients with palmoplantar pustulosis (PPP) are rarely seen. We herein describe four cases of alopecia in patients with PPP.
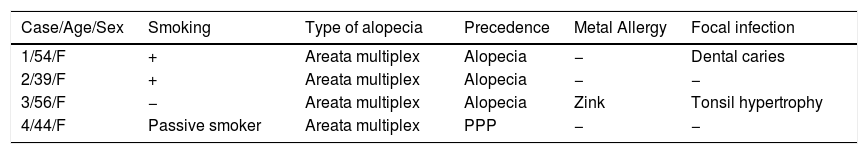
During these 10 years, we diagnosed 128 patients with PPP (M:F=1:2) in our department. Among these patients, four patients had PPP and alopecia (3.1%). All of the patients were female, and the age range was from 39 to 56 years old (Table 1). Three patients developed alopecia prior to the onset of PPP, and the remaining patient developed alopecia 10 years after the onset of PPP. Two patients had pustulotic arthro-osteitis. Two patients were smokers, and one was a passive smoker. A metal patch test was carried out in all cases. Three patients showed no reaction, while one patient showed a positive reaction (+) to zinc according to the criteria of the International Contact Dermatitis Research Group. Regarding the type of alopecia, all patients presented with alopecia areata multiplex. Severe types of alopecia involving sites other than the scalp, such as the eyelashes and eyebrows, were not observed. Representative figures are shown in Fig. 1. Laboratory examination did not reveal positive antinuclear antibodies and thyroid abnormalities. Examination of focal infection was performed in all cases, in which dental caries and tonsil hypertrophy were observed each in one case. All cases were conservatively treated for alopecia. Topical immunotherapy with squaric acid dibutylester (SADBE) was applied in one case (Case 1), while the other cases were treated with topical corticosteroid or carpronium chloride lotion. Among four patients, Case 1 was resistant while others were relatively responsive to topical therapies for alopecia.
Characteristics of four patients with PPP and alopecia areata.
| Case/Age/Sex | Smoking | Type of alopecia | Precedence | Metal Allergy | Focal infection |
|---|---|---|---|---|---|
| 1/54/F | + | Areata multiplex | Alopecia | − | Dental caries |
| 2/39/F | + | Areata multiplex | Alopecia | − | − |
| 3/56/F | − | Areata multiplex | Alopecia | Zink | Tonsil hypertrophy |
| 4/44/F | Passive smoker | Areata multiplex | PPP | − | − |
F: female; PPP: palmoplantar pustulosis
Thyroiditis, diabetes mellitus, hyperlipidaemia, and psychiatric disorders are sometimes accompanied by PPP. By contrast, There is a limited number of reports on autoimmune skin disorders such as vitiligo and alopecia. Previously, Nakamura et al. reported a patient with PPP, alopecia totalis and Hashimoto's thyroiditis.1 In their case, the alopecia was severe with involvement of the total scalp, eyebrow, and eyelashes, suggesting immunological interplay among PPP, alopecia, and thyroid disorders. By contrast, our four patients showed a common type of alopecia areata multiplex. Both alopecia and PPP are occasionally associated with autoimmune thyroiditis; however, autoimmune thyroiditis was not detected in any of our patients.
Similar to psoriasis, IL-23/IL-17 inflammatory pathway has recently been suggested to be important in PPP. IL-17 and IL-22 are detected close to or in the acrosyringium of PPP skin lesions, and increased serum levels of both cytokines.2 The etiology of alopecia areata is complicated, and recent studies have suggested Th1 dominance, Th2 dominance, and Th17 involvement.3,4 It is known that psoriasis and alopecia mutually exert exclusive local effects, e.g. the protective effect of psoriatic lesions against hair loss.5 This Renbök phenomenon is speculated to occur due to a local balance of different Th1/Th2/Th17 subsets which amplify self-sustaining cytokines while suppressing alternative pathways. Most likely, the immune balance may depend on the disease stages, such as initial and progressive phases, or associated diseases such as atopic dermatitis, autoimmune diseases, and connective tissue disorders. In conclusion, alopecia associated with PPP may be overlooked, and thus more attention should be paid to alopecia in the clinical examination of PPP.
Please cite this article as: Hiraiwa T, Yamamoto T. Alopecia areata y pustulosis palmoplantar: informe de 4 casos. Actas Dermosifiliogr. 2018;109:751–752.