The literature on peristomal pyoderma gangrenosum (PPD) is scarce, and studies to date have included few patients. It is therefore difficult to determine the incidence of PPD, investigate risk factors, or evaluate the effectiveness of the different treatments available. We report on a series of 4 patients diagnosed with PPD at our hospital in 2013 and 2014, and review the clinical characteristics and responses to treatment. Three of the patients had inflammatory bowel disease and 1 had rectal cancer. Three patients responded favorably to initial treatment with 0.1% tacrolimus ointment (administered as monotherapy in 2 cases and combined with immunosuppressants in the other). However, on withdrawal of tacrolimus, the disease recurred in all 3 patients, requiring treatment reintroduction or modification.
La literatura del pioderma gangrenoso periestomal (PGP) es escasa, y las series publicadas tienen un número de pacientes limitado. En dicho contexto es difícil determinar la frecuencia de la enfermedad, así como sus factores de riesgo, y valorar la eficacia de los distintos tratamientos disponibles. Presentamos una serie de casos de PGP diagnosticados en nuestro centro entre los años 2013 y 2014 y revisamos las características clínicas y la respuesta terapéutica. Se incluyeron un total de 4 pacientes, 3 de los cuales estaban diagnosticados de enfermedad inflamatoria intestinal, mientras que uno de los casos se asoció a carcinoma de recto. Tres pacientes presentaron evolución favorable tras el tratamiento inicial con tacrolimus 0,1% en pomada (2 casos en monoterapia y uno asociado a otros inmunosupresores), con recurrencia en todos ellos tras la suspensión del tratamiento precisando reintroducción o cambio de tratamiento.
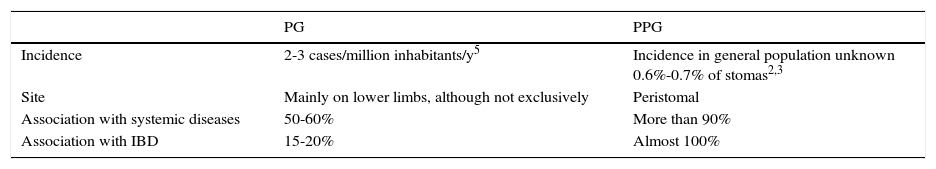
Peristomal pyoderma gangrenosum (PPG) is one of the most uncommon subtypes of pyoderma gangrenosum, accounting for 15% of all cases of pyoderma gangrenosum.1 Its characteristics enable it to be differentiated from other types (Table 1). Almost 100% of cases of PPG are associated with inflammatory bowel disease (IBD), although not exclusively,1,2 whereas pyoderma gangrenosum is associated with IBD in 15%-20% of cases.2
Differences Between Pyoderma Gangrenosum and Peristomal Pyoderma Gangrenosum.
| PG | PPG | |
|---|---|---|
| Incidence | 2-3 cases/million inhabitants/y5 | Incidence in general population unknown 0.6%-0.7% of stomas2,3 |
| Site | Mainly on lower limbs, although not exclusively | Peristomal |
| Association with systemic diseases | 50-60% | More than 90% |
| Association with IBD | 15-20% | Almost 100% |
Abbreviations: IBD, inflammatory bowel disease; PG, pyoderma gangrenosum; PPG, peristomal pyoderma gangrenosum.
The literature on PPG is scarce, and studies to date have included few patients.1 Therefore, it is difficult to determine the incidence of the disease and its risk factors and to evaluate the effectiveness of the various treatment options.2 We present the clinical characteristics and response to therapy of a series of 4 cases of PPG.
Material and MethodsWe performed a retrospective observational study of all cases of PPG diagnosed based on clinical and histopathology findings at our hospital during 2013-14. We excluded all dubious cases and cases for which no biopsy evidence was available. After reviewing the clinical histories, we recorded the following variables: sex, body mass index (BMI), age, underlying disease, activity of the underlying disease, type of surgery, treatment, and response to treatment.
