In the hospital setting, dermatologists are often required to evaluate inflammatory skin lesions arising during surgical procedures performed in other departments. These lesions can be of physical or chemical origin. Povidone iodine is the most common reported cause of such lesions. If this antiseptic solution remains in contact with the skin in liquid form for a long period of time, it can give rise to serious irritant contact dermatitis in dependent or occluded areas. Less common causes of skin lesions after surgery include allergic contact dermatitis and burns under the dispersive electrode of the electrosurgical device. Most skin lesions that arise during surgical procedures are due to an incorrect application of antiseptic solutions. Special care must therefore be taken during the use of these solutions and, in particular, they should be allowed to dry.
Dentro del ámbito hospitalario no es infrecuente que los dermatólogos debamos valorar lesiones cutáneas inflamatorias que surgen en intervenciones quirúrgicas realizadas por otros servicios. Estas lesiones pueden ser de causa física o química. La povidona yodada es la causa descrita más frecuentemente de aparición de estas lesiones. Este antiséptico, si permanece en solución en contacto con la piel durante un periodo prolongado, puede ocasionar dermatitis irritativas graves en zonas declives u ocluidas. Otras causas menos frecuentes son dermatitis alérgicas de contacto o quemaduras en el terminal de toma de tierra del bisturí eléctrico. Debido a que la mayor parte de estas lesiones se debe a una aplicación incorrecta del antiséptico, deben extremarse sus normas de uso, especialmente dejándolo secar de forma adecuada.
Interdepartmental consultations, including both the requests from other specialties for the dermatologic evaluation of patients and those made by dermatologists to colleagues in other specialties, form a very important part of dermatologic practice. The hospital is one of the main environments in which interdepartmental dermatologic consultations occur, usually in the form of a written consultation request.1,2 In this environment, one of the clinical problems that we may be asked to evaluate is that of a patient with inflammatory lesions after a surgical intervention.3
Analysis of the ProblemAcute skin lesions that arise as a result of a surgical intervention can be of physical or chemical origin.3,4 Physical causes include burns and lesions due to traction, friction, or pressure, while the mechanisms underlying lesions produced by contact with a chemical product may be irritant or allergic. Finally, as in any hospitalized patient, the differential diagnosis must always include infections and drug reactions; the clinical correlates of such lesions differ from those of lesions arising during surgical procedures and do not fall within the scope of this article.
