Cutis verticis gyrata (CVG) is a rare skin condition characterized by thickening of the scalp, giving rise to convolutions and sulci, with a cerebriform pattern. CVG is classified as primary (essential and nonessential) or secondary.
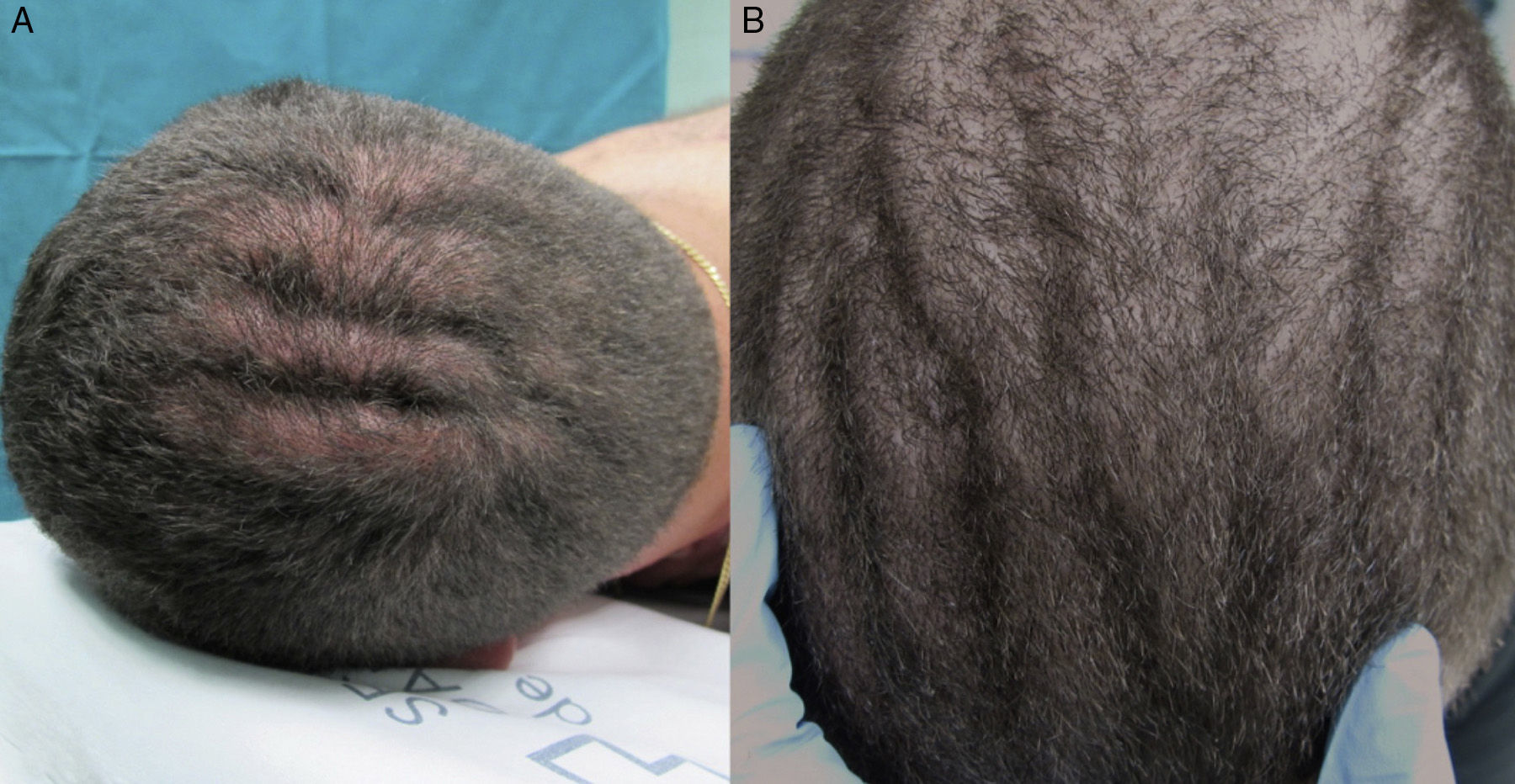
We present 2 cases of primary essential CVG in a single family. The 2 men (patients 1 and 2) were siblings of 32 and 28 years of age, with no other relevant family history. They presented progressive thickening of the scalp that had started in adolescence. Physical examination revealed anterior-posterior folds on the scalp of both patients (Fig. 1) and mild subungual hyperkeratosis and distal onycholysis of the nail plates of the great toes of both feet.