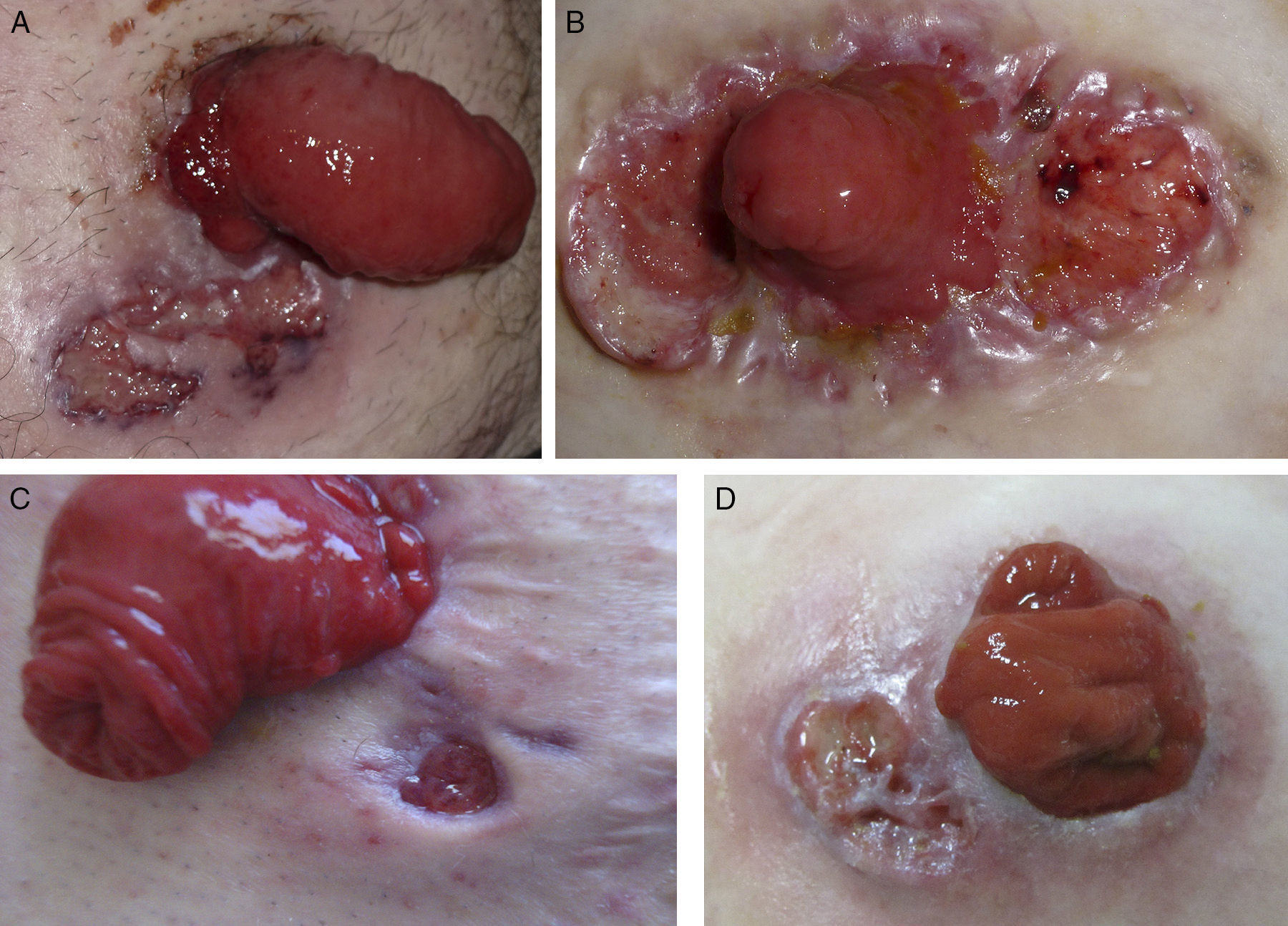
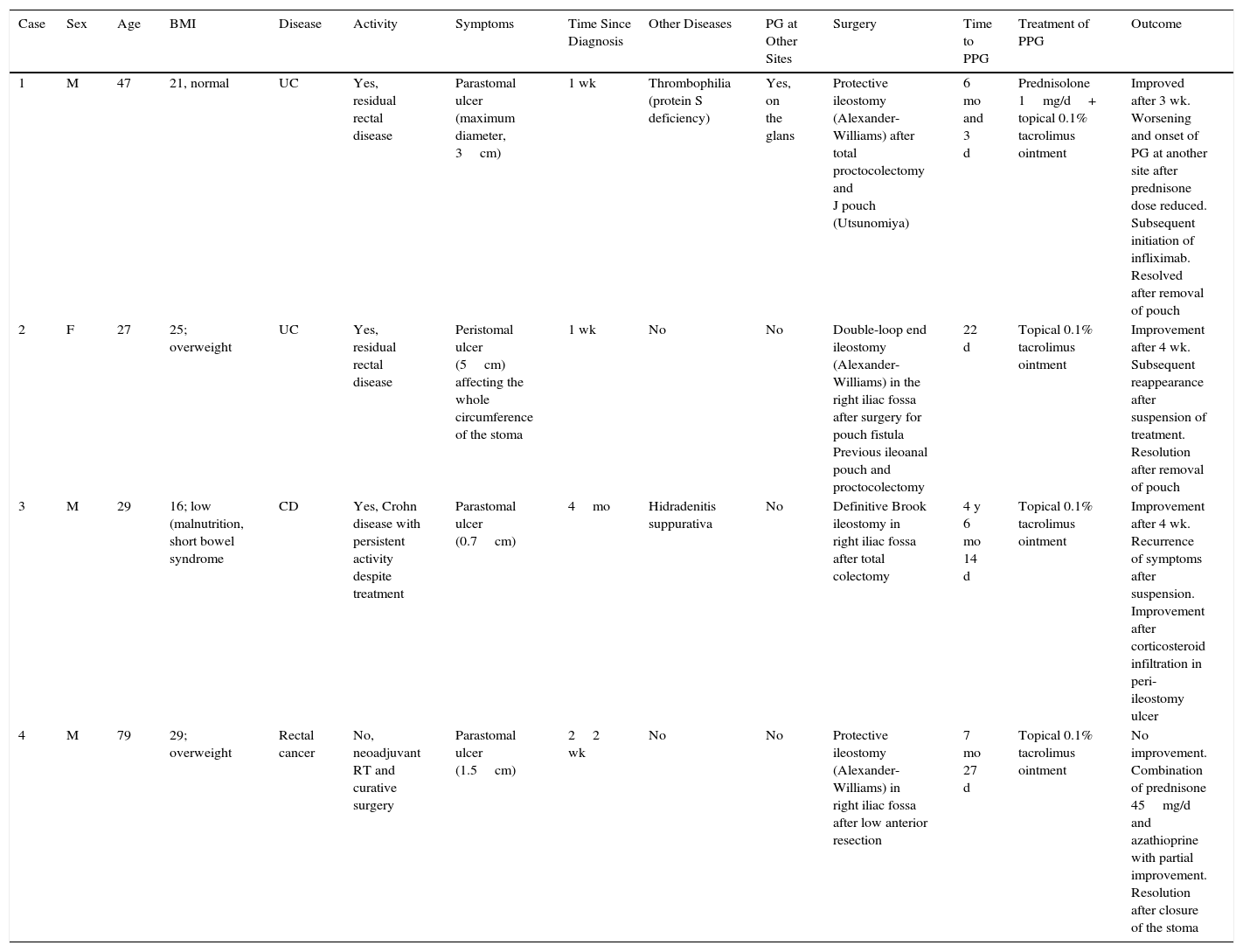
ResultsThe study population comprised 4 patients (3 men and 1 woman) aged between 27 and 79 years (Fig. 1A-D), whose characteristics are included in Table 2. Three of the 4 patients had IBD (ulcerative colitis in 2 cases and Crohn disease in 1 case); 1 patient had rectal carcinoma, although this was not associated with IBD. Time from surgery to onset of PPG varied from 22 days to more than 4 years. Outcome was favorable in 3 patients after initial treatment with 0.1% tacrolimus ointment (monotherapy in 2 cases and combination with other immunosuppressive agents in 1 case). The disease recurred after suspension of treatment, which had to be reintroduced or switched.