A number of aspects must be taken into account in the initial evaluation of a patient with acute postsurgical skin lesions. The first is to determine the sequence of appearance of the lesions. It is not uncommon for patients to spend a significant time in the emergency room, where they may undergo limb traction or have prolonged contact with antiseptics or chemical debriding agents before the surgical intervention. We must also consider the possibility of lesions developing during the patient's stay in the postoperative recovery room, or that the lesions were present previously and the operation merely led the surgeon or nurse responsible for the patient to notice them. Finally, the patient may have developed similar lesions during other operations or following contact with other medical devices, which would suggest a possible allergic mechanism.
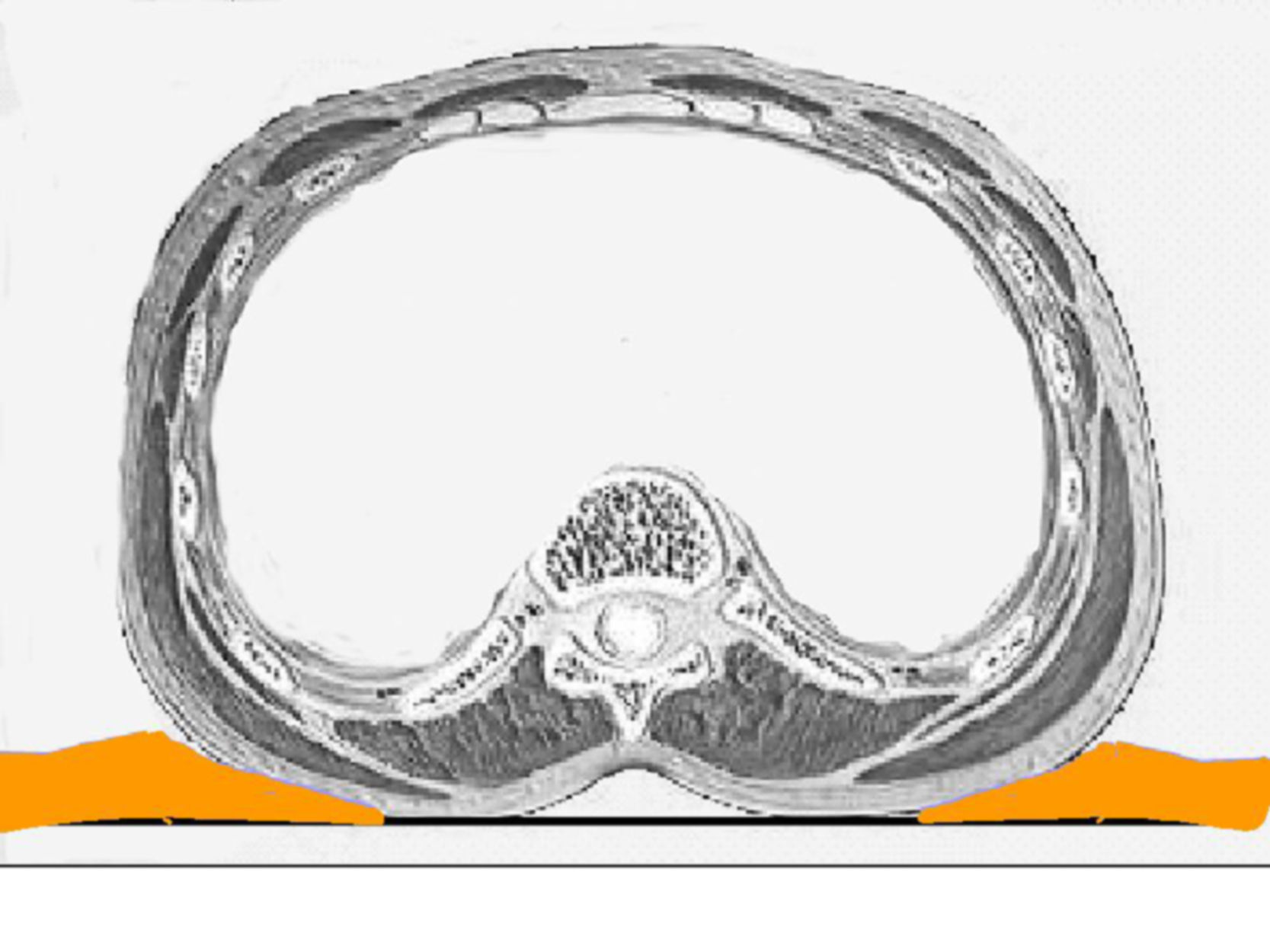
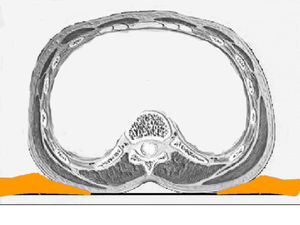
For lesions that arise during a surgical intervention or in the immediate postoperative period, the first characteristics that we must evaluate are the site of the lesions, their morphology, and their relationship to the surgical wound. Lesions in dependent areas and signs of dropping figures would suggest a liquid has played a role (Fig. 1), while an annular or rectangular morphology could suggest the electrocardiography pads or the dispersive electrode of an electrosurgical device (Fig. 2). Finally, lesions around the surgical incision may be due to antiseptics or to the dressings used before, during, or immediately after the operation.
Other factors that can affect the appearance of lesions are the use of occlusive plastic dressings (Fig. 3), the antiseptic solution employed in the surgical field, and the care applied up to the time of consultation. All the procedures on the patient must be tracked from entering the surgical area until transfer to the ward. A record should also be made of the type and duration of the operation, the position in which the patient was placed for the intervention, and any changes to this position during the course of the procedure. If a burn is suspected, the use of an electrosurgical device and the electrical frequency employed must be evaluated. Sometimes it may even be necessary to take into consideration the antiseptics used to clean the operating table and surgical drapes. Finally, we must always determine whether the lesion is a sporadic event or if there are other patients with similar lesions.
