Localized myxedema is a late manifestation of thyroid dermopathy, occurring mainly secondary to Graves disease. While the condition most commonly affects the pretibial region, it can also affect the upper limbs, neck, and face. It is usually self-limiting and may involve cosmetic or functional impairment. We report the case of a patient with thyroid dermopathy located on the hand that responded well to topical corticosteroids.
Case presentationA 64-year-old woman diagnosed with Graves disease consulted for a pruriginous lesion on the back of her left hand that had first appeared 2 months previously. The patient had a history of rheumatoid arthritis treated with sulfasalazine and leflunomide. Six years before consulting, she had received radioactive iodide for thyroid disease and was being treated with levothyroxine for iatrogenic hypothyroidism. She had also been in follow-up for pretibial myxedema for the last 3 years.
Physical examination revealed a slightly indurated erythematous–edematous plaque with diffuse borders affecting the anatomical snuff box and the metacarpal region of the second and third finger on the dorsum of the left hand (8cm×3.5cm, Fig. 1). The examination also revealed exophthalmos. The only finding of interest in the laboratory work-up was slightly increased serum thyroid-stimulating hormone values.
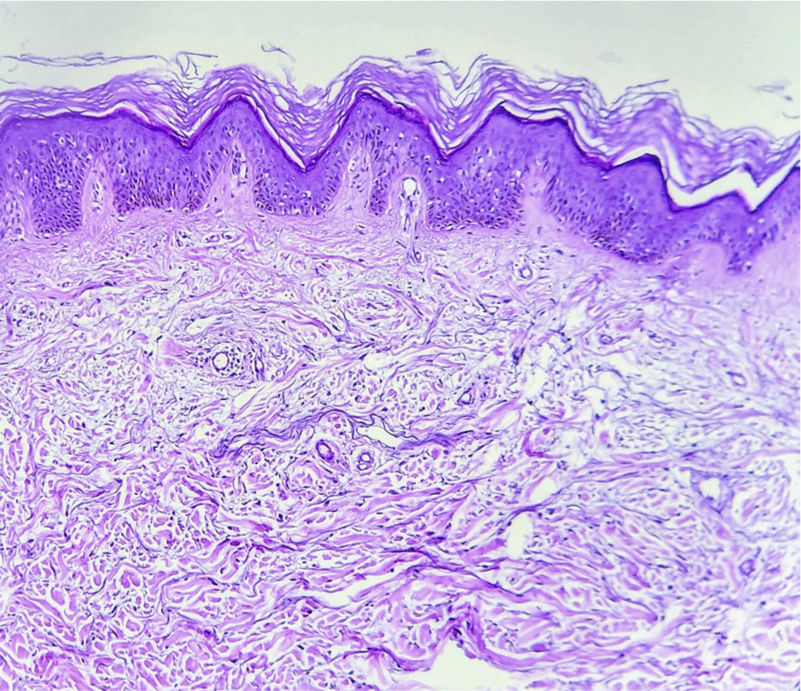
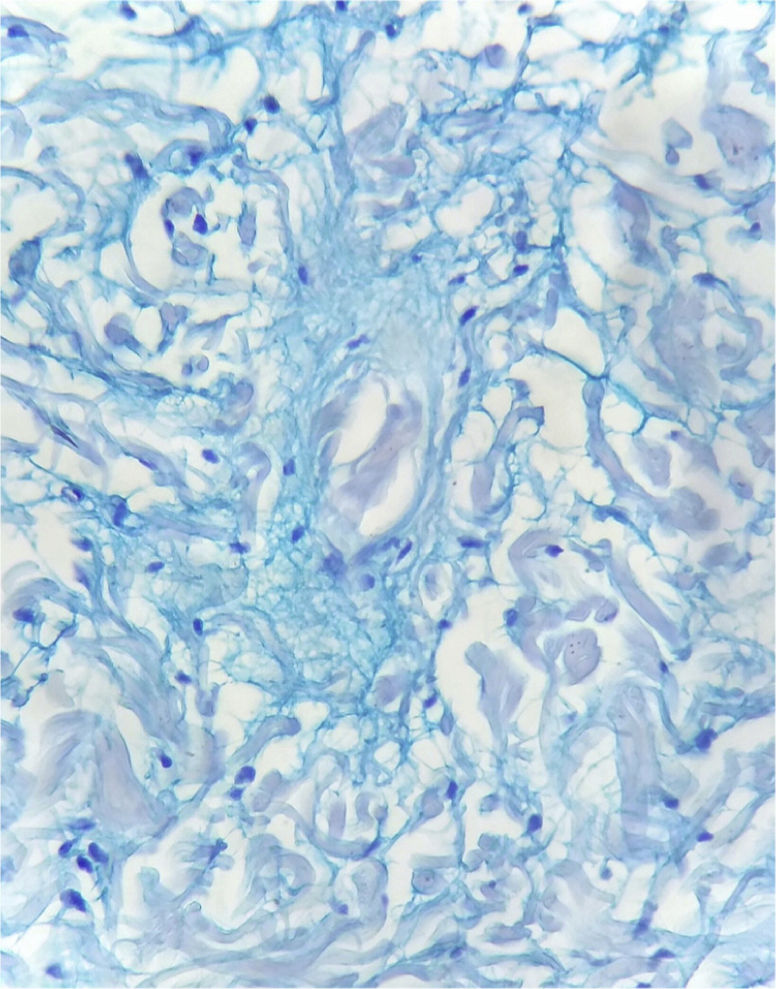
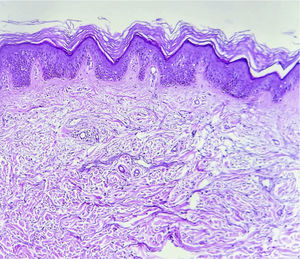
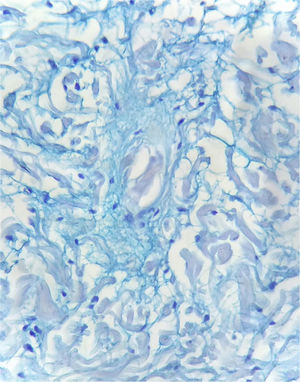
Histopathology of the skin biopsy specimen revealed basket-weave orthokeratosis in the epidermis (compact in some areas) and acanthosis-papillomatosis (Fig. 2). Alcian blue staining revealed mucin deposits between the collagen bundles in the dermis and a scant perivascular mononuclear inflammatory infiltrate that was compatible with myxedema (Fig. 3).
The lesion was treated with clobetasol cream under an occlusive dressing. It had improved clinically 1 month later, with improvement in edema and accompanying pruritis.
DiscussionThe term myxedema (myxo: mucus) was first used in 1877 by Ord, who believed that the cutaneous manifestations of thyroid diseases were due to excessive mucus formation in the subcutaneous tissue.1
Thyroid dermopathy is a type of cutaneous mucinosis that affects the dermis.2 While the standard term is pretibial myxedema, it seems more appropriate to use the term thyroid dermopathy, since it can affect other areas.
This condition is a late manifestation of Graves disease and affects less than 5% of patients.3 It has been reported in patients with other thyroid disorders such as hypothyroidism secondary to treatment of Graves disease (see above), Hashimoto thyroiditis, and, albeit less frequently, in patients with a healthy thyroid function.4,5
Thyroid dermopathy is the second most frequent extrathyroidal manifestation (the first is ophthalmopathy) and tends to affect women in the sixth decade of life.6
While the pathophysiology is unknown, various mechanisms have been postulated to explain the clinical manifestations. The most widely accepted is the presence of antibodies against thyroid-stimulating hormone receptors that act on the activation of fibroblasts. The participation of insulin-like growth factor type 1 (IGFR1) has also been reported. IGFR1 leads to an increase in the production of glycosaminoglycans in the dermis and, consequently, their deposition in tissue and subsequent formation of edema.5–7
Thyroid dermopathy takes the form of plaques and/or generally bilateral nonpitting edema. It can vary in terms of coloring, from erythematous and erythematous–violaceous to flesh tone with a translucid appearance. It is waxy in appearance and indurated on palpation, with accentuation of the hair follicles, leading it to resemble orange peel. The condition may be associated with pruritus and more commonly affects the lower limbs (pretibial myxedema), although, as in the case we report, it can compromise other regions, such as the upper limbs, face, and even scar tissue.6–8
In most cases, these manifestations are asymptomatic or mild and self-limiting, resolving in a few months or years. Their main drawback is cosmetic impairment, although they may also lead to functional compromise and local malaise.7
Histopathology may reveal separation of collagen fibers in the dermis owing to mucin deposits, which are clearly visible with specific stains such as Alcian blue and colloidal iron. A perivascular lymphocytic infiltrate and mastocytes may also be seen. In more advanced cases, we can observe papillomatosis, acanthosis, and hyperkeratosis.
The question of whether a return to normal thyroid values improves the skin lesions remains open to debate, since no supporting evidence for this hypothesis has been reported.2
If the decision is taken to treat the lesion, for either cosmetic reasons or the presence of functional abnormality, the treatment of choice is medium- to high-potency topical corticosteroids under an occlusive dressing.9
Alternative treatments have been proposed, although some have not been standardized and are based on small case series or free papers. They include systemic or intralesional corticosteroids, intralesional octreotide, intravenous immunoglobulin, plasmapheresis, isotretinoin, and even surgical resection.10
The interest in the presentation of this condition lies in the uncommon topography of thyroid dermopathy, which progresses well and responds favorably to topical treatment.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Drs. G. Poppi and C. Chiappe of the Histopathology Department of our hospital for their help with the histology findings and for providing the skin biopsy images.