Clinical images. A, Case 1. Parastomal ulcer (maximum diameter, 3cm) with violaceous edges and cribriform scarring in a man aged 47 years with ulcerative colitis. B, Case 2. Peristomal ulcer (diameter, 5cm) with raised and violaceous edges in a woman aged 27 years with ulcerative colitis. C, Case 3. Small parastomal ulcer with punched out edges that first appeared 4 months previously in man aged 29 years with Crohn disease. D, Case 4. Parastomal ulcer (diameter, 2cm) with a fibrin-covered base in a man aged 79 years diagnosed with rectal carcinoma.
Series of Patients with PPG: Clinical Characteristics and Treatment.
| Case | Sex | Age | BMI | Disease | Activity | Symptoms | Time Since Diagnosis | Other Diseases | PG at Other Sites | Surgery | Time to PPG | Treatment of PPG | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 47 | 21, normal | UC | Yes, residual rectal disease | Parastomal ulcer (maximum diameter, 3cm) | 1 wk | Thrombophilia (protein S deficiency) | Yes, on the glans | Protective ileostomy (Alexander-Williams) after total proctocolectomy and J pouch (Utsunomiya) | 6 mo and 3 d | Prednisolone 1mg/d+ topical 0.1% tacrolimus ointment | Improved after 3 wk. Worsening and onset of PG at another site after prednisone dose reduced. Subsequent initiation of infliximab. Resolved after removal of pouch |
| 2 | F | 27 | 25; overweight | UC | Yes, residual rectal disease | Peristomal ulcer (5cm) affecting the whole circumference of the stoma | 1 wk | No | No | Double-loop end ileostomy (Alexander-Williams) in the right iliac fossa after surgery for pouch fistula Previous ileoanal pouch and proctocolectomy | 22 d | Topical 0.1% tacrolimus ointment | Improvement after 4 wk. Subsequent reappearance after suspension of treatment. Resolution after removal of pouch |
| 3 | M | 29 | 16; low (malnutrition, short bowel syndrome | CD | Yes, Crohn disease with persistent activity despite treatment | Parastomal ulcer (0.7cm) | 4mo | Hidradenitis suppurativa | No | Definitive Brook ileostomy in right iliac fossa after total colectomy | 4 y 6 mo 14 d | Topical 0.1% tacrolimus ointment | Improvement after 4 wk. Recurrence of symptoms after suspension. Improvement after corticosteroid infiltration in peri-ileostomy ulcer |
| 4 | M | 79 | 29; overweight | Rectal cancer | No, neoadjuvant RT and curative surgery | Parastomal ulcer (1.5cm) | 22 wk | No | No | Protective ileostomy (Alexander-Williams) in right iliac fossa after low anterior resection | 7 mo 27 d | Topical 0.1% tacrolimus ointment | No improvement. Combination of prednisone 45mg/d and azathioprine with partial improvement. Resolution after closure of the stoma |
Abbreviations: CD, Crohn disease; F, female; M, male; PG, pyoderma gangrenosum; PGP, peristomal pyoderma gangrenosum; RT, radiation therapy.
The incidence of PGP seems to have increased during recent years.1 PGP is observed in approximately 2%-4% of patients with IBD who undergo intestinal surgery with stomas and in 0.6% of patients who undergo surgery with ostomy.1–3 PPG is almost always associated with IBD, although there have been reports of isolated cases associated with cancer, diverticulitis, neurologic dysfunction, monoclonal gammopathy, and collagen disease.1,4 In the present series, only 1 case was associated with rectal carcinoma, whereas the remainder were due to underlying IBD.