Lesions of Physical OriginLesions produced by heat are associated with the use thermal warming blankets and warming lamps. These are rare and may be due to poorly calibrated devices, a defect, or inappropriate use.5 Such lesions occur in very long operations, as the skin surface can tolerate temperatures of 44°C for up to 6hours.3
Other types of burns are caused by the electrosurgical device. A serious conflagration can occur if an electrical spark ignites intestinal gases or the vapor from alcohol-based antiseptic solutions.4 These 2 situations are very rare and are clearly surgeon-related.6 Another type of thermal burn is one produced under the dispersive electrode of the electrosurgical device used in high-frequency mode. These lesions can develop when the electrode becomes impregnated with a fluid (blood, saline solution used for lavage, or antiseptic solution). Activation of the electrosurgical device causes the solution to vaporize, producing the burn.4,7 A further possible source of burns is disruption of the circuit of the electrical device used to produce hemostasis. When working with a high-frequency electrical device, a poorly or only partially adherent dispersive electrode will cause the current to run through a different site with less electrical resistance. In this situation, if the patient's skin is in contact with a material that offers low electrical resistance, such as areas of moisture or metallic objects, the current will flow through these points and may cause burns.8 The area of the sacrum, where liquid can collect during an operation, is a typical site for this to occur.3 These risks are higher in minimally invasive procedures, such as laparoscopy or endovascular catheterization (Fig. 4).9 The possibility that the dispersive electrode has become detached from the skin, with the consequent increase in the risk of causing a burn, must be considered whenever the power of the electrosurgical device needs to be increased significantly during an intervention.4,10
Lesions due to prolonged pressure are very rare; they can develop in patients with arterial insufficiency and are similar to early pressure sores. Traction lesions are more common. These occur in patients undergoing orthopedic surgery, when dressings stuck directly onto the skin are used to hold a limb in traction. The shear force on the epidermis during removal of the adhesive dressing can produce blisters. A clinical finding that can help in the diagnosis of this type of lesion is that the dermatitis may be more marked around the follicles.3 Although friction dermatitis is theoretically possible as a concept, it is more likely that the lesions are due to the antiseptic employed.11,12
Lesions Caused by ContactInflammatory lesions in the postoperative period can be caused by contact with various substances. The mechanism of production of the lesions is usually irritant, but it may also be allergic. Irritant contact dermatitis is one of the most common causes of in-hospital interdepartmental dermatology consultations.2 Preparation of the surgical field for the operation can alter the characteristics of the corneal layer, and this will facilitate the subsequent appearance of a dermatitis. Factors that favor the onset of acute irritant dermatitis during the operation include immobility, occlusion, maceration, the use of plastic dressings, a long surgical procedure, and the liberal use of antiseptics (Fig. 1 and Fig. 3).1 Progression along the established hospital pathway for patients undergoing surgical interventions can produce contact with 2 groups of irritant substances. First are the soaps and antiseptics used to clean the surgical table in the operating room and the stretchers for transfer; second are the antiseptics applied to the skin to prepare the surgical field. The antiseptics employed to clean operating room furniture and utensils are usually quaternary ammonium compounds, which are excellent disinfectants and are supplied for dilution in water to form soapy solutions. The irritant potential of most of these products on contact with the skin is well established and their instructions for use always indicate that direct contact with the skin should be avoided and that clinical material should be dried after cleaning with these disinfectants. However, these solutions are usually highly volatile, which reduces the risk of dermatitis. In the normal hospital pathway these substances cannot enter into contact with the skin, and cases of dermatitis will only arise when this pathway is in some way altered.