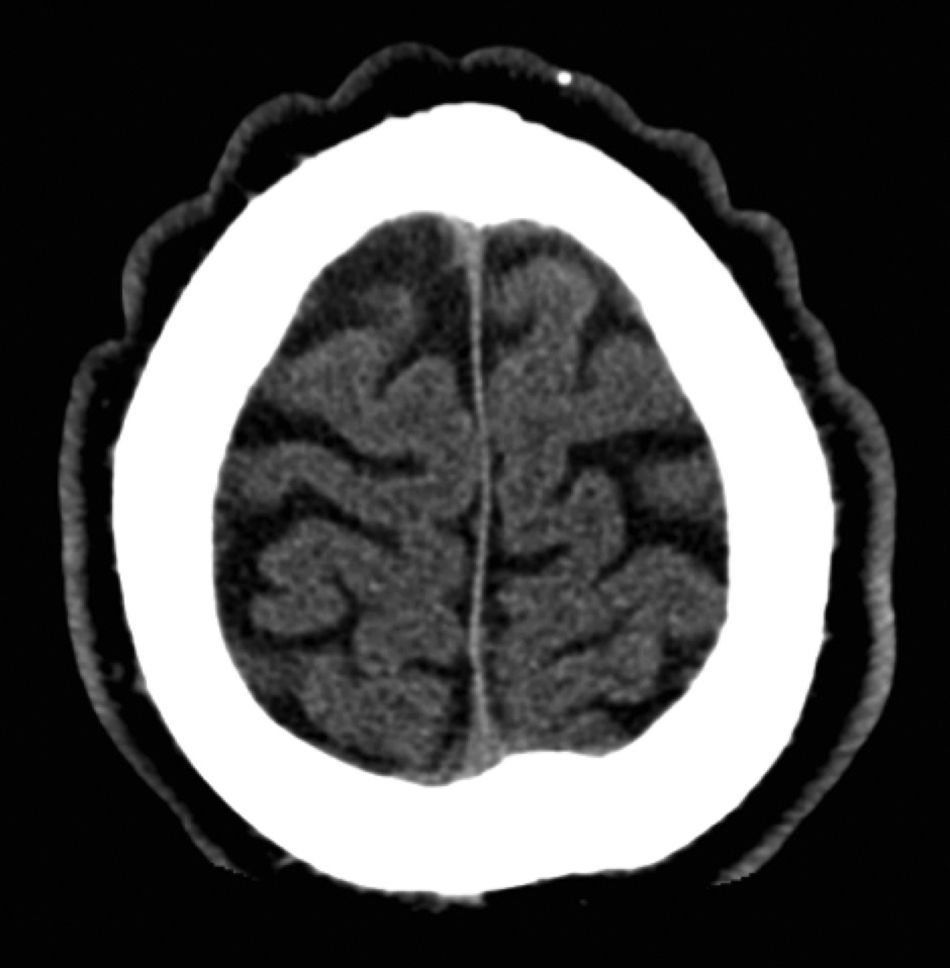
Detailed dermatologic and systemic medical history and physical examination, including endocrine and neurologic evaluation, detected none of the abnormalities associated with the primary nonessential forms. Scalp biopsy revealed a mild nonspecific superficial periadnexal and perivascular mononuclear inflammatory infiltrate in both patients. The following studies were performed to exclude causes of secondary CVG: plain x-rays of both hands, cerebral computed tomography (CT), routine blood tests with thyroid function, lipid profile, insulin-like growth factor1, antinuclear antibodies, and syphilis serology. The cerebral CT of patient 1 showed the skin folds affecting the scalp (Fig. 2). Other studies were normal or negative. Studies of the nail alterations (culture and histopathology) were only positive in patient 2 (growth of Trichophyton interdigitale), and treatment was prescribed with oral terbinafine (250mg/24h for 3 months). Genetic analysis was not performed in either patient.