Most studies highlight the greater incidence of PPG in patients with Crohn disease than in those with ulcerative colitis,2 although this finding seems to have been called into question in recent years.1 Some authors explain the greater incidence of PPG in patients with Crohn disease by the more common indication of surgery for this condition, which requires partial resection of the intestine. In patients with ulcerative colitis who require surgery, on the other hand, the usual approach is total colectomy, which results in definitive cure of the disease.2 Only 1 patient in the present series was diagnosed with ulcerative colitis, whereas 2 of those with Crohn disease had undergone total colectomy with conservation of the rectum in order to create an ileoanal pouch. Both had pouchitis (disease activity in this section of the colonic mucosa). Other authors have also suggested the presence of residual activity in the rectum as a risk factor for PPG in patients with ulcerative colitis.2 The current trend in surgery is to perform reconstructive techniques with ileoanal pouches in order to avoid permanent ileostomy, and this may play a role in the increased incidence of PPG in patients with ulcerative colitis.
In 2012, Wu et al.1 performed a study on risk factors for PPG in a series of 15 cases. The multivariate analysis revealed independent risk factors and statistically significant differences only for female sex, high BMI, and the association with autoimmune disease. Half of the patients in the present series were overweight, although none were obese. Patient 3 was underweight because of malnutrition owing to short bowel syndrome. We found no association with chronic inflammatory or autoimmune disease, except for the case of a patient with severe hidradenitis suppurativa, although this association is uncommon.5 In cases where pyoderma gangrenosum is associated with hidradenitis, each disease progresses independently of the other. However, the presence of common clinical findings and specific pathogenic mechanisms, as well as the response to treatment with anti–tumor necrosis factor agents in both conditions, leads us to believe that this association is not completely casual, even though its mechanisms are not well known.5 The triad of pyoderma gangrenosum, hidradenitis, and severe acne was recently included in a new autoinflammatory syndrome known as pyoderma gangrenosum, acne, and suppurative hidradenitis syndrome,6 which shares some features with pyogenic arthritis, pyoderma gangrenosum, and acne syndrome.
Management of PPG is difficult, and no treatment of choice is available.2 Both topical and systemic approaches have been used. Initially, topical treatments seem to be the most widely used, although they are subject to complications in areas where stomas have been created, since they hamper adherence of bags and dressings, which require frequent changing, thus potentially leading to microtrauma and worsening of PPG. Tacrolimus seems to have significant benefits in PPG resistant to topical corticosteroids.7 The only clinical trial that has compared topical tacrolimus with beclomethasone showed that topical 0.3% tacrolimus was more effective, especially in large PPG lesions.7 Other cases of a good response to topical tacrolimus have been reported.8,9 In the present series, we observed an initial improvement in 3 of the 4 patients, 2 of whom had been treated with monotherapy, whereas the remainder received combination treatment with oral corticosteroids owing to the associated gastrointestinal symptoms. The patient with a poorer response to therapy was the only one whose PPG was not associated with underlying IBD but was secondary to cancer.
Treatment of PPG is controversial. Reinsertion of stomas at other sites leads to recurrence of PPG at the new site in almost all patients1,2 and is therefore not indicated. Most articles report a cure rate of 100% for PPG after closure of the stoma,2 as in patient 4 in the present series. In patients with residual rectal disease after colectomy with ileoanal pouch, removal of the pouch can sometimes improve PPG,2 as observed in patients 1 and 2.
ConclusionsWe conclude that a high degree of suspicion is necessary in the face of any lesion in the peristomal area in order to ensure an early diagnosis of PPG. The most closely associated risk factors are IBD and its activity, female sex, high BMI, and association with other autoimmune diseases. Treatment should be selected based on the number, size, and localization of PPG, as well as on the underlying disease. Tacrolimus ointment could prove useful as local treatment, especially in lesions that are resistant to corticosteroids.
Ethical DisclosuresProtection of Persons and AnimalsThe authors declare that no tests were carried out in humans or animals for the purposes of this study.
Confidentiality of DataThe authors declare that no private patient data appear in this article.
Right to Privacy and Informed ConsentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Turrión-Merino L, Hermosa-Zarza E, Miguel L, Muñoz-Zato E. Pioderma gangrenoso periestomal: presentación de 4 casos y revisión de los factores de riesgo y la respuesta terapéutica. Actas Dermosifiliogr. 2016;107:e13–e17.