It has been clearly demonstrated that the use of antiseptics to prepare the surgical field reduces the rate of intraoperative and surgical wound infections. All the substances employed have high germicidal activity and a marked irritant potential.13 They are usually applied to the surgical field and allowed to dry by evaporation or with the aid of a swab. However, when generous amounts of these substances are used, they remain in liquid form for a long period and can give rise to acute inflammatory lesions, particularly in dependent areas or beneath plastic dressings. Additional factors that produce occlusion, or the presence of damp swabs or drapes in contact with the patient's skin, increase the risk of irritant contact dermatitis.1 Lesions that develop under these circumstances may not affect the surgical scar, which can lead to confusion as the physician may thus exclude antiseptics as the origin of the dermatitis.14,15
Although any antiseptic can cause acute irritant dermatitis if appropriate guidelines on application are not observed, povidone iodine is at present the antiseptic reported most commonly in the literature as a cause of this type of dermatitis.4,16–18 Povidone iodine is an iodophor formed of povidone, a very long-chain carbon polymer, complexed with iodine in equilibrium with the concentration of iodine in solution. Free iodine in the liquid phase has germicidal power and, as it is consumed, more iodine is released from the complex. Free iodine is irritant and, if it remains in liquid phase in contact with the skin for a long period, it can produce severe irritant lesions similar to burns or toxic epidermal necrolysis.14,16,18–20 Four lesion patterns are recognized. The first and most specific is a pattern of parallel linear lesions in the lumbar region, caused by the accumulation of the antiseptic in lateral dependent areas during long procedures (Figs. 5–7).18 The second pattern develops when povidone iodine impregnates a terminal stuck to the patient, such as the electrocardiography monitoring electrodes or the dispersive electrode. In this case, the outline of the lesion mirrors the shape of the terminal; this must be differentiated from a possible allergic contact dermatitis (Fig. 2). The third pattern occurs when the povidone impregnates the cotton wool or swabs used to protect the patient's skin from a physical device employed during the procedure. A characteristic lesion of this type is the one that develops along the border of the tourniquet cuff for limb operations. These cuffs are usually placed around the proximal part of the limb to block the blood flow (Fig. 8). Swabs and cotton wool are placed between the tourniquet and the skin; if these become impregnated with povidone iodine, lesions can develop at the borders of the cuff.4,11,12,21 The fourth recognized pattern is random and occurs in the dependent areas of the patient during the operation, with the appearance of runs caused by dripping of the liquid or impregnation of the surgical drapes (Fig. 9). As most operations are performed with the patient in the supine position, the lesions are found most commonly on the back, particularly in the sacral region.18 The differential diagnosis of postoperative inflammatory lesions in this area must include not only irritant dermatitis due to the antiseptic,15 but also burns caused by incorrect use of the electrosurgical device,4,6 as has been commented above.
In addition to their irritant potential, antiseptics used to prepare the surgical field can cause allergic contact dermatitis.22–24 In this case the area of the surgical incision is always affected and the appropriate investigations must then be performed, with patch testing to determine if the allergen is the antiseptic molecule itself, an excipient, or another substance that may have been in contact with the patient.18,25–30
During a surgical intervention, the skin comes into contact with devices and substances that can cause allergic contact dermatitis in previously sensitized patients. Although contact dermatitis due to the nickel contained in medicosurgical instruments has been reported,31–33 the alloys employed and the short period of contact during the procedure make it unlikely that lesions will be triggered by this hapten. As in all types of eczema, if a patient presents lesions in the area of contact with an object, appropriate evaluation must be performed in a contact dermatitis unit.27,28,30 Lesions that occur in the area of the dispersive electrode of an electrosurgical device or of pacemaker electrodes can be caused not only by the irritant properties of the adhesive, aggravated or not by the antiseptic employed, but also by sensitization to any of the components of the electrode or to the gels used to increase the electrical conductivity of the skin.30,34
DiscussionAlthough mild skin complications after surgical interventions have not been extensively studied, they can be relatively common. The lesions are usually transitory and are typically assumed to be inherent to the surgical procedure, both by the patient and by the medical staff.3 Even when these lesions are mild, they should be investigated and diagnosed to prevent more serious harm in the future, if the same situation arises with additional concomitant factors. However, the in-depth study of cases is usually difficult, as health staff adopt a defensive approach to any investigation that may be required. Most of the lesions occur due to an inappropriate use of the substances or devices employed and they are very rarely due to allergy or defective material.3,6,16 It is our duty as physicians to draw attention to the possible incorrect use of medical materials, thus helping to establish appropriate guidelines. A basic rule that would prevent many complications would be to ensure that the antiseptic solution dries completely before the surgical procedure is started.3,4,6,8
Adequate collaboration with our colleagues not only offers an opportunity to improve the quality of patient care, but will also bring credit to our specialty in the hospital environment.3
Ethical DisclosuresProtection of human and animal subjectsThe author declares that no experiments were performed on humans or animals for this investigation
Confidentiality of dataThe author declares that he has followed his hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe author declares that no private patient data are disclosed in this article.
Conflicts of InterestThe author declares that he has no conflicts of interest.
Please cite this article as: Borrego L. Lesiones cutáneas agudas tras intervenciones quirúrgicas. Aproximación clínica. Actas Dermosifiliogr. 2013;104:776–781.