Primary essential CVG is most common in postpubertal men.1 The etiology is unknown, but genetic and endocrine factors are believed to be implicated.2 The majority of cases of primary essential CVG are sporadic, although familial forms with autosomal dominant or recessive inheritance with variable expression have been reported.3,4 The prevalence data for the general population date from 1964, with an estimated prevalence among men and women of 1 and 0.026 cases per 100000 population, respectively.5
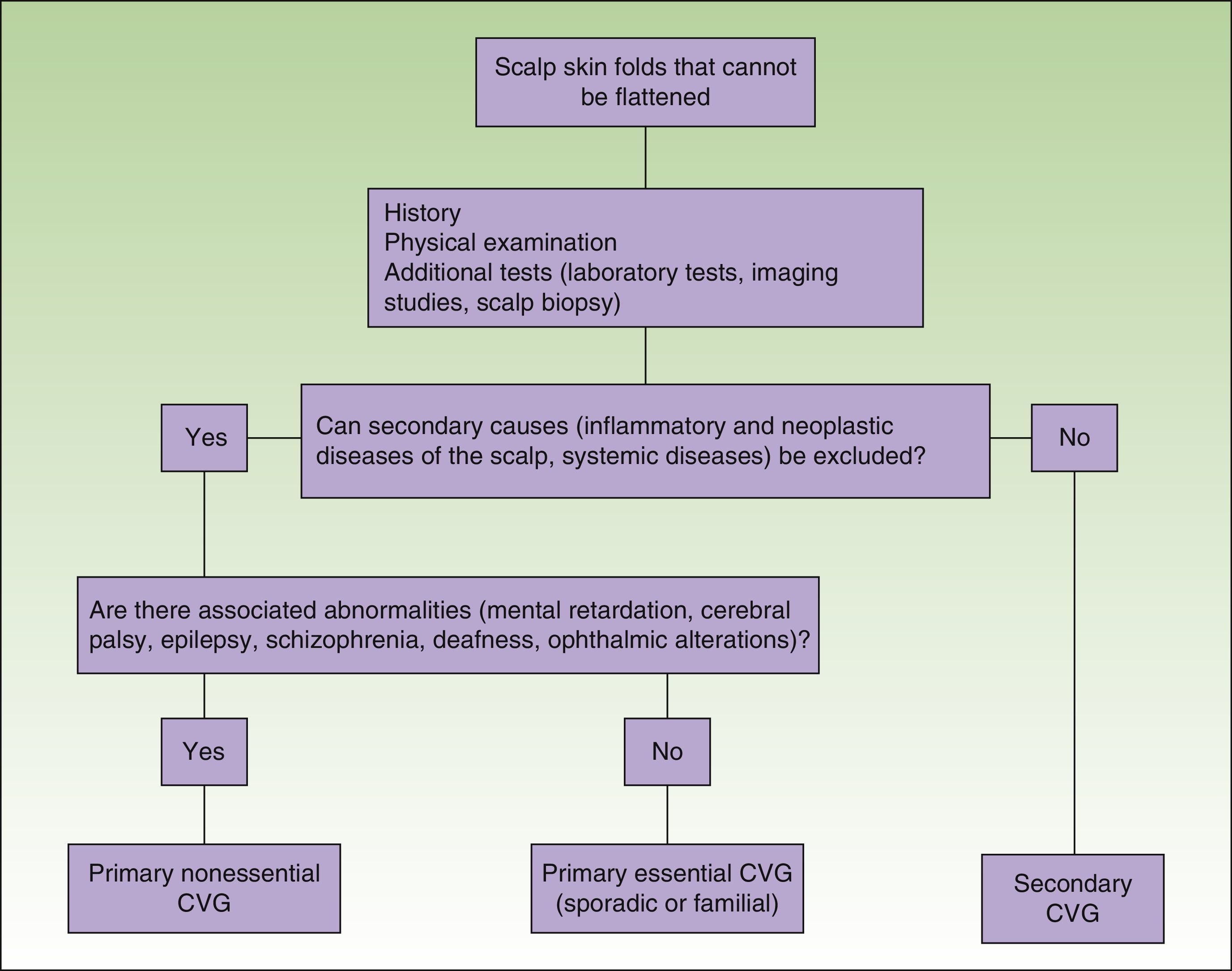
The primary essential form is not associated with other abnormalities, in contrast to the primary nonessential form, which can be associated with mental retardation, cerebral palsy, epilepsy, schizophrenia, deafness, and cranial and ophthalmologic abnormalities.6 The secondary forms of CVG can be associated with numerous underlying diseases, such as pachydermoperiostosis, acromegaly, cutis laxa, cylindroma, cerebriform intradermal nevus, amyloidosis, myxedema, syphilis, intracranial aneurysms, intraventricular ependymoma, and inflammatory conditions of the scalp; exclusion of these associations is therefore important (Fig. 3).7,8
Primary CVG affects the scalp, particularly at the vertex and in the occipital region. The folds usually run symmetrically in an anterior-posterior direction, although they can be transverse in the occipital region. The number of folds varies between 2 and 12, and they cannot be corrected by pressure or traction.4
The additional tests to be performed will depend on the clinical presentation and on any associated disease. Imaging studies such as magnetic resonance imaging or CT must be performed when neurologic or ophthalmologic abnormalities or mental retardation are present, although some authors recommend routinely performing these studies to exclude structural cerebral alterations.9 Scalp biopsy enables us to exclude other underlying causes, such as cerebriform intradermal nevus, cylindroma, and inflammatory dermatoses of the scalp. In the primary forms, histopathology is normal in the majority of cases, although thickening of the dermis and hypertrophy of the pilosebaceous units have been reported.10
CVG is a progressive disease and, in its primary essential form, only affects the scalp; surgery is therefore only considered in cases with major psychological repercussions.11
In summary, we have presented a case of familial primary essential CVG. Primary essential CVG is a rare entity, especially in its familial form, with only 1 other familial case described, also with clinical manifestation arising in adolescence.4 In these cases it is still important to exclude causes of secondary CVG as well as diseases associated with the primary nonessential form.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Suh H, Flórez-Menéndez Á, de La Torre-Fraga C. Forma familiar de cutis verticis gyrata primario esencial. Actas Dermosifiliogr. 2016;107:435–437.