A 34-year-old man with no relevant past medical history attended the emergency department for a mildly painful tumor with occasional bleeding on the lower gum. The patient had developed periodontitis in the adjacent molar 2 months earlier that was treated with oral antibiotics (amoxicillin plus clavulanic acid) and the lesion developed following the treatment. He reported no fever, previous ingestion of other medication, or surgery in the area.
Physical ExaminationPhysical examination revealed a firm erythematous-violaceous tumor lesion of 20 mm in diameter on the gum adjacent to the lower second right molar (Fig. 1). No other abnormalities were noted in the mouth.
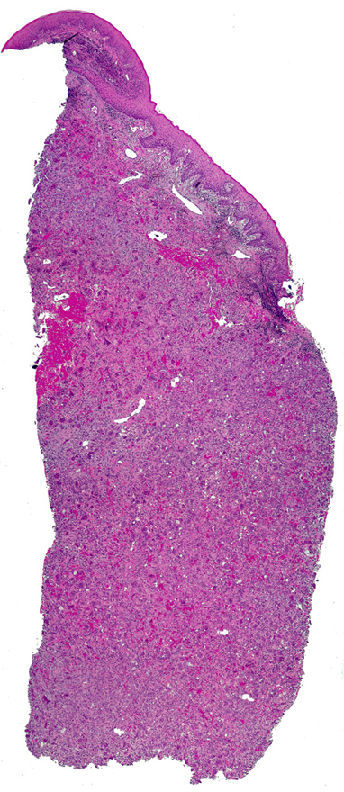
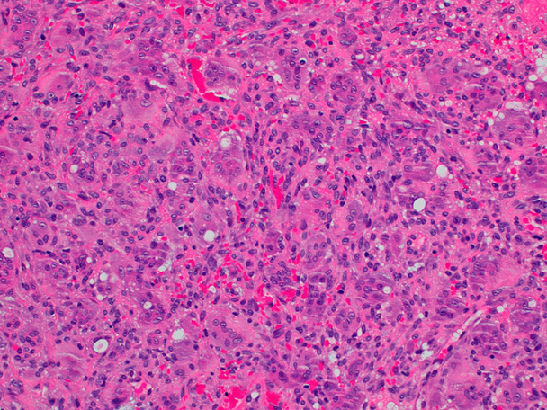
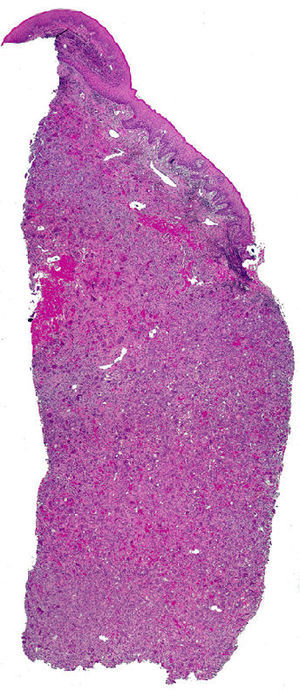
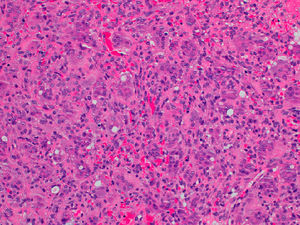
HistopathologyHistopathology revealed a gingival mucosa formed of a stratified squamous epithelium with no significant abnormalities. The superficial dermis was totally occupied by an inflammatory infiltrate characterized by a connective-tissue stroma containing numerous multinucleated giant osteoclastic cells, immature mesenchymal cells, and a mild, predominantly mononuclear infiltrate. Abundant capillaries with foci of extravasated red blood cells and hemosiderin deposits were also seen (Figs. 2 and 3).
Additional TestsOrthopantomography showed no underlying bone abnormalities. There were no significant alterations in the blood count and biochemistry, and thyroid and parathyroid hormone studies were normal.
What Is Your diagnosis?
DiagnosisPeripheral giant cell granuloma (PGCG).
Clinical CourseThe lesion was excised by the maxillofacial surgery service and the patient remained asymptomatic 6 months after surgery.
CommentIn 1953, Jaffe1 used the term “giant cell reparative granuloma” to define a form of benign reactive tumor and to distinguish it from more aggressive giant-cell tumors that appear in the metaphyses of the long bones and that can metastasize in 2% of cases. PGCG is a giant-cell epulis or giant-cell granuloma that appears in the oral cavity and consists of a smooth-surfaced erythematous-violaceous gingival tumor of rapid growth adjacent to the bone. It typically arises in the mandibular mucosa, although it can also develop in the maxillary region; there have been very rare cases in other locations such as the nasal mucosa.2 This rare disease is most common in men of less than 30 years of age, with very occasional reports in children3; it has also been described in the elderly, related to friction from dental protheses.4 These lesions are thought to occur as a reaction to infection, trauma, or constant friction.1,3,4
Clinically, the differential diagnosis should include pyogenic granuloma (which tends to be softer and more prone to bleeding), irritation fibroma (slower growing and also found at other sites, including the cheek and lips), and venous malformations of the mouth (typically present from an early age).
Histologically, PGCG is characterized by osteoclast-like multinucleated giant cells surrounded by an inflammatory infiltrate in the stroma. The differential diagnosis must therefore include central giant cell granuloma as this disease presents the same histological characteristics with the added feature of underlying bone involvement, which appears as a radiolucent area on orthopantomography.1,5 Another similar lesion is the “brown tumor” (osteoclastoma) of hyperparathyroidism and it is therefore necessary to determine the calcium, phosphorous, and parathyroid hormone levels in these patients.1
Surgery is the most widely used treatment and outcomes are good, though with some recurrences.1,5,6 Medical treatments have been published in the form of anecdotal reports or case series, above all for central giant-cell granuloma. Intralesional injection of corticosteroids tends to reduce the size of the lesion.6 Oral or intranasal calcitonin has been used with excellent results.6 Other treatments include interferon alfa, imatinib, or a combination of the two. However, there have been no comparative studies of the various treatments to determine whether they are as effective as surgical excision.6
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Nuño-González A, et al. Lesión nodular en encía de rápido crecimiento. Actas Dermosifiliogr. 2011;102:465